13 Ways to Help Residents Sleep Normally
13 Ways to Help Residents Sleep Normally
Author: Mark Parkinson RPh: President AFC CE
Credit Hours 4- Approximate time required: 240 min.
Educational Goal:
To provide Adult Foster Care providers with information that will help them understand and manage their residents sleeping patterns.
Educational Objectives:
- Explain the anatomy and physiology of normal sleep patterns.
- Teach 13 techniques (caregiver tools) that help ensure healthy sleeping behaviors.
- Provide the definition of common sleep terminology
- List medication that effect sleep and tell of their effect and side effects.
Procedure:
1. Read the course materials. 2. Click on exam portal [Take Exam]. 3. If you have not done so yet fill in Register form (username must be the name you want on your CE certificate). 4. Log in 5. Take exam. 6. Click on [Show Results] when done and follow the instructions that appear. 7. A score of 70% or better is considered passing and a Certificate of Completion will be generated for your records.
Disclaimer
The information presented in this activity is not meant to serve as a guideline for patient management. All procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this article should not be used by care providers without evaluation of their patients’ Doctor. Some conditions and possible contraindications may be of concern. All applicable manufacturers’ product information should be reviewed before use. The author and publisher of this continuing education program have made all reasonable efforts to ensure that all information contained herein is accurate in accordance with the latest available scientific knowledge at the time of acceptance for publication. Nutritional products discussed are not intended for the diagnosis, treatment, cure, or prevention of any disease.
13 Ways to Help Residents Sleep Normally
 |
In-Home Caregiving Challenge
One of the most difficult aspects of living with the patients you take care of is when your residents have difficulty sleeping. Those who don’t work and live in a care home don’t know how hard it is on caregivers to have a patient who won’t or can’t go to sleep. You can’t appreciate how stressful it is until you are the one who has to stay up with the patient and go without sleep for days on end.
 When a resident of the home has chronic sleeping issues, it disrupts the entire home. It’s bad for the patient, it disrupts the sleep of the other residents, and it saps the strength, patience, and morale of the caregiver. It creates a stressful environment that is just plainly unpleasant to live in. Unlike other health professionals who get to leave there troubling patients behind and go home for the night, in-home caregivers never get to leave their work and escape the pressures of the patient who stays up.
When a resident of the home has chronic sleeping issues, it disrupts the entire home. It’s bad for the patient, it disrupts the sleep of the other residents, and it saps the strength, patience, and morale of the caregiver. It creates a stressful environment that is just plainly unpleasant to live in. Unlike other health professionals who get to leave there troubling patients behind and go home for the night, in-home caregivers never get to leave their work and escape the pressures of the patient who stays up.
So what is a tired caregiver to do? All too often they call up the doctor and demand some “knock-out pills”. But have you noticed that sleeping pills don’t always make the problem go away? Or they help for a few days but then the problem returns. Have you noticed how reluctant some doctors are to hand out the really strong stuff? I have noticed that, too. Sleeping is a very complicated issue. Medications have their place in therapy, but they're limited to what they can do. There are other things that caregivers can do to help their residents get to sleep.
Managing sleeplessness in a care home is a much more complicated than it first appears. As a pharmacist, I can tell you that there is no magic pill for this problem. The purpose of this article is give the caregiver a better understanding of sleep and tell you about 12 caregiver tools that I think will help you better manage the situation when it arises. To use the tools effectively, caregivers first better understand sleep.
Sleep
Just exactly what is sleep? What happens when we nod off? After decades of research, we really don’t know for sure. There are so many individual factors and so many aspects of our lives that affect the way we sleep that it makes understanding sleep behaviors difficult. Variability in behaviors and individual sleeping patterns force us to think of the subject in broader, more general terms.
Sleep - definition:
“In animals, sleep is a naturally recurring state characterized by altered consciousness, relatively inhibited sensory activity, and inhibition of nearly all voluntary muscles. It is distinguished from wakefulness by a decreased ability to react to stimuli, and it is more easily reversible than being in hibernation or a coma.” Wikipedia 2015
Confusing, isn’t it? It turns out that sleep is more complicated than just closing our eyes. There are a lot of details involved in going to sleep and staying asleep. Fortunately sleep researchers have figured out a few of those details. Let’s start with the big picture. Despite all the variability in human behavior, there are basic patterns to our sleep. Researchers have found that those patterns are greatly influenced by two interacting body systems: 1 - The internal biological clock and 2 - The sleep/wake homeostatic workings of our body.
Our inner clock
 |
The internal biological clock according to the National Institute of Health NIH is “The biological clocks that control circadian rhythms are groupings of interacting molecules in cells throughout the body. A ‘master clock’ in the brain coordinates all the body clocks so that they are in synch.” That master clock is a group of nerve cells located in the hypothalamus of the brain and is called the suprachiasmatic nucleus. I wish I could be more informative, but the biological clock is extremely intricate. It involves a multitude of cells, possibly all the cells scattered throughout the body. There are multiple genes and proteins in those cells involved, and more details and facts are still being discovered and understood. So for now it is enough to know that we have an internal clock ticking out the timing of our sleep.
Homeostasis the Self-regulating System
The sleep/wake homeostasis is the biochemical system that regulates the body’s internal functioning. This is the workings of the body that strive to maintain a certain pattern of behavior. It is influenced by feedback loops and operates without conscious direction from us. It responds to external stimulus, especially changes in light and darkness, and tries to keep sleeping patterns the same. This system creates the sleep/awake drive or pressure to awake or fall asleep. Everyone has experienced the sleep/wake homeostasis working when they try to stay up. The longer we stay up the more chemicals build up that put us to sleep. When we sleep, those chemicals are cleared and others start to build up that wake us up. Again I wish I could write more, but we still don’t know enough. The hormones adenosine, melatonin, and cortisol are major players in the system.
Along with other factors this creates in our bodies a physical response called the circadian rhythm. It is roughly a 24-hour cycle of bodily function and behavior that gives us our regular sleep intervals. Our circadian sleep cycle involves more than just falling asleep and waking up. There are dips in the daytime toward sleeping and moments of going toward wakefulness at night that occur on a fairly regular basis. When these dips and peaks occur is very individualistic and contribute to being a “morning person or a night owl.” They are also subject to environmental and behavioral influence so we can consciously alter the patterns somewhat. It is also important to note that our circadian rhythm naturally changes over our life time. The following graph shows how much sleep is usually required for varying ages.
|
Age and Condition |
Sleep Needs |
|
Newborns (0–2 months) |
12 to 18 hours |
|
Infants (3–11 months) |
14 to 15 hours |
|
Toddlers (1–3 years) |
12 to 14 hours |
|
Preschoolers (3–5 years) |
11 to 13 hours |
|
School-age children (5–10 years) |
10 to 11 hours |
|
Adolescents (10–17 years) |
8.5 to 9.25 hours |
|
Adults, including elderly |
7 to 9 hours |
Source http://en.wikipedia.org/wiki/Sleep
Two important facts for caregivers to note is: 1. the amount of sleep for the elderly doesn’t decrease as we age (even though it may become more difficult to achieve at times) 2. Adolescents still need more sleep than adults.
For those of you who take care of teenagers, it may not seem like they need more sleep because they always want to stay up at night. Sleep researchers have found out that the normal circadian rhythm sleep time for teenagers shifts toward later in the evening. It turns out that the average teenager sleep cycle puts them to sleep about 11:00 p.m. and wakes them up about 8 or 9 a.m. That might be a moot point because today’s society dictates other behaviors like getting to go to school on time. But it does help to explain certain behaviors that arise and may be helpful in your caregiving.
Caregiver Tool One- What Is Interfering?
The bottom line to all this is we are biologically programmed to sleep in a regular pattern. When events occur that change our sleep behavior, our bodies strive to get back to our normal sleep patterns. This brings us to the first caregiver tool about sleep. It is the “what is interfering tool.” This is a patient, investigative attitude toward sleep problems. Instead of reaching for a sleeping pill, the caregiver should figure out what is interfering with the normal sleep pattern then try to control the interference and patiently wait for the normal sleep pattern to reassert itself. More about this later. ****
This new attitude requires more patience and caregiver fortitude, but it does tend to permanently resolve sleep problems better than pills. Generally sleeping pills just masks the true problem. This might also help you understand why some doctors are reluctant to issue the strong stuff. They want to figure out and fix the underlying cause of the sleeplessness and just not tape over it with a sleeping pill Band Aid.
I know how frustrating that response can be when you’re very tired. I’ve been there. The solution is to understand what the doctor is trying to do and communicate effectively with them. Reassure the doctor that this is just a short- term request so that you can sleep and function better as a caregiver. Tell them if you get your sleep, you can better assist them in figuring out what is actually interfering with the normal sleep pattern. Hopefully by the end of the article, you will be better prepared to do that. Let me assure you I am not asking you to become a doctor. What I am saying is you will become the eyes and ears of the doctor. You can ask questions, observe the patient, and report facts. Let everyone know that you are part of the caregiving team and you’re ready to cooperate and get to work solving the sleep problem.
Every field of scientific study has its own terminology. A few terms that will help you to communicate more effectively are:
- Endogenous - Naturally produced by the body itself
- Jet lag - When your body’s clock is different than your wrist watch
- Quiescence - Being at rest, quiet, still, inactive, or motionless
- Sleep debt- The effect of not getting enough sleep
- Sleep drive- The body’s pressure to fall asleep
- Sleep inertia - Feeling of grogginess immediately following an abrupt awakening
- Sleep latency - Length of time it takes to accomplish the transition from full wakefulness to sleep
Medical terminology can be boring so we’ll break it up into smaller bite size portions. More sleep terms will come later.
What Is Involved in Sleep?
It’s easy to think of sleep as a quiet time when not much happens. But in many ways, the opposite is true. Sleep is a busy time for the body and mind. Ironically, even though we are unconscious, the brain remains very active. Using an electroencephalograph (EEG), which measures brain wave activity and observes eye movement underneath closed eye lids, researchers have observed a pattern of two distinct stages of sleep, non-REM and REM (rapid eye movement) sleep. The mind cycles through these stages approximately every 90 minutes.
Non-REM: In non-rem, as the name implies, eye movement is slow or very still and brain waves, as recorded on an EEG, go through three phases of distinct wave patterns, N1- N2 and N3. N1 is when we first start to nod off. N2 is when brain wave patterns start to slow down, interspersed with bursts of activity called sleep spindles. N3 is the time of the deepest sleep. N3 have also been called “deep” or “slow wave sleep.”
Source http://healthysleep.med.harvard.edu/healthy/science/what/sleep-patterns-rem-nrem
REM, on the other hand, is characterized by rapid eye movement and small fast brain waves. It is believed to be the time of the most intense dreams. The arms and legs become paralyzed to prevent the body from acting out the dreams. Some researchers call the REM sleep phase active sleep.
Source http://healthysleep.med.harvard.edu/healthy/science/what/sleep-patterns-rem-nrem
Non-REM and REM phases continue to cycle throughout the period of sleep. At first, non-REM dominates most of the time. It is thought to be a time of physical repair and replenishment. Later, REM sleep becomes lengthier, signaling that the brain is becoming more active. From my descriptions, it may seem that there is a regular pattern of sleep but that is just generally so. Many things can affect sleep cycles, and patterns change throughout our life. For example, in infants, non-REM dominates when the needs of a growing body are greatest. Later in life, REM time lengthens as one might expect because the demands on our minds is greater. Physical repair demands, length of sleep, naps, environmental changes, habits, drugs, and alcohol use can all change sleep patterns. Some changes affect non-REM while others affect REM more. We can temporarily go with less of either, yet we still need the right amount of both sleep phases over time. As we go without sleep or rely on a sleeping tablet, a sleep debt starts to build up and homeostatic pressures start to change the way we sleep. You can now begin to appreciate just how complicated sleep can be and understand that there is no one pill for insomnia. You can also understand how sleep cures can sometimes only work for a short time. The bottom line is that there are some predictable patterns to sleep but they are fluid, individualistic, and dependent on many factors.
This brings us to my next caregiving tool
Caregiver Tool Two “Copy Cat.”
When a new resident moves into your home, they come with a preset sleep pattern that the body fights to maintain, despite the new surroundings. It’s going to take a while to reset the resident’s sleep pattern to fit in your home’s environment. There will be those who can make the adjustment by themselves (hopefully everyone), but there are those who will need help or at least they will need your patience as their body makes new sleep patterns. One way you can help make this transition easier is to find out what sleeping arrangements the new resident had previously. Did they sleep with a night light? Was the room cool or hot? Did they have a bedtime rituals. Which pictures on the wall and what items around the bed are they used to falling asleep with and waking up to. Since habits and the environment play a big role in sleep patterns, copying what you can from the new resident’s former surroundings can make the transition to a new sleep pattern a lot easier. Temporary use of sleeping pills can also help with the transition, but they can also slow down the natural resetting of the sleep cycle process if the resident becomes dependent on the pills to get to sleep.
The Need to Sleep
Science hasn’t figured out all the reasons why we sleep yet but it is clear that we need to sleep. Sleep is a time for restoration, renewal, and repair, but interestingly it is not a uniform process. Some aspects of repair and renewal dominate at different times in the sleep cycle.
Physical repair and renewal is more likely to occur is deep, slow-wave, non-rem sleep, while psychological repair and renewal is associated more with REM or active sleep. In fact, REM brain wave patterns look very similar to waking brain waves. It is thought to be a time where the old noggin’s file cabinet is cleaned up after the day’s activity, so to speak.
On average, a typical healthy adult sleeps for eight hours. Each sleep cycle lasts for approximately 90 minutes. If you do the math that means there are five periods of repair. At first physical repair dominates and REM sleep time is reduced. As the night wears on, REM sleep becomes lengthier and psychological repair is thought to start to dominate. This helps explain why we have the most vivid dreams early in the morning before we wake up.
The needs of the body and the mind greatly influence our sleep patterns. For example, when an infant sleeps, the body has little damage to repair, but it has a lot of new experiences to process. As one could expect, babies spend all of their time in REM sleep. As we get older, our bodies need more and more repairs so in adults, non-REM sleep dominates. But if we have mentally stressful times, psychological repair and renewal take up more sleep time, leaving less time for needed physical repairs. Thus it has been discovered that stress robs the body of needed time to repair and replenish itself as more and more sleep time is taken up by stress-processing REM sleep. As you already know, go without deep sleep and you’re more likely to get sick. Recent studies indicate that inadequate sleep is also a factor in developing obesity and diabetes. The more we go without adequate sleep, the less repair and renewal happens, which naturally leads to a painful, fatigued body. The more sleep we go without, the more we have thinking and memory difficulties. That sounds very familiar to any tired and grumpy caregiver watching over a tired and grumpier resident.
Pharmacist Medication Alert
Sleeping pills promote drowsiness, but they do not promote deep sleep or REM sleep. In fact, they can interfere with it. I have seen cases where a patient took  sleeping pills and a full eight hours of sleep occurred, but the patient still woke up tired and restless. Taking more sleeping pills doesn’t seem to help and the patient can get quite frustrated. Hum, sounds like the patient was using the wrong Band Aid over the owwie, so to speak.
sleeping pills and a full eight hours of sleep occurred, but the patient still woke up tired and restless. Taking more sleeping pills doesn’t seem to help and the patient can get quite frustrated. Hum, sounds like the patient was using the wrong Band Aid over the owwie, so to speak.
What Is Going Wrong and Caregiver Myths
Sleep may be influenced by endogenous forces, but these forces are also under partial conscious control. We can choose to ignore the sleep impulses and stay up or stay in bed whenever we feel like it. This has led to a caregiving myth that residents can choose to cooperate with house rules about sleep anytime it is demanded of them by the caregiver. When the residents don’t comply, the caregiver all too often jumps right into another myth and thinks “let’s just make them cooperate by knocking them out with a sleeping pill.”
The resident’s ability to choose to cooperate with home rules about sleep is only partially true. Residents are subject to the inner workings of the body just like we all are. If a resident is not cooperating, there is usually a physical component only partially under conscious control that is going wrong. Change in sleep patterns usually is not caused by an uncooperative attitude but by something else. That’s both insomnia and wanting to sleep all the time. Those occurrences should be a giant red flag to the caregiver signaling that something else is wrong and needs looking into.
As I said earlier, I am not asking you to become a doctor and cure the patient. In-home caregivers play the other important roles of patient caretaker and advocate. Your job is to observe report and demand action. You best serve your residents when you keep the rest of the care team on their toes while at the same time giving them the necessary information about the patient.
What Are You Looking For, Information Gathering
It has always been my advice for care providers to communicate effectively with doctors. After all, the more information the doctors have, the better decisions they make. It also helps your reputation in the help care community to be prepared before you send the patient in. Send a copy of your records with the patient along with your observations of the resident’s behavior concerning sleep. You can make up your own or use the third caregiver tool - “sleep assessment.” You have my permission to copy any or all of this for your own use.
Caregiver Tool Three- Sleep Assessment
_______________________________________________________________________________________________________________
Sleep Assessment
What are the sleep difficulties?
How many times per week does the patient experience them?
When does the resident take a nap(s?)
What do you think is causing the problem?
1. Patient thoughts
2. Caregiver thoughts
Is there anything you've done in the past that has helped the resident sleep?
Does the resident lay awake, feeling anxious or worrying?
How long has the resident had trouble sleeping?
Has the patient had trouble sleeping in the past?
Has there been any major changes (a move, a new job, new illness, new medication, emotional changes)?
Have there been any stressful circumstances in the resident’s life recently (financial troubles, death of a loved one, family issues)?
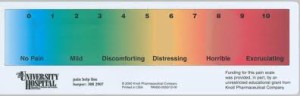
What is the level of the resident’s pain, if any?
(less pain) 0, 1, 2, 3, 4, 5, 6, 7, 8, 9, 10 (most pain)
Does the resident snore? How loudly?
Are there any uncomfortable feelings in the legs (a creepy crawly feeling)?
What are the bedtime symptoms observed or reported?
Sweating ____ Sleep talking or walking or screams___ Nightmares ____
Restlessness ____ Coughing____ Teeth grinding____ Wets bed_____
Stops breathing____ Gasps for breath____ Heartburn ____
Kicking or twitching____
Is there troubles going back to sleep once awake?
How often does the resident get up to go to the bathroom?
Does the resident resist going to bed?
Does the resident fall asleep during the day?
Does the resident feel refreshed after a night’s sleep?
____________________________________________________________________________________________________
Diagnosis and Difficulties
 Once the doctor has enough information, he or she will try to diagnose the problem first then figure out the cure. The current prevalent thinking about sleep problems is to consider short-term therapies first and prescribe accordingly. If the problem is a chronic or reoccurring one, the diagnosis will be much more difficult. It will take a while longer to figure out what’s going wrong. Don’t be surprised if in these cases the prescriber is more reluctant to hand out the strong stuff. There are so many issues that can cause sleep problems, and some sleep- inducing pills will only mask the real problem. It might even take a referral to a sleep specialist or a psychiatrist to figure it out. If that is the case, then you have the issue of who pays for the specialist. Medical insurances may not be very cooperative. It has been my experience that if someone shouts long and loud enough, insurance companies will buckle.
Once the doctor has enough information, he or she will try to diagnose the problem first then figure out the cure. The current prevalent thinking about sleep problems is to consider short-term therapies first and prescribe accordingly. If the problem is a chronic or reoccurring one, the diagnosis will be much more difficult. It will take a while longer to figure out what’s going wrong. Don’t be surprised if in these cases the prescriber is more reluctant to hand out the strong stuff. There are so many issues that can cause sleep problems, and some sleep- inducing pills will only mask the real problem. It might even take a referral to a sleep specialist or a psychiatrist to figure it out. If that is the case, then you have the issue of who pays for the specialist. Medical insurances may not be very cooperative. It has been my experience that if someone shouts long and loud enough, insurance companies will buckle.
Caregiver Tool Four- More Medical Terminology
Insomnia- Insomnia is a general term for sleeplessness. In most cases, the term is used to describe a symptom not the main problem so we need more medical terminology to be clear about the subject. Using the right words correctly garners greater respect and more cooperation from others.
- Primary Insomnia - Insomnia not directly caused by other health conditions (sleep disorder).
- Secondary Insomnia – Sleep problems occur because of other health concerns (interference with sleep).
- Chronic Insomnia - Insomnia that occurs at least three times a week for a month or longer
- Parasomnias - A disorder characterized by abnormal or unusual behavior of the nervous system during sleep (all the abnormal things that happen while you sleep, like sleep walking)
It will help you to understand what the doctor is going to do if you ask the doctor if he or she thinks the insomnia is primary or secondary, acute or chronic. Whatever the diagnosis is, understanding the medical terminology will give you clues of what is happening. You will be better prepared to cooperate and it will make your job easier. If you don’t know a word, look it up and research it.
Primary insomnia is just a fancy way of saying that the doctor can’t see any illness that is causing the issue, so maybe insomnia is the problem by itself. Most cases of insomnia will be secondary insomnia, though. Something else is interfering with normal sleep patterns. There are so many things that can interrupt sleep like stress, anxiety, pain, depression, alcohol, poor sleeping habits, and infections like UTIs. Even that stupid dog at the end of the street that barks all night. It is also correct to think of insomnia when you wake up too many times at night or get up too early in the morning. Here are a few things for the caregiver to consider and watch for in insomnia cases.
Pain - Pain causes insomnia, and in return insomnia feeds the pain monster. Chronic pain management goes a long way in solving sleep issues, and a good night’s sleep can help chronic pain. A good place to start is assessing the pain level by asking the resident to describe the pain on a scale of 1-10, 10 being the highest. Keep track of how it changes over time. Report these findings to the doctor.
|
|
Sleep Apnea - Sleep apnea occurs when the upper airway becomes blocked and it becomes difficult to breathe. That wakes the patient up anytime it happens. Sleep apnea is something that caregivers can observe and report. Loud snoring can be a warning sign, and obesity is a contributing factor to sleep apnea.
Other breathing problems - Other breathing problems can interfere with sleep like asthma, COPD, and allergies. If the resident is known to have these issues then a CPAP or oxygen mask will be of more use than sleeping pills. Obviously if coughing at night is an issue, report it to the doctor. If you use oxygen and the cough continues, ask the patient about GERD symptoms like sour stomach, acidity taste in mouth, burning throat, and heartburn. When the resident lies down at night, stomach acid flows easier into the throat. Even small irritations can cause coughing. Report these finding to the doctor as well. GERD can often be overlooked in children, so those who take care of teens might be on the lookout. Obesity is also a factor in GERD.
Restless leg syndrome - Restless leg syndrome is a nervous system disorder where there is discomfort in the legs and feet. It prompts the sufferer to move around to find relief. The feeling often peaks at night, hindering to sleep or waking the resident up. Caregivers can ask the resident if they feel a creepy crawly feeling in their legs or feet. Restless leg syndrome becomes more common with age.
Parkinson’s disease - Parkinson’s disease is a disorder of the central nervous system that affects muscle movement. It can cause tremors (shaking), rigidity (stiffness), slowness of movement, and balance problems. It can also cause insomnia and restless leg syndrome. Parkinson’s is a progressive disease that can’t be cured, just managed. The quicker the diagnosis is, the more effective the management can be. This is a case where caregivers, as patient advocates, can see the red flags and ask the right questions. You’re not making a diagnosis; you’re just planting the idea about the possibility of sleeplessness being a symptom of a much more serious illness.
 UTIs - Urinary tract infections are easier to contract when the immune system is weaker. This happens more often as we age, have diabetes, or other like events. The urge to pee becomes stronger and more frequent, which naturally will wake a person up. But it also for some reason makes the infirm elderly act very contrary and uncooperative about sleep when they are tired. Many times in my careers as a caregiver and a pharmacist UTIs were first recognized because of the contrarian sleep behavior. This is one of the best examples I can think of where prescribing a sleeping pill was the wrong thing to do.
UTIs - Urinary tract infections are easier to contract when the immune system is weaker. This happens more often as we age, have diabetes, or other like events. The urge to pee becomes stronger and more frequent, which naturally will wake a person up. But it also for some reason makes the infirm elderly act very contrary and uncooperative about sleep when they are tired. Many times in my careers as a caregiver and a pharmacist UTIs were first recognized because of the contrarian sleep behavior. This is one of the best examples I can think of where prescribing a sleeping pill was the wrong thing to do.
Depression - Clinical depression is more than just feeling blue. There is a chemical imbalance or the inner workings of the brain are not up to snuff. The inability to sleep isn’t always a factor in mental health problems, but it is a major consideration in any most cases and should be always reported by the caregiver.
Dementia and Alzheimer’s – Brain-deteriorating diseases can affect the sleep control centers of the brain. They can also dramatically increase the stress felt by the sufferer. Sleep issues tend to be more chronic in such cases. Caregivers would be helped considerably if they developed contingency sleep plans with the aid of the doctor before they become a problem. One tragic irony of these conditions is that the more powerful sleeping pills can add to the patient’s confusion and dementia. Such events can turn into a downward spiral leading to turning the patient into a drugged-out zombie. Chemical restraint is not what sleeping pills should be used for. Anti-anxiety medication might be an alternative that will break the downward cycle and enable a normal sleep cycle to come through. Anti-anxiety meds take longer to kick in, so timing before bedtime will take some skill.
Sundown syndrome- Sundown syndrome is more of a laymen’s term for when a patient becomes confused and agitated toward the hour of sleep. It is usually seen in dementia cases but can also be seen in uncontrolled diabetes and people with poor hearing or eye sight. For caregivers, such agitation couldn’t come at a worse time. The caregiver is tired and the patient is tired. Other medical professionals have gone home and are for the most part out of reach. Even getting sleeping pills down an agitated resident can be an effort.
The main challenge to caregivers is that the patient is agitated and confused, not exactly cooperative states of mind. The following are caregiver tools five, six, seven, and eight that can be especially helpful in sundowners.
 |
Caregiver Tool Five - Relaxation techniques (Part one)
 Control the agitation by using calm responses. Don’t argue even if the resident wants to. Calm the environment (calm music or a recording of ocean waves or a forest stream). A calming five-minute hand massage might help. Agree with the patient’s perception of reality then divert them away from anxiety- causing issues. The idea is to work on the environmental factors and thought processes that are making the agitation worse. More about relaxation techniques later.
Control the agitation by using calm responses. Don’t argue even if the resident wants to. Calm the environment (calm music or a recording of ocean waves or a forest stream). A calming five-minute hand massage might help. Agree with the patient’s perception of reality then divert them away from anxiety- causing issues. The idea is to work on the environmental factors and thought processes that are making the agitation worse. More about relaxation techniques later.
Caregiver Tool Six – Full-spectrum florescent lamp
Sometimes the problem is that the body’s clock has been thrown off. According to Caring.com, “Researchers have also found that placing a full-spectrum fluorescent lamp (between 2,500 and 5,000 lux) about 1 meter from the person suffering from sundown syndrome and within his visual field for a couple of hours in the morning can work wonders at getting his biological clock back on track and making him less agitated at sundown.” If you’re going to try this, get the doctor to sign off because this might be considered therapy. Of course a walk in the sunshine also exposes the resident to full-spectrum light and doesn’t require a doctor’s order.
Caregiver Tool Seven - The reality check
Eyesight and hearing can be powerful stimuli for the tired, confused mind. I had a case where the patient started to have hallucinations. His eyesight was failing, and the only thing he could see was shadows. When he got tired, his concentration wandered. When he saw the shadows flickering in his field of vision, his mind tried to fill in the blanks and created hallucinations that seemed real. It was quite upsetting to him. The solution was a reality check. I reminded him that he couldn’t see clearly, so if he saw a clear image he would know that it was not real. I also read a story of a caregiver who told the patient to poke the hallucination with his cane and see what happened. Naturally nothing happened, and the patient was able to calm himself down. The trick here is to give the patient the reality check tools so they can calm themselves down.
Caregiver Tool Eight- The Snack Trick
If you can’t get the resident to cooperate in taking pills, put them into chocolate pudding or applesauce. The texture and colors hide the pills well. Use a little stealth when giving the snack or you’ll blow the whole trick. Use this trick with caution and skill because a patient has a right to refuse medication. On the other hand sundown syndrome, the resident’s ability to even make a choice is greatly impaired. Some experts consider this not a refusal of medication but just a general instinctual non-cooperative reaction. When in doubt, get a doctor’s orders to cover yourself or take the patient to the hospital where they can worry about administering the right sleep medication.
Understanding the Drugs
 |
It may seem that I am anti-sleeping pills. That is just not the case. Used with skill, they can be very helpful. But they are not the cure all that some caregivers think. A quick discussion of some of the more common medications might help with the skill part. Consider this caregiver tool nine.
Caregiver Tool Nine - Being a Proficient Pill Popper
Medications are a big part of modern medicine. As part of the health care team and as a paid professional, it is your responsibility to use the drugs as prescribed AND monitor for effect. Your job doesn’t stop when the pill enters the mouth. It is also your job to see if the drugs are doing what they are supposed to do and if any bothersome side effects crop up. You are then obligated to pass the info on to the doctor. If the doctor doesn’t hear from you, he assumes that everything is hunky dory.
For example, the doctor gives the patient a new blood pressure pill, and a few days later the patient starts to fall asleep during the day. The resident then gets their days and nights mixed up. They stay up, and the caregiver has to stay up. You call the doctor for sleeping pills. How about monitoring and reporting on the new B/P pills and avoid the sleeping problem in the first place? The bottom line is to read the information from the pharmacy that comes with the pills. Then watch for both the effect and side effects. Communicate what you observe and expect action to be taken. The sleepiness side effect big-three drug categories are narcotic pain killers, mental health drugs, and cold remedies.
Drugs for Sleep
Sedative/sleeping pill medical terminology
Anxiolytics= Anti-anxiety meds= stress pills= tranquillizers
Hypnotics = Sleep inducers = sleeping pills
When considering what to do about insomnia problems, doctors have many options. There are far too many to write about each one, so I’ll explain as a group in their drug classes.
Hypnotics
Hypnotics are true sleeping pills, a group of psychoactive drugs whose main purpose is to induce sleep. The most powerful ones are used in surgeries. Most hypnotics work by increasing the activity of the mind’s neurochemicals that induce sleep. That creates a problem, though. As you know, sleep is much more than falling unconscious. It is a whole cycle of activities, collectively called the sleep architecture. If you have a drug that constantly works on just a part of the cycle, it will interfere with the rest of the sleep phases. Longer acting sleep inducers blunt deep sleep non-REM so they actually mess up the normal sleep architecture. Ironic isn’t it, sleeping pills that interfere with sleep. That might explain a few things that you have probably observed. For example, residents waking up tired after a full night’s sleep, or sundown syndrome that repeats day after day despite the use of sleep inducers. Think of sleep inducers as just the start button to the sleep cycle.
Non-Benzodiazepines
These are the newer sleeping pills whose main feature is that they wear off quickly. The idea is to induce sleep then get out of the way of the normal sleep architecture. Caregivers should know that even though this class of drug will help put a resident to sleep, it will not keep them asleep. That’s an important detail to know, isn’t it?
The drug names to watch for are:
• Zolpidem (Ambien, AmbienCR)
• Zaleplon (Sonota)
• Lunesta eszopiclone
• Rozerem ramelteon
Ambien CR or controlled-release zolidem is a bit different than the rest. It has two parts. It has the fast-acting part that wears off like the others in this class. It also has a controlled-release portion that leaks out over time to induce sleep later on. It’s supposed to help keep people asleep all night long. On the surface that sounds perfect, except you know now that there is still the sleep architecture problem.
Rozerem works at different sites than the rest. It has less chance for causing addiction and abuse and rebound insomnia. Some doctors don’t think that it is as powerful as the other hypnotics or are familiar enough with its use to prescribe it.
These drugs where meant to be a fix for short-term insomnia, not long- term cures. There is evidence that long-term use creates dependency (more about that later). Other problems that crop up are sleep walking and sleep eating, daytime anxiety, and increased chance of depression. There is even some links to increased cancer risks. Caregivers should not use these meds as a shortcut to make their long-term job easier because in many ways they won’t.
Anxiolytics
Anti-anxiety medication works by stimulating inhibitory neurotransmitter chemicals. In laymen’s terms, it slows down certain brain functions. Originally developed as an anti-anxiety drug, over the years they have been developed for other uses including muscle relaxer, anticonvulsant, tranquillizer, and sleeping pill. Doctors often find them useful to help people fall asleep and treat the underlying cause of the insomnia, such as anxiety and worry issues that disrupt falling asleep.
The main class of anxiolytic drugs in use today is the benzodiazepines.
Benzodiazepines
There are short, intermediate, and long-acting drugs in this class. Short and intermediate are the ones most commonly used for sleep alone. They have been largely replaced in this role by the non-benzodiazepines primarily because they have fewer side effect issues. Of prime concern for caregivers is that the resident becomes groggy and is more apt to fall. Excessive daytime sleeping can occur and rebound insomnia has been known to happen.
You might recognize a few of these drugs:
• diazepam (Valium)
• temazepam (Restoril)
• clonazepam (Klonopin)
• triazolam (Halcion)
• lorazepam (Ativan)
• alprazolam (Xanax)
Since these medications could be used throughout the day, their effect on sleep patterns should be monitored. Other medications that cause drowsiness like pain killers could compound the issue and really mess up the sleep cycle.
Antihistamines
Histamine is a very important chemical our body uses to control a wide variety of functions. There are specialized histamine receptors all through the body, each controlling different functions including immune responses, digestion, and mental alertness. Antihistamines stops histamine from working in its normal function. There are different kinds of antihistamines that work at different sites in the body, but there is always some bleed over into other histamine systems. Thus antihistamines used for allergic reactions (stopping the immune response) have a side effect of sleep (stopping the wake/alertness function). The higher the dose, the greater the side effect, up to a certain point. At some point all the histamine receptor sites are blocked, so more will have no more sleepiness effect. Of course it doesn’t stop there. Anywhere histamine has a function will be affected by antihistamine use. For several reasons as we age we become even more susceptible to the other effects of antihistamines. It is a surprisingly complex system that is affected by an over-the-counter medication.
The antihistamines used in OTC sleep pills are:
Diphenhydramine
Doxyalmine
For caregivers in residential care homes what this boils down to is a tradeoff. Sleep verses the side effects of antihistamines. Of course if you’re not looking for the side effects, you’re going to end up running around in circles chasing one adverse reaction to another. Watch for and report the following occurrences to the doctor. Then follow up by asking the doctor if antihistamine use is an issue in these cases.
Next day drowsiness and fatigue, dizziness, impaired thinking and memory, agitation, hallucinations, dry mouth, constipation, urinary retention, dry eyes, blurred vision, and hot flushing. Some children and the elderly are wired backwards and may experience excitation and agitation, just the opposite of sleep. Many of these side effects look exactly like dementia. It is hard to tell the difference between the two or if the antihistamines are making the dementia more severe. Another irony, sleeping pills used to help with sundowners may be making the sundown syndrome worse.
Have patience with the doctor. They will have difficulty discerning what is really going on, too. If the doctor does make a change, be patient while the resident adjusts to the new routine. There will be some sleepless nights for sure, but there is a good chance that they will go away and normal sleep will return. It’s a judgment call on what you can tolerate and what is best for the resident, sleeplessness or side effects.
Other drugs
The length of this sleeping pill list might be acting like a sleep inducer to the reader, but we’re not done yet. There are three more commonly used drug categories to talk about.
Melatonin
Melatonin is a hormone that helps regulate the circadian rhythm of the body. It is produced by the pineal gland as environmental light becomes less. It is just one of the chemicals used to help make us drowsy. It is not a very powerful sleep inducer so it is mainly used to help keep the circadian rhythm in its proper place. In normal doses it is OK for long-term use, but it just won’t help in all cases of insomnia.
Herbals
Herbals are a tricky area of medicine. They have been around forever, but they aren’t scientifically studied as much as prescription drugs. It’s hard to tell between what is true and what are old wives tales. There is also a problem of potency and consistency of effect. It is an unregulated area of medicine so its buyer beware. Changing brands can have a big difference in effect. If you find something that works, it’s best to stick with that brand. Side effects and long- term use of herbals are also gray areas. Make no mistake. They are therapy so they must be reported to and controlled by the doctor in care home settings. If you’re lucky enough to have a doctor who is skilled in their use, they can be useful alternatives in difficult situations. It won’t hurt to ask the doctor about their use.
• Valerian
• Chamomile
• Kava Kava
• Lemon Balm
• Passion Flower
• St. John Wart
• Lavender
Secondary insomnia drugs
As you recall, secondary insomnia is sleeplessness caused by other illnesses. When a doctor uses a drug that treats the underlying causes of insomnia, they are by default using them as a sleeping pill. Mental health medications that have a drowsiness side effect are often used as sleeping pills.
Some examples are:
• Trazadone (anti-depressant)
• Risperidone -Risperdal (anti-psychotic)
• Doxepin –Sinequan (anti-depressant)
• Amitriptyline –Elavil (anti-depressant)
It may seem that this complicates medication management, but it really doesn’t change the basic caregiver skill of monitoring for all effects and side effects. If things get a bit confusing to you, just ask the plain questions of the doctor. What is this medication being used for? Is it also for sleep? What effects and side effects do you want me to watch for and report back to you on?
Other Caregiver Issues
Dependence
A hidden danger in all long-term sleep therapies is the issue of dependence, which is defined as the state of relying on or being controlled by something else. Those insomnia sufferers who use drugs long term to fall asleep start to lose the ability to naturally fall asleep. If they attempt to fall asleep without the medication, they experience rebound insomnia, which leads them to go right back on the sleeping pills. The longer they are on the drugs, the more chance that their bodies will develop a tolerance to them and it will require more to achieve the same affect. You might have noticed the drug-dependent resident saying things like “my sleeping pills just don’t work like they used to,” or “these aren’t as potent as the ones I use to take.” Drug tolerance can even be seen in OTC antihistamines. The result is the resident takes more medication, which increases the chance for harmful side effects.
Stronger prescription sleeping pills also can be addicting. All of the hypnotics except Rozerem and many of the anxiolytic drugs carry this warning. Addiction is a complex issue and is a topic for another time. The short version is those addicted take the medication for how it makes them feel or to avoid withdrawal symptoms more than just falling asleep. Caregivers should note and report any of the following signs.
• Euphoria/happiness after taking the pills
• The resident seems to be compelled to take the pills, they become desperate.
• The resident finds it hard to cope with life without the pills.
• Loss of interest in other things
• Deterioration of personal hygiene and grooming
• Defensiveness about drug use
• Other bodily aches and complaints crop up without the drug
My advice is to not stress over who’s addicted and who’s not. There are ways to deal with the issue if it shows up. The goal is to have all your residents sleeping as naturally as circumstances will allow. A concerted effort on your part in drug and sleep management will solve almost any addiction problem without too much extra effort. The heart of these efforts will be to work with the doctor to gradually reduce the dosages and increase other efforts to induce sleep. The body will over time make the adjustments back to being normal, which incidentally is the same cure for dependence on sleeping pills.
Another real issue for caregivers is sleeping pills increase the risk of falling. It just goes with the entire drug class. Sleeping pills make a person less alert and groggy, making it easier for people to fall. In addition there is also a loss of coordination and balance that compounds the issue.
As a professional caregiver you should be able to manage this risk by:
• Having the resident go to bed after they take the pills, especially with the hypnotics which begin to work very quickly.
• Make the bedroom slip and trip hazard free.
• Keep the path to the bathroom clear and well lit.
• A commode by the bed can be very helpful.
• Help the resident get up in the morning, especially if they use antihistamines to sleep. They tend to make a person groggy for a long time, making the resident a bit of a drugged-out zombie in the morning. Being there in the morning prevents falls.
Prescriber reluctance
Sometimes doctors don’t cooperate as well as you would like in handing out sleeping pills. They know the problems of sleeping pills better then you do. But they may not know about how care homes operate and need to be educated.
If a doctor is reluctant to prescribe sleeping pills, it may help reduce some of their concerns by telling them of your fall-prevention efforts and medication- management techniques.
Ask the doctor about their major concerns and assure them that you will monitor the patient and report any of them if they occur.
Tell the doctor that care homes do not work in shifts. You are there all the time and you need sleep as well to give proper care to the patient.
Contraindications
Contraindications are conditions where it would be very dangerous to use sleeping pills. Caregivers and prescribers would have to take a very, very long look before using sleeping pills.
• Breathing problems - Many sleeping medications tend to reduce respiration. If there are breathing problems already present (sleep apnea, COPD, asthma), taking sleeping pills may become life threatening.
• Sleep walking - If a resident has sleep walking tendencies, sleeping pills may make it worse. If you observe sleep walking, talking, or other activities, report them to the doctor. The resident is not in their right mind and they may get hurt.
• Daytime agitation - Some people are wired backwards. What should put them to sleep winds them up instead. Watch for an increase in day time agitation. It might be tied to the sleep medication.
• Pregnancy - It doesn’t happen very often in care homes, but if a resident is pregnant, sleeping pills can harm the developing baby.
Final words on drugs
Sleeping pills can be very useful in managing insomnia, but they are just one tool in the caregiver tool box. They are not even the ultimate tool or the tool of last resort. Drugs are not the cure-all that many think. They must be considered as just a part of the overall care strategy to manage sleep.
More about this Later****
At the beginning of this article I told you about the first caregiver tool “What is Interfering,” and told you I would tell you more later. Well… it’s later so let’s get to it. The rest of these caregiver tools are based on the principle that a body wants to sleep until something interferes with its natural sleep processes. The core of these principles is to remove obstacles first then if needed, seek additional medical help. These are not PRN therapies but an ongoing effort of good caregiving techniques that reduce or eliminate insomnia causes before they become a major problem. These will also have an impact on new move-ins and help ease their transition into your home.
Caregiver Tool Ten - Bedroom Environment
Your home is your work place. Just like any business you have to optimize the work place to give the best business outcomes. Bedroom design is not the first thing a caregiver may think about when it comes to insomnia, but it is something that has to be thought out carefully.
The ultimate goal of bedroom design is to create a sanctuary from the world. A place of peace and relaxation in which all you have to do is walk in and feel calm and comfortable.
 •Dim the lights at hour of sleep to reinforce the circadian rhythms of the body. Night lights only when sleeping, including hall and bathroom lights.
•Dim the lights at hour of sleep to reinforce the circadian rhythms of the body. Night lights only when sleeping, including hall and bathroom lights.
- Choose neutral wall colors. Have plenty of personal, familiar objects on the wall and near the bed. Keep the place neat and orderly.
- Commode placement can keep a person in bed, but be careful not to cause a trip hazard. Bedrails can be easily installed in any bed. Bedrails can cause more problems than they solve. They must be used with skill. Having doctor’s orders for their use always keeps you out of trouble.
- Cool the room temperature. Our bodies sleep better when it’s cool. The National Sleep Foundation recommends 67.0F to get the best sleep. If the room is slightly cool, the resident will less likely want to get out of a nice warm bed.
- Studies have shown that we like fresh and clean sheets and pillow cases. The “feel” of the bed is very important. If the resident can bring their own bed into your home, it will be more comfortable. For most cases that won’t happen, but at least have them bring their own pillow if it’s available.
- Reduce noises in and outside of the bedroom. If that’s impossible, white noise devices can really help. Fans turned on in the corner can create enough noise to drown out sleep-disruptive sounds.
- Surround the residents with pleasant smells. Scents can have a powerful influence on the subconscious mind. Studies have shown that lavender promotes sleep.
Caregiver Tool Eleven - Sleep Hygiene
Sleep hygiene is the behaviors and habits that make up sleep-promoting practices. They are the recommendations made by sleep professionals for their clients. Most are common-sense type stuff, but you’d be surprised how often they are forgotten by insomnia sufferers. When one of your residents has insomnia, this list is the first place to look for signs of troubles.
- Fix a bedtime and an awakening time. If times float too much, the body’s clock gets confused.
- Avoid too much daytime napping. This can be problematic for elderly. It is well worth the effort of caregivers to keep track of such things. It is much easier to keep a person awake during the day with activities and interactions than to fight with them to get to sleep at night.
- Light management. The optic nerve is a powerful sleep regulator. Get plenty of light during the day (especially in the morning) and reduce it at night. Opening and closing the curtains can go a long ways in good sleep hygiene.
- Avoid alcohol four - six hours before bed. I know this is not a problem in care homes. I included it in this article because of the myth of the nightcap. A drink can relax you, but as the body metabolizes, the alcohol it creates substances and conditions that will actually wake a person up. No booze before bed.
- Avoid stimulants four - six hours before bed. That means caffeine in any drinks, coffee, tea, and sodas. Have the medications residents take before bed evaluated by your pharmacist to see if they can interfere with sleep. Pass on to the doctor any important information you find.
- Control food intake. If a resident is hungry, a light snack can settle down a noisy stomach. Also a tasty treat can be quite diverting to an overly anxious mind. Large amounts of chocolate may cause trouble. Avoid heavy, spicy, or overly surgery foods. Calming herbal teas can be quite helpful. If you’re using them as therapy, get the doctor to sign off on their use. Some herbs can interfere with medications. Too much food will interfere with restful sleep.
- Exercise regularly, but not right before bed. A walk in the sunshine is the easiest and helps with the light exposure and napping issues. Stationary bikes and steppers are also helpful in care homes. Make it part of the daily routine and good habits will form.
- Reserve the bed for sleep only. You’re trying to train the subconscious mind that when the body feels the bed, it’s time to go to sleep. Provide other comfortable furniture in the bedroom for other activities like reading or watching TV.
- Establish a pre-sleep ritual that provides habitual clues for sleep. This should be easy for care homes. For example, announce, “It’s time for your bedtime snack,” “Go turn down your covers,” “Soak your dentures,” etc.
- Manage entertainment before sleep. TV programs are designed to grab your attention and keep it. Some programs can really get you stirred up. On the other hand, music can be quite calming. Relaxing music or environmental sounds can really help calm a resident before bedtime.
Caregiver Tool Twelve- Just in Case.
Keep an extra calming activity in your pocket, just in case. For example, a bedtime bath, a massage, a walk around the house, or apply lotion to limbs. The purpose of these activities is to divert the mind and calm the senses of an overly anxious insomniac. Use them sparingly or they will lose some of their power. If a particular activity always proves useful for a resident, you might consider making it part of the pre-sleep ritual.
Caregiver Tool Thirteen - Cognitive Behavioral Therapy (CBT)
CBT is psychotherapy whose goal is to change thought patterns that cause problems. For insomnia, it mostly offers education about sleep to target dysfunctional beliefs about sleep. In layman terms, it straightens out the thinking about sleep.
For example, if a resident believes that they will always wake up at 3 in the morning and then not be able to go back to sleep, it may turn into a self-fulfilling prophecy. A possible therapy would be: "Waking up early happens from time to time. But I might still get some sleep. And it's no big deal if I don't.”
This therapy is administered by trained mental health professionals so accessing it can be problematic for care homes. Mental health homes clients may be able to qualify for such therapy if pushed for by the caregiver as well as residents who have insurance programs like HMOs. An example is Kaiser Permanente. They have on staff-psychotherapists available with a referral from the patient’s doctor.
Relaxation Techniques – (Part two)
There is more to say about relaxation techniques. Now that you have a broader understanding of sleep principles, we can talk more about them. Anxiety and stress are sleep robbers. In fact, stressing over not being able to sleep compounds the problem. No matter how hard you try, you can’t think yourself to sleep. It has to happen naturally. The first step is to have the resident stop worrying and relax. Sometimes that’s easier said than done. A resident might need a little bit of caregiver support to start to relax.
Divert the resident’s thoughts away from anxiety-causing issues. If the resident is tossing around in bed worrying about not sleeping, the sleep experts suggest getting out of bed. It can divert the mind from stressing about not sleeping. Once relaxed, try going to bed again. Caregivers should always have peaceful, calm responses. Deep breathing can help residents relax. Tensing muscle groups then purposely relaxing them can also help as can exercising (taking a walk), heat, and massages.
There are more advanced relaxing techniques that can be taught by experts. They are progressive muscle relaxation (Jacobson’s), autogenic training, biofeedback, and imagery.
Sleep Specialists
There is an increasing number of sleep centers filled with specialists more than willing to help with difficult clients. The problem is who’s going to pay for them. In your role as a patient advocate, you might have to make some noise with the doctor and the insurance company to get the troubled residents to a sleep specialist.
Conclusion
There are many things a skilled caregiver can do to support good sleeping habits in their residents. The core principles to remember are:
- There are natural patterns to sleep and the body wants to sleep. If the resident can’t sleep, then something is getting in the way. Eliminate the “something,” and sleep will return on its own.
- Sleep medication can be very helpful in the short term, but they are not a cure-all for insomnia. There are many drug options. Some will not be sleeping pills but will have the same effect as they work on eliminating underlying causes of insomnia. All have to be used with skill, which includes the vital caregiver roles of monitoring for effect and side effects then communicating that information to the prescriber.
- Caregivers can greatly influence good sleeping habits. The constant application of caregivers sleep tools can go a long way in getting their residents to sleep and staying asleep. Controlling the sleep environment tends to provide more permanent sleep solutions than medications alone.
A brief review of the caregiver tools listed in this article.
Caregiver tool one - What is interfering?
The caregiver patiently investigates the cause of sleeplessness in order to solve the underlying problem. Start by asking the question what has changed?
Caregiver tool two - Copy cat
Everyone has certain sleep patterns but they are greatly influenced by the individual choices a resident makes. Copying what has worked in the past makes it easier to maintain good sleep patterns now.
Caregiver tool three - Sleep assessment
This is a questionnaire that helps you gather the right information to pass on to the doctor.
Caregiver tool four - Sleep medical terminology
Knowing sleep terms gives you power to communicate and understand better
Caregiver tool five - Relaxation techniques Part 1 and 2
Stress robs sleep. Relaxation promotes natural sleep. There are a number of things that a caregiver can do to get the resident to relax. They include calmly diverting attention, massage, music, calming environmental sounds, heat, baths, tensing then relaxing muscles, and deep breathing.
Caregiver tool six – Full-spectrum florescent light
Light influences the circadian rhythms of the body and a caregiver with the help of doctor instructions can use it to influence the resident into good sleeping patterns.
Caregiver tool seven - The reality check
Residents’ senses can fool them into believing that sleep-robbing events are occurring. Caregivers can help the residents see beyond those illusions and reduce their stress level.
Caregiver tool eight - The snack trick
If an anxiety-ridden client unrealistically refuses sleep medication, offering the medication in a snack can be diverting enough to get the medication down the over-stimulated patient. Useful in sundown syndrome.
Caregiver tool nine - Being a proficient pill popper
Drugs must be used with skill. In order to achieve the best outcomes, the caregiver should know the purpose(s) of the drug and monitor for effect and side effect. Then report finding to the doctor for action. Simply reading the literature that the pharmacy gives with each prescription can go a long way in becoming a proficient pill popper.
Caregiver tool ten – Bedroom design
Arrange and decorate bedroom to optimize sleep outcomes as much as possible. Pay attention to colors, lighting, furniture placement, temperatures and noise reduction.
Caregiver tool eleven- Sleep hygiene
Sleep hygiene are the good sleeping habits that caregivers should promote and maintain.
Caregiver tool twelve - Just in case
Always be ready with an extra calming activity. Use each infrequently to maintain its full diversional potential.
Caregiver tool thirteen - Cognitive behavioral therapy CBT
The “straightening out” of the sleep-robbing thoughts of a resident. To be applied by trained therapists.
Insomniacs cause sleep-deprived caregivers, which in turn causes poor caregiver care. It is an issue that every caregiver should be prepared to handle. Hopefully this article has helped.
As always, good luck in your caregiving efforts.
Mark Parkinson RPh
PS. May you have many many restfull nights and all your residents sleep like a ...........
References:
1. Dr. D. A. Williams and Dr. M. Carey. YOU REALLY NEED TO SLEEP: Several methods to improve your sleep. University of Michigan Health System 2003 http://www.med.umich.edu/painresearch/patients/Sleep.pdf
2. Michael Thorpy, MD. Sleep Hygiene. National Sleep Foundation.http://sleepfoundation.org/ask-the-expert/sleep-hygiene
3. Sleep Hygiene. University of Maryland Medical Center. July 31, 2013.http://umm.edu/programs/sleep/patients/sleep-hygiene
4. Sleep Hygiene. Wikipedia The Free Encyclopedia. Feb. 25,2015.http://en.wikipedia.org/wiki/Sleep_hygiene
5. Relaxation techniques and sleep hygiene for insomnia. PubMed Health. U.S. National Library of Medicine. Sept. 24, 2013 http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0004995/
6. Six Tips to Design the Ideal Bedroom for Sleep. National Sleep Foundation. http://sleepfoundation.org/sleep-news/six-tips-design-the-ideal-bedroom-sleep
7. D.T. Max. The Secrets of Sleep. National Geographic.com May 2010 http://ngm.nationalgeographic.com/2010/05/sleep/max-text
8. Aging and Sleep. National Sleep Foundation. Dec. 2009.http://sleepfoundation.org/sleep-topics/aging-and-sleep
9. W. Vaughn McCall, M.D., M.S. Sleep in the Elderly: Burden, Diagnosis, and Treatment. Prim Care Companion J Clin Psychiatry. 2004; 6(1): 9–20.http://www.ncbi.nlm.nih.gov/pmc/articles/PMC427621/
10. Angela Gentili, MD, Iqbal Ahmed, MBBS, FRCPsych (UK). Geriatric Sleep Disorder. Medscape Sept 23, 2014 http://emedicine.medscape.com/article/292498-overview
11. David N. Neubauer, M.D. Sleep Problems in the Elderly. American Family Physician. May 1, 1999. Am Fam Physician. 1999 May 1;59(9):2551-2558. http://www.aafp.org/afp/1999/0501/p2551.html
12. Aging changes in sleep. Medline Plus, National Institute of Health. Sept 3,2012 http://www.nlm.nih.gov/medlineplus/ency/article/004018.htm
13. Natural Patterns of Sleep. Healthy Sleep. Division of Sleep Medicine at Harvard Medical School. Dec 18, 2007 http://healthysleep.med.harvard.edu/healthy/science/what/sleep-patterns-rem-nrem
14. Circadian rhythm. Wikipedia The Free Encyclopedia.Feb. 26,2015 http://en.wikipedia.org/wiki/Circadian_rhythm
15. Circadian Rhythms Fact Sheet . National Institute of General Medicine Nov. 2012 http://www.nigms.nih.gov/Education/Pages/Factsheet_CircadianRhythms.aspx
16. Luke Mastin. Sleep-Wake Homeostasis, How Sleep Works. Sleep 2013 http://www.howsleepworks.com/how_homeostasis.html
17. Sleep Assessment Quiz. Martha Jefferson Sleep Medicine Center http://www.mjhsleep.org/Uploads/Public/Documents/MarthaJefferson/assessment.pdf
18. 5 Common Sleep Disorders. Atlantic Health Sleep Centers http://www.ahsleepcenters.com/articles
19. An Overview of Insomnia. Sleep Disorders Health Center, WebMD. Aug. 21,2014 http://www.webmd.com/sleep-disorders/guide/insomnia-symptoms-and-causes
20. Insomnia. Wikipedia The Free Encyclopedia.Feb 12, 2015 http://en.wikipedia.org/wiki/Insomnia
21. Medicines for Insomnia. Sleepdex.org http://www.sleepdex.org/meds.htm
22. Laurie Udesky. Sundown Syndrome. Caring.com https://www.caring.com/articles/sundown-syndrome
23. Annette (Gbemudu) Ogbru, PharmD, MBA . Sleep Disorder Drugs (Hypnotic and Sedative Drugs). RxList.com Nov. 15, 2011 http://www.rxlist.com/sleep_disorder_medications/drugs-condition.htm
24. Hypnotic. Wikipedia The Free Encyclopedia. Jan 21 2015 http://en.wikipedia.org/wiki/Hypnotic
25. Karen J. Tietze, PharmD. Nonprescription antihistamines: Geriatric considerations. Pharmacist.com American Pharmacist Association Dec 01 2012 http://www.pharmacist.com/nonprescription-antihistamines-geriatric-considerations
13 Ways to Help Residents Sleep Normally
Exam Portal
click on [Take Exam]
Purchase membership here to unlock Exam Portal.
|
|
|
|
|
*Important*
Registration and login is required to place your name on your CE Certificates and access your certificate history.
Username MUST be how you want your name on your CE Certificate.
| Guest: Purchase Exam |