A Caregiver’s Guide to Inhalers
A Caregiver’s Guide to Inhalers
Author: Mark Parkinson BsPharm: President AFC-CE
Credit Hours 4 - Approximate time required: 240 min.
Educational Goal
Enable caregiver to properly facilitate inhaler device therapy.
Educational Objectives
- Present the basic anatomy and physiology of the respiratory tract.
- Discuss the two main types of lung pathology
- Prove through statics that the pathology is not well controlled despite readily available therapy.
- List the reasons for inhaler therapy failure
- Provide an understanding of inhaler types
- Give information that will enable caregivers to facilitate proper inhaler device use.
Procedure:
Read the course materials. 2. Click on exam portal [Take Exam]. 3. If you have not done so yet fill in Register form (username must be the name you want on your CE certificate). 4. Log in 5. Take exam. 6. Click on [Show Results] when done and follow the instructions that appear. 7. A score of 70% or better is considered passing and a Certificate of Completion will be generated for your records.
Disclaimer
The information presented in this activity is not meant to serve as a guideline for patient management. All procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this article should not be used by care providers without evaluation of their patients’ Doctor. Some conditions and possible contraindications may be of concern. All applicable manufacturers’ product information should be reviewed before use. The author and publisher of this continuing education program have made all reasonable efforts to ensure that all information contained herein is accurate in accordance with the latest available scientific knowledge at the time of acceptance for publication. Nutritional products discussed are not intended for the diagnosis, treatment, cure, or prevention of any disease.
A Caregiver’s Guide to Inhalers
Quickly, take a breath. Taking a deep, cleansing breath always feels so good. Can you imagine trying to take a deep breath and that big inrush of air doesn’t happen? Instead, only a small wheezing trickle of air comes into your lungs. How terrible would that be if it happened over and over again? This is the health concern that is faced by many of your residents. Foster care providers are in a good position to help—but only if they understand how to help. Let us get started with a brief discussion about the respiratory system, its disorders, and how they are treated.
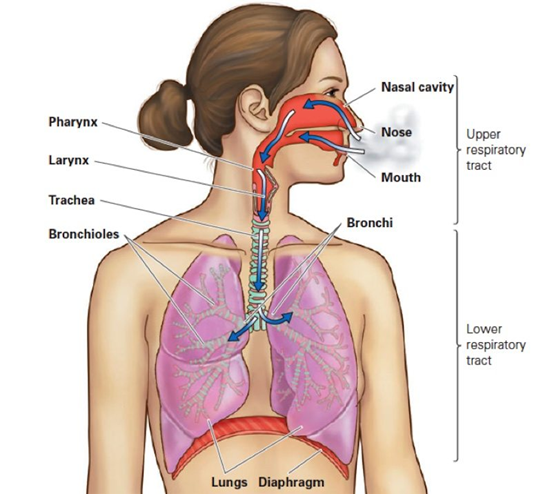
The Respiratory Tract
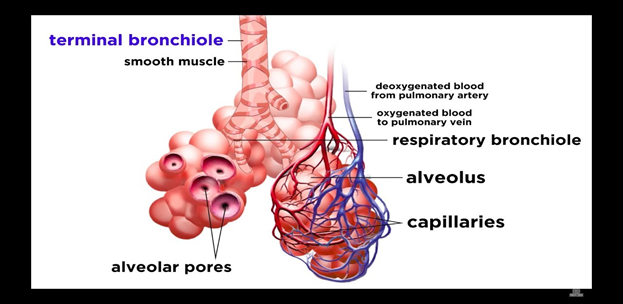
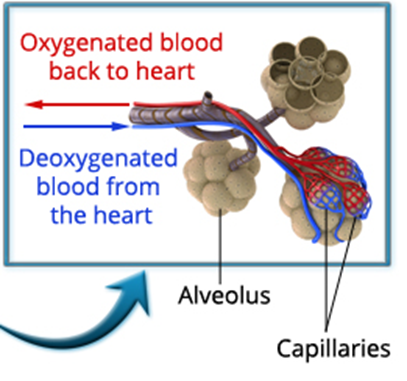
The respiratory system consists of the organs and structures used to exchange the gases we utilize to live and function. It is divided into two parts. The upper respiratory tract is the mouth, nose, sinuses, and throat. The lower respiratory tract is the throat below the vocal cords, lungs, and diaphragm. The lungs are subdivided into the trachea, bronchi, bronchioles, and alveola.
Lining the respiratory system are several concentric layers of specialized tissue. Throughout the layers, you will find, to varying degrees, cartilage, muscle, nerves, blood vessels, mucosal cells, epithelium cells, and immunity cells, all of which have their part to play in taking in the oxygen we need to function. Once in the lungs, the oxygen can diffuse into the bloodstream and be transported around the body. In a reverse process, the carbon dioxide waste gas we produce diffuses out of the bloodstream and into the lungs, where it is exhaled. If all the parts work properly, respiration occurs. If something goes wrong, the whole body suffers.
 |
 |
Diseases and Disorders
I’m not going to have a long, drawn-out discussion about everything that can go wrong in the lungs. For brevity, I am going to lump them into two broad categories and name them “asthma type” and “COPD type.” I know that I am taking quite a large medical literary liberty by doing so. Please don’t sweat the details, and instead, look at the broader picture I’m painting.
Asthma Type
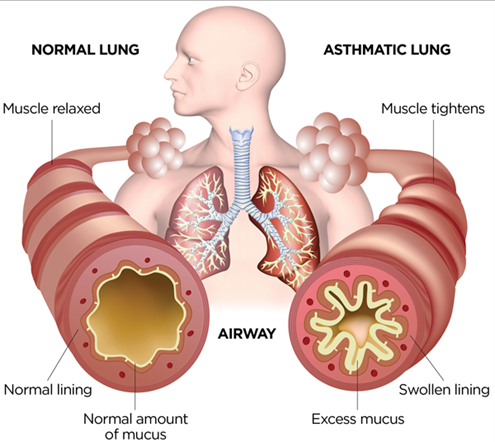 Asthma is an inflammatory condition in the lungs. The layers lining the lungs become inflamed and swollen to the point that the airway paths are severely reduced. Along with the inflammation, extra mucus is produced. Together, these conditions block the capacity to breathe normally. Asthma symptoms can be triggered by environmental factors like allergies or pollutants, or they can be triggered by internal events like a sudden increase in exercise or strong emotions. The likelihood of an asthmatic condition manifesting itself can be increased by disease or genetic factors. The signs and symptoms of asthma are difficulty breathing, chest pain, cough, and wheezing. The symptoms can be seen as part of a chronic condition or a sudden flare-up called an asthma attack.
Asthma is an inflammatory condition in the lungs. The layers lining the lungs become inflamed and swollen to the point that the airway paths are severely reduced. Along with the inflammation, extra mucus is produced. Together, these conditions block the capacity to breathe normally. Asthma symptoms can be triggered by environmental factors like allergies or pollutants, or they can be triggered by internal events like a sudden increase in exercise or strong emotions. The likelihood of an asthmatic condition manifesting itself can be increased by disease or genetic factors. The signs and symptoms of asthma are difficulty breathing, chest pain, cough, and wheezing. The symptoms can be seen as part of a chronic condition or a sudden flare-up called an asthma attack.
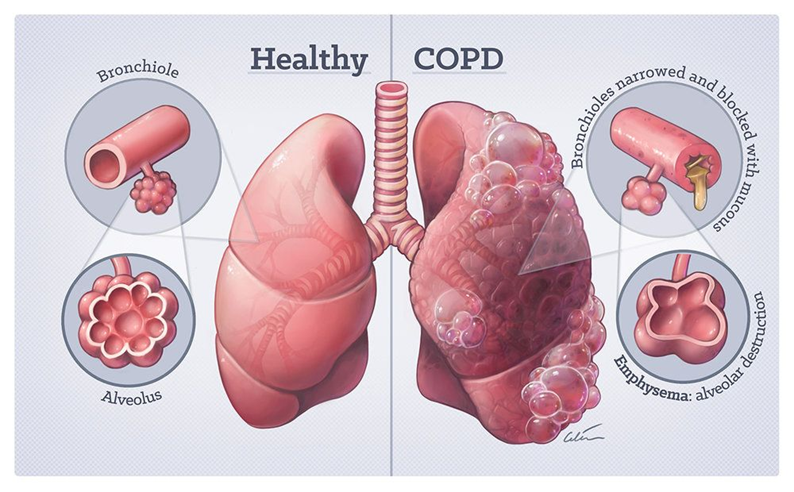
COPD Type
COPD, or chronic obstructive pulmonary disease, refers to a group of diseases that cause airflow blockage and a reduced capacity to exchange gases normally in the alveola. Exposure to toxins (like those in tobacco) and disease progression cause permanent damage to the lung tissues. The loss of lung tissue reduces the ability to breathe properly. Emphysema and chronic bronchitis are the two most common conditions that contribute to COPD. In emphysema, the alveoli have been damaged or destroyed. In bronchitis, the lining of the bronchial tubes is inflamed, and becomes mucus-filled. The signs and symptoms of COPD are shortness of breath, wheezing, chronic cough, and extra mucus production.
Asthma and COPD are both common respiratory disorders. Asthma can be seen in all ages, including the very young. COPD is usually seen in adults, with its prevalence increasing with age. Worldwide, approximately 300 million have asthma, and 10 percent of the adult population over the age of 40 years may have COPD. These conditions are common enough that, sooner or later, every foster caregiver will have to care for a resident with breathing difficulties.
Caregiving and Breathing Problems
Asthma and COPD are incurable diseases. The breathing problems—or the potential for breathing problems—will plague the resident for the rest of their life. Both conditions can be managed with the help of the right equipment, medication, and an understanding of how to use them. Medical oxygen can compensate for the reduced airflow, and medications can open airways by controlling the inflammation and reducing mucous production. Properly applied, these treatments can enable your resident to have a fairly normal life.
The majority of medications used for your residents with breathing problems are delivered via inhaler devices. They are the gold standard in respiratory care. Doctors prefer inhalers because they have several advantages over other treatment options.
- They enable the medication to be delivered directly where it is needed immediately.
- Doses of medication are small so that side effects can be reduced.
- The inhalers are portable and convenient, and they require little if no preparation to dispense the drugs.
But (and this is a Big But) the patient has to be taught how to use them. Inhalers requires practice to properly deliver the medication where it is supposed to go. If inhalers are used incorrectly, the outcome is less than desirable.
The Problem
Even though effective inhaler-based treatment options are readily available, asthma and COPD patients continue to suffer from their diseases. Far too many deaths from these controllable conditions are still being reported. It is a tragedy that so much suffering still occurs from these largely preventable adverse conditions.
The Stats
In medical studies, it has been shown that if patients use their inhalers correctly just 80 percent of the time, respiratory disorders can be controlled. But during recent research, it was observed that adherence to inhaler therapy rates are much lower, ranging from 73 percent to as low as 8 percent. It was also observed that when patients do use their inhalers, the majority of patients made errors in inhaler use. Non-adherence to therapy and improper inhaler use has resulted in a major health problem in the United States.
The impact of COPD:
- Over 16 million doctor’s visits a year are related to COPD
- It is the fourth-leading cause of death in the United States.
- Direct costs for COPD are estimated to be over $18 billion annually.
The impact of asthma:
- Asthma accounts for 9.8 million doctor’s office visits, 188,968 discharges from hospital inpatient care, and 1.8 million emergency department visits each year.
- Asthma is the third-ranking cause of hospitalization among children younger than 16
- Each day, ten Americans die from asthma, and in 2017, 3,564 people died from asthma. Many of these deaths are avoidable with proper treatment and care.
- Adults are four times more likely to die from asthma than children.
- Women are more likely to die from asthma than men and boys are more likely than girls.
- From 2008–2013, the annual economic cost of asthma was more than $81.9 billion—including medical costs and loss of work and school days.
Source: https://www.aafa.org/asthma-facts
The Solution
How could this all have happened, and can it be prevented? That is where you, the in-home care provider, can step in and have a huge impact on those in your care. You can do what foster caregivers do better than anyone else, including family, doctors, nurses, therapists, and pharmacists. You are THE 24-7 therapy facilitator specialist. You can ensure that therapy is followed and done correctly. But you can’t facilitate anything until after you have the knowledge and skills required. So, let’s get to it and start learning what you need to know.
The Causes of Non-Compliance
The reasons for non-compliance in respiratory therapy are as complex and varied as humans are themselves. It can be a bit intimidating to caregivers to try to tackle such a huge subject. That is, until you simplify things by placing all various reasons for non-compliance into two categories: intentional non-compliance and unintentional non-compliance.
Intentional Non-Compliance
Intentional non-compliance is all the reasons a patient gives for not wanting to cooperate. Those who have been in the caregiving profession long enough will recognize the following list.
- The belief that a particular medication is unnecessary
- Concerns about side effects
- Medication costs
- Social stigmas
- Unrealistic expectations of treatment
- Dissatisfaction with health-care providers
- General poor health that leads to grouchiness or just plain, old-fashioned grouchiness
- Apathy (just doesn’t care or has a lifetime of poor health habits)
Intentional non-compliance is the easier category to understand and to manage … at least for foster care providers. Just perform your daily routine of good care practices, and eventually, even the grouchiest, most non-compliant resident will come around. New habits will be established, and greater understanding and acceptance will occur, but only if you maintain your good practices and persevere in your efforts. By the way, only foster care providers can apply this kind of behavior-altering pressure on the patient. Every other medical professional sees the client too infrequently to have as much of an impact on patient compliance as your caregiving efforts do.
Here are a few ideas for your caregiver’s mental toolbox.
- Consistency is key. Stick to a regime—repeated actions lead to habits.
- Appeal to an authority who is not there to argue with. Say that the doctor, nurse, family member, etc. said to do it. You’re just following orders. They can’t argue with you because you’re not the one giving the orders.
- Give treats as a reward for compliance, thus reinforcing good behaviors.
- If they complain of the taste, promise to wash it down with juice or a snack.
- Point out the benefits. “Don’t you want to breathe better?”
- Point out the consequences. “Do you really want to have difficulty breathing?”
- Emphasize outcomes. “I’m glad to see you’re breathing so much better. That medicine sure is effective.”
- Sincerely compliment efforts. “Now you’re getting the hang of it. Soon you’ll be teaching me how to use the inhaler.”
- Empathy is rewarded with compliance, if done appropriately. Say things like, “I would think that using the inhaler all the time is a nuisance, but on the other hand, I would think that not breathing is worse.”
- Educate the resident. Question them on what they think the inhaler is for, what side effects they think they have, and what benefits they think they are getting from the medication. Then correct any misconnections or fill in any missing information.
Unintentional Non-Compliance
 Unintentional non-compliance is where the resident wants to cooperate but still falls short in their therapy. This type of non-compliance falls into three categories: forgetfulness, misunderstanding of the instructions, or poor inhaler technique.
Unintentional non-compliance is where the resident wants to cooperate but still falls short in their therapy. This type of non-compliance falls into three categories: forgetfulness, misunderstanding of the instructions, or poor inhaler technique.
In my opinion, this is where most of the problems with non-compliance occur. That may surprise you, considering these are the patients who want to cooperate. They think they are using the medication the way it was prescribed but, for one reason or another, they are falling short of full adherence to therapy. This leads to sub-optimal outcomes and the patient still suffers. Often, the patient gets frustrated with their therapy, wondering why it’s not working for them. If the frustration continues, they lose confidence in the treatment or the prescriber and become less willing to comply with instructions.
In one study of inner-city children with asthma, 87 percent showed they had poorly controlled symptoms. It is small wonder that the same study showed that only 1 percent of the children’s caregivers were able to demonstrate proper inhaler technique.
Stating again what is now more obvious, this is where foster care providers can have the greatest impact. You are in the unique position of being with the patient the most. You can remember for the client when to use the inhaler. You can objectively evaluate inhaler technique and catch errors in inhaler use. You can identify and report any handicaps and barriers that prevent optimal drug therapy. You can follow up with concerns, help overcome handicaps, and continually ensure that therapy is followed. With a little effort on your part, things will only get better for your residents. Let’s go over a few caregiving suggestions I have for you.
Ways to Manage Forgetfulness
Life events and activities of daily living tend to compete for the attention of every person, including residents and their caregivers. It’s only human to forget even the most important of action items. Here are a few ways to help you and your resident remember their inhaler medication in a foster care setting. These are by no means the only methods of remembering dosage times. The following ideas are meant to augment what you are currently doing.
The Caregiver
A caregiver tool to help you remember medication administration times is good recordkeeping techniques. That’s right, the MARS. You know, that annoying chore that every caregiver wants to avoid and is tempted to put off until the very last day before inspection. But you got it all wrong. The MARS is not a chore; rather, it is the most powerful memory tool you’ve got. If utilized properly, it’s the ultimate “to-do” list for medication administration.
I suggest making filling out the MARS a part of the drug-dispensing routine. Fill it out as you’re giving out the meds. Don’t hide away the MARS in a closet; pull it out and bring it with you when you grab the meds. Heck, use it as a tray to carry the meds. Put it right down in the middle of things where it can’t be overlooked. Tie a pen on a string and attach it to the MARS where it will be handy. As you dispense the drug, fill out the MARS, just like crossing off an item on a to-do list. Then, move on to the next medication to dispense. If you regularly use the MARS several times a day, you will never forget to dispense the resident’s medication. I promise you, if you avoid filling out the MARS in robot mode and use it instead as a to-do list, the resident will always be compliant with medication times. (And you will never again worry about being dinged during an inspection.)
Another powerful memory tool is timer alarms. You can buy medication delivery devices with sound reminders, but why spend the money? Just set up your smartphone with timer alerts apps. It’s not that much effort to download free versions to your cell phone.
The Resident
First things first: Get permission from the doctor to self-administer all inhaler medications. This is one of those details that can come back to bite you come inspection and relicense time. You will find it easier to obtain the necessary documentation if you do all the work for the doctor. Write out your own order and have a place for the doctor to sign.
It doesn’t have to be fancy, and you can certainly copy other self-admin orders you have seen. In fact, you can copy the format below:
__________________________________________________________________________________
Consent to Self-Administer Medication
_________________________
Resident’s name
_________________________________ __________
Medication Dosage
_________________________________
Time of administration
I have prescribed the specified medication to the patient listed above and authorize the patient to self-administer it as I have instructed.
________________________________
Signature of the prescriber
__________________________________________________________________________________
Please return to: Business name, address, email, fax, or include in patient’s return file.
A final note on self-admin forms: As a matter of courtesy and to avoid future problems, make a copy of yours and send it along with the resident if they participate in any event, work, or program where you are not present. That thought brings us to the next item.
There will always be times when you are not around to remind the resident to use their inhalers, such as recreational or work programs and family outings. During such events, your resident will experience extra distractions that will make them forget their medication. You will have to set things up so it is easy for the resident to remember their dose. Here are a few ideas that might help. 
- Reminder notes are good, but timer alarms are better. Buy a cheap timer from Walmart and set it for them for when the inhaler dose is due. Slip it into their pocket before each trip and collect it when they get back. That way, you have control and can make time adjustments when needed. It will also give you an opportunity to visit with the resident about their inhaler use.
- Educate the resident on what the medication does for them and when it is to be taken. Let them ask questions. If you don’t have the answers, ask the pharmacist or prescriber. The idea is to give them enough information so that they will buy into the need for taking the medication and alleviate any lingering fears.
- Educate the person in charge of the outing. Make sure they have enough info to gain their cooperation. Supply them with a copy of the self-admin order from the doctor. If the outing is a repeated event, provide a mini MARS that requires filling out when doses are given. The responsible person will not really be responsible for filling it out, but it will be a motivational tool and give you information that you can follow up on.
- Keep the inhaler noticeable. If the resident is responsible enough, slip the inhaler into their pocket, where it can be felt. If they will have trouble with that, give it to a responsible person for safekeeping. Another idea is to drill a hole in the plastic case of the inhaler and put a string through it, so it can be worn as a necklace. Have the resident place the inhaler necklace under their clothes for privacy reasons. When you are sending an inhaler with the person, it would be wise to get the prescriber to write the prescription for additional inhalers in case one gets lost.
- Have them return and report. Tell them that you are required to keep track of when the inhaler gets used and are relying on them to help fulfill your responsibility. Have the MARS handy and fill it out as they report. It will give them a sense of importance and a feeling of control that will inspire further cooperation. You see, the MARS is a tool, not a burden.
Misunderstanding of the Instructions
As far as medications go, inhaler use is quite involved. It is a lot more complicated than just popping a pill every day and you’re done. In order to get the full benefit out of the medication, the patient has to know when to take it, how to use the device, and why they are taking it in the first place. The data in studies show that misunderstandings are occurring in far too many cases. Why is that? The doctor and/or the pharmacist are supposed to educate the patient in all these details to ensure the medication’s proper use. “Yeah, right. Like that happens 100 percent of the time.” At the very least, they are supposed to send home literature explaining everything. “Well, you know how often the patient reads those wonderful literary masterpieces.”
 Now consider understanding inhaler medication from the perspective of your resident’s point of view. How much medical training have they had? Add to that the mental acuity of your typical foster care resident. They are handicapped by their age (too old or too young) or impaired by their condition (developmentally disabled or mental-health challenged). In addition to those factors, think about how often they have seen their prescriber or pharmacist. “Once a year if you’re lucky.” Finally, think how long ago they received their initial instructions on inhaler use. “Months or even years, maybe.” Given these facts, it is small wonder that so many patients misunderstand their inhaler instructions.
Now consider understanding inhaler medication from the perspective of your resident’s point of view. How much medical training have they had? Add to that the mental acuity of your typical foster care resident. They are handicapped by their age (too old or too young) or impaired by their condition (developmentally disabled or mental-health challenged). In addition to those factors, think about how often they have seen their prescriber or pharmacist. “Once a year if you’re lucky.” Finally, think how long ago they received their initial instructions on inhaler use. “Months or even years, maybe.” Given these facts, it is small wonder that so many patients misunderstand their inhaler instructions.
You would be totally justified in thinking that none of your residents totally understand their inhaler medication instructions. In my expert opinion, you should assume that the resident doesn’t understand their inhaler medication. Start from scratch on every single inhaler prescription that comes into your home, no matter how long the resident has been on it. Even if I am proven wrong and they do understand the instructions, it is always wise to have a review of the details every so often.
If you are starting to get apprehensive about helping the residents with their inhalers, don’t be. It may appear that inhaler use is very difficult and impossible to get right. Quite the opposite is true. Inhalers are designed to be simply understood and used by almost anyone. You just need to be instructed on some of the basics and you will be good to go. As you read the following details about inhalers, remember, you’re not the prescriber, you’re the facilitator of therapy. You don’t have to understand the ins and outs of a drug. You just have to know enough to see that it’s used correctly.
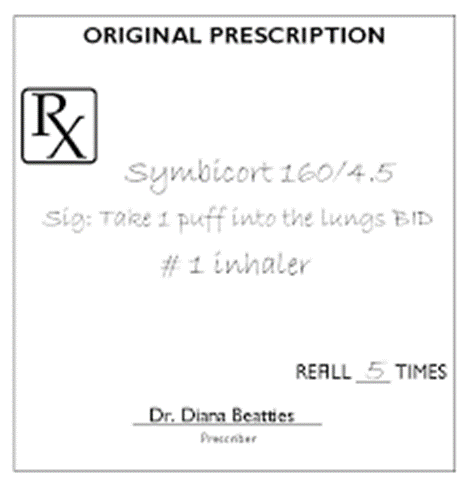
The Prescription
As you know, the prescription contains the prescriber’s instructions on how the patient is to use the medication. When you first receive the medication from the pharmacy, read the instructions to see if you understand it. If you don’t fully understand it, ask the pharmacist questions until you do. Don’t worry about bothering the pharmacist. Remember, it’s your license on the line if you don’t ensure the doctor’s orders are followed as he or she intended.
Look for the hidden details that are not spelled out. For example:
- Inhale by mouth 1 to 2 puffs as needed. Ask the pharmacist – How much time between puffs? As needed for what? How do you know when the second puff is needed? How long would you have to wait before giving the drug again? If the drug doesn’t seem to be working, then what do you do?
- Take once daily. Ask the pharmacist – What time of day is the best time to take the medication? Why is that time the “best” time? What circumstances would justify a change in that time? How many days is the prescription supposed to last? When should I call in for refills?
- Use as directed. Just hand the bag back to the pharmacist and say, “Call the doctor for better instructions.” Teach the pharmacist about what is required by foster care providers. If they are not cooperative, tell them you will have to go over their heads and call the doctor for a better written prescription.
- If there are multiple inhalers prescribed, ask in which order they are to be used and how much time should be allowed between doses. (You might have to call the doctor for the answer to these questions.)
- Rarely will the prescription label be placed on the inhaler itself. That means, when the inhaler is used away from your home, the instructions for use will be missing. If the patient is going to be taking the device outside your home on a regular basis, it would be wise to ask for a second label. From the second label, cut out the essential instructions and stick them directly on the device.
Patient Drug Information Insert
Every medication that comes from a pharmacy has to have an information sheet. Have you taken the time to read those papers from the perspective of a caregiver? It has listed almost everything you need to know to manage the resident’s medication use. It’s all spelled out in black and white in everyday language. How easy is that?
I went down to my local grocery store pharmacy and picked up an information sheet on an albuterol inhaler. Listen to how it is organized.
- What is this drug used for?
- How is this drug best taken?
- What are some other side effects of this drug?
- What are some things I need to know or do while I take this drug?
- If overdose is suspected:
- How should I store and/or throw out this drug?
It’s practically a caregiver’s training guide on albuterol. The only thing that is missing is how to fill out the MARS.
Once the details are clear to you, set some time aside to counsel with the resident. Normally, caregivers don’t have to have a discussion with their residents about their drugs. But since inhaler devices are essentially self-administered, they require a degree of understanding and cooperation that must be verified by the caregiver. When you counsel with the resident, remember to be non-judgmental and use plenty of caring empathy in your discussion.
I suggest you start out by asking the following questions.
- What do you think this inhaler is used for?
- When do you usually take it?
- How do you think the medication helps you?
- How can you tell if the medication is working?
- Could you show me how you use it?
- Do you have any concerns about the drug?
- Do you have any difficulties when using the inhaler device or devices?
As they answer your questions, you may start to notice misconceptions and misunderstandings the patient has collected over the course of their therapy. How you correct those misunderstandings will take some skill. I suggest that you do not try to make any corrections after each response. Wait until all the questions are done. If corrections need to be made, do not make the resident feel like they were wrong. You will get more cooperation if you do not make them feel bad about what they have done in the past. Tell them that there is a better way, better understanding, or better techniques that will help them get better outcomes from their therapy.
Another counseling technique is not addressing the error in understanding at all. Make the correction appear to be something brand new. Say something like, “Well, it looks like there was a change somewhere along the way because I was told the doctor wants you to take the medication like this (add the correct detail). The doctor must have thought that you would feel better if you did it this way.”
Empathy can also be used to gain cooperation when changes are needed. Say something like, “I totally understand why you think (or feel) that way. Given your circumstance, I think I would have thought (felt) that way too. But there is a better way (better understanding) that will help you even more.”
There are circumstances when the mental abilities of the resident are so low that any discussion would just confuse the resident. In these cases, it is better to present the correct information as an authority figure. Confidence in your demeanor will be key for better outcomes.
Be careful not to blame any misconceptions on the doctor or pharmacist or you will undermine the resident’s confidence in them. That will only lead to problems down the road.
The Family or Other Responsible Person
Finally, do not forget to counsel with family members or other responsible persons who have influence on the resident in any significant way. If you do not include them in the conversation, they may undermine all your efforts to change the situation.
Poor Inhaler Technique
The vast majority of patients make at least one error in inhaler technique. Your residents either picked up some bad habits along the way, forgot their initial instructions, or were never shown the proper technique in the first place. If it wasn’t for the fact that inhalers are designed to be easily used, I don’t think that anyone would be close in getting it right.
The reality is that most health-care professionals are not very good at teaching their patients proper inhaler technique. In one study of pulmonologists (they are supposed to be the inhaler therapy specialists), it was discovered that only 43 percent were knowledgeable in teaching patients how to use inhalers. The problem is lack of available training. I remember as a practicing pharmacist I was never given any instructions on how to educate a patient when a new inhaler hit the market. I was supposed to just know what to say. I assume the same happens with doctors and nurses. Even if the resident was shown the proper technique, one education session is rarely enough to ensure proper inhaler use over the course of the therapy.
Knowing these facts should give you, the caregiver, the proper perspective when you start working with your residents. You are in a great position to teach what has not been taught and help remember what has been forgotten. After all, you have more time with and better access to the patient than any other health professional. Why shouldn’t foster caregivers be the ones to support proper inhaler technique? “But where is my training?” I hear you say. This CE is the start. I will show you how to access more training as we continue. All you will need is a computer, your good communication methods, and your keen observational skills. You will be able to help your resident have better inhaler technique.
Let us start with the basics. There are three varieties of inhalers: metered-dose inhalers (MDIs), dry powder inhalers (DPIs), and slow mist inhalers (SMIs). Each type relies on a different mechanism to deliver the medication into the lungs. I will give a general description of each category, but don’t get too caught up in the narrative. Each brand of inhaler will have its own set of specific instructions. I will cover how to get those instructions later.
Metered-dose inhalers deliver the medication via a propellant from a pressurized canister. It works in the same way as an aerosol can of hairspray. By depressing the canister into the plastic mouthpiece, a measured dose of the drug is pushed into the lungs. This is the type of inhaler that most people are familiar with and, unfortunately, it is the most difficult type to get right.
Patient Instructions
- Remove the cap from the MDI and shake well.
- Breathe out all the way.
- Sit up or stand with your back straight.
- Place the mouthpiece of the inhaler between your teeth and seal your lips tightly around it.
- As you start to breathe in slowly, press down on the canister one time.
- Keep breathing in slowly and as deeply as you can. (It should take about 3–5 seconds for you to completely breathe in.)
- Hold your breath for 10 seconds (count to 10 slowly) to allow the medication to reach the airways of the lungs.
- Repeat the above steps for each puff ordered by your doctor. Wait about 1 minute between puffs.
- Replace the cap on the MDI when finished.
- If the inhaler is a corticosteroid MDI, rinse out the mouth after each use.
Caregiver Instructions
- Make sure there is medication in the canister. The most accurate way is by keeping track of how many times it is used. Each box has listed how many total doses there are, and you just count it down each time it is used. The MARS will come in real handy for this. Remember to record when a new inhaler is used in the MARS. Once the number of doses is used up, don’t count on the inhaler working for symptom relief, even if the inhaler continues to spray.
- New inhalers will have to be primed by shaking the inhaler and spraying it into the air one to two times. If the inhaler sits for over two weeks, prime it again. Don’t count the primer sprays in the dose countdown.
- The plastic mouthpiece should be rinsed with warm water once a week and left to air-dry. Remove the canister before cleaning. If the canister can’t be removed, wipe its opening with a soft rag or cotton swab.
- The timing and speed of breath intake is very important. If the resident inhales too late or too soon, the medication is sprayed on the back of the mouth or tongue. The medication is then swallowed into the stomach, where it doesn’t do much good. If the intake is too fast and strong, most of the medication ends up too deep in the lungs. The drug has to be deposited all along the airway to have full effect. Some residents are so used to tasting the medication as a result of bad technique that they think that they didn’t get the dose if they don’t taste it. You will have to educate them the opposite is true.
- Make sure the resident is breathing through the mouth and not their nose. Make sure the tongue is placed under the mouthpiece and out of the way.
- During times of stress, the resident will have difficulty with the timing and thinking clearly. Keep watch during these times and coach them along.
- If the resident just can’t get the timing or breathing right, ask the doctor for a “spacer” prescription. It is a special hollow tube designed to hold the spray in the air of the tube. This makes it easier to breathe in the medication correctly. Pediatric versions can come with a mask for even easier use. Spacers also need to be periodically cleaned as per manufacturer instructions.
Spacer Instructions
- Remove the cap from the MDI and chamber. Shake well.
- Insert the MDI into the open end of the chamber (opposite the mouthpiece).
- Place the mouthpiece of the chamber between your teeth and seal your lips tightly around it.
- Breathe out completely.
- Press the canister once.
- Breathe in slowly and completely through your mouth. If you hear a horn-like or whistle sound, you are breathing too quickly and need to slow down.
- Hold your breath for 10 seconds (count to 10 slowly) to allow the medication to reach all the airways of the lung.
- If the resident is still having issues even with the spacer, ask the doctor for another type of inhaler or maybe even a nebulizer.
- Monitor for effectiveness and side effects.
DPI
Dry powder inhalers deliver the medication as a fine powder mixed into the air of the inhaled breath. They come in either a multidose inhaler or as individual capsules that are placed into the devices with each use. In either case, the drug-containing capsule needs to be punctured by the device before a breath is inhaled. Most often, it makes a clicking sound. The medication is released only when the user takes a deep, fast breath in through the inhaler.
Patient Instructions
- Remove the cap.
- For single-use devices, load a capsule into the device as directed.
- Sit up or stand with your back straight.
- Breathe out slowly and completely (not into the mouthpiece).
- Place the mouthpiece between the front teeth and seal the lips around it. Hold it like a sandwich.
- Breathe in through the mouth quickly and deeply over two to three seconds. Suck like drinking through a straw.
- Remove the inhaler from the mouth. Hold your breath for as long as possible (10 seconds).
- Breathe out slowly.
- Rinse the mouth after use.
Caregiver Instructions
- Do not shake the device or let the resident shake the device before use.
- As you set up the device, listen for the telltale click that lets you know the drug-containing capsule has been broken. Then hand the DPI to your resident.
- Do not let the resident blow into the device.
- Never use a spacer with a DPI.
- If the medication is a corticosteroid, make sure they rinse their mouth after use and spit out the water.
- Clean the mouthpiece with a clean cloth but do not get the device wet.
- Each multidose device comes with a counter so you know when to reorder the prescription.
- The resident will most likely not taste or feel the medication. Assure them that they are getting the drug delivered to the proper area of the lungs.
- The technology relies on a deep, strong breath. If the resident has trouble with that, consult with the doctor.
- Monitor for effectiveness and side effects.
SMI
Soft mist inhalers deliver the medication via a sprayed mist. It does not have a propellant but has a spray of fine vapor, which is breathed into the lung. They are also known as Respimat inhalers and are the newest device type on the market.
Patient Instructions
- Hold the inhaler upright with one hand, with the cap closed. Use your other hand to turn the clear base to the right until it clicks.
- Open the cap.
- Sit upright or stand with your back straight.
- Breathe out slowly and completely.
- Put the mouthpiece in your mouth, holding the inhaler horizontally (pointing toward the back of your throat).
- Close your lips around the mouthpiece, making sure not to cover the air vents on the sides.
- Take a slow, deep breath in. As you start to inhale, press the button on the side of the inhaler.
- When your lungs are full, hold your breath for 10 seconds to keep the medicine in your lungs.
- Take the inhaler out of your mouth and breathe out slowly.
- Put the cap back on the mouthpiece.
Caregiver Instructions
- Before you can start using the SMI, insert the medication cartridge. Press the safety catch on the side of the inhaler and remove the plastic base. Push the cartridge into the inhaler until it clicks. (To make sure it is inserted completely, push the cartridge against a firm surface, like a tabletop.) Once the cartridge is in, put the clear plastic base back on and press until you hear a click.
- Brand-new devices need to be primed three times, as follows:
- Hold the inhaler upright with the cap closed and twist the clear base clockwise (to the right) until it clicks.
- Open the cap and point the inhaler at the floor, away from your face.
- Press the button on the side until you see a mist come out.
- Prime the device once if it has not been used in more than three days. If more than three weeks, prime it three times.
- The medication does not need to be shaken, but it does not hurt anything if it is. Spacers are not required.
- You may have to help the resident with step one.
- Clean the mouthpiece with a damp cloth.
- Monitor for effectiveness and side effects.
Foster Caregiver Considerations
You now have a basic understanding of the fundamental principles of inhaler therapy. You are by no means an expert, but you don’t have to be. You have enough info to get started. You certainly have more understanding than the resident has, and that is the whole point of foster care—taking better care of those who can’t take care of themselves. You may not be the authority on therapy and medication (that’s why you keep a doctor and pharmacist around) but you are the authority on “get ‘er done,”
Here are a few more ideas on “get ‘er done” and inhaler therapy.
Rescue vs. Regular
We have talked a lot about inhaler devices and technique. Now, let’s talk about the medication itself. I’ll spare you a long, drawn-out (and boring) discussion of the different classes of drugs and what they do. If you have a burning desire for that knowledge, ask the pharmacist for the package insert on the medication. What you do need to understand is rescue versus maintenance therapy.
Maintenance therapies are the drugs that prevent respiratory symptoms from occurring. Rescue medications are drugs that relieve breathing problems after they happen. Most likely that would be albuterol, but there are others. When you first receive the inhalers, ask which ones are the rescue inhalers. You can also tell which ones they are by the instructions on the prescription. They’re the ones that will be PRN (or as-needed).
There are two reasons why you ask about the rescue inhaler up front. First, you have to know what to reach for in breathing emergencies. Second, how often the PRN meds are being used is a great indicator of how the therapy is going. If the resident is having to be constantly “rescued,” you have to start thinking, “Why?” What is causing all the problems? Here are a few possibilities.
- Poor technique is preventing the maintenance medication from getting to where it belongs. Solution: Observe inhaler use and educate the resident when needed.
- Handicaps are interfering with therapy, especially in regard to how strong the breath needs to be for each type of inhaler. Solution: Make notes of your observations and consult with the doctor on what to do.
- The resident may be using the rescue medication as a crutch. This one is tricky. Define as needed. Along with the medical need, there may also be emotional need, or a need to feel secure. It is clear that there will always be an emotional element in respiratory therapy. It is very hard not to be afraid when you can’t breathe. If this is a concern, the fear may lessen over time as you provide a caring, safe environment in your home. Of course, you can always discuss the matter with the doctor.
- The resident may have developed a bad habit of relying on the rescue inhaler because they can feel it working, while the maintenance med can’t be immediately felt. Solution: Ensure proper use of the maintenance med, which will in turn reduce the need to be rescued. The problem will gradually take care of itself. If it doesn’t, concentrate on patient education.
- Before they moved into your home, the patient may have skipped the maintenance med when they felt good. Of course, that is not going to happen after they move in, because you’ll see to it that the med is taken as prescribed. If they balk, explain how constant use of the maintenance medication is the reason they felt good in the first place.
Evaluating Inhaler Technique
Pay close attention to how the resident uses their inhalers when they first move into your home. Keep observing inhaler technique from then on. You should know that their technique will suffer during respiratory distress. School them with empathy and caring, or you might add to their anxiety. They may not be able to hold their breath for the full count. To ensure proper breath-hold times, have them concentrate on counting to 10 with their fingers.
These are common errors made by the patient to watch for.
- Inhaler not shaken before use or shaken when it should not be.
- Incorrect body positioning. If they’re hunched over, they cannot take a full breath in.
- Failure to exhale fully prior to dosing.
- Poor coordination of depressing the MDI and inhalation.
- Breathing in too hard or too soft for the device they use.
- Breath-hold is not long enough after dosing.
- Failure to remember to rinse out the mouth.
Spacer Use and Care
Spacers are made of plastic, and plastic can build up an electrical static charge. The charge will make the medication stick to its side. Before using a spacer for the first time, you should wash the spacer with warm dilute soapy water. The device should be air-dried. Some brands are manufactured electrostatic-free, and no preparation is needed. Read the package instructions. When in doubt, wash them out. Cleaning the spacer with just warm water will cause the electrostatic charge to develop, reducing the effectiveness of the spacer. If you are using the pediatric version that comes with a mask, the same cleaning techniques apply. Also, when you use a mask, make sure there is a good seal around the entire mask. If you are careless, extra air will leak in and the entire dose of the med will not be inhaled.
When the Resident First Moves into Your Home
Inspect the inhalers and spacers. Determine which are the maintenance inhalers and which ones are the rescue inhalers. Do the inhalers need to be cleaned? Which ones are empty or close to being empty, expired, or broken and need to be replaced? When in doubt, replace them.
Determining How Full the Canister Is
Using the MARS to keep track of how many doses are left is the best way to determine when prescriptions should be renewed. But that’s not the only way. It is also not as useful when you cannot account for every dose used, for example, when they first move in or when the inhaler is used outside of the home. Two methods of estimating what remains in the MDI inhaler are:
- Remove the canister and drop it into a bowl of water. See how it floats. Straight up and down means the canister is full. Floating horizontally means empty. If you are forced to use this method, dry the canister completely before use and remember to prime the device.
- Read the package or call the pharmacist to find out how many doses there are in the inhaler. Then estimate how many puffs are used in a day. Find out how many days since the prescription was filled and do the math. Spraying the inhaler to see if something comes out will not work because even a medication-empty inhaler will continue to spray the propellant.
Rescue Inhaler Prescription Refill
For rescue inhalers, I recommend that you try to keep spares around just in case of emergencies. You can get around insurance refill issues by calling the pharmacy and finding out how many days’ supply they assigned the prescription. Most insurances will allow you to fill the prescription when 80 percent of the days assigned to the prescription fill have transpired. Keep ordering the rescue med early even if you don’t need it until you have a full extra prescription in reserve. Another method is to have the prescriber order two inhalers for a same-day’s supply. The insurance may not cooperate with that, though.
A Demonstration Is Worth a Thousand Words
Every brand of inhaler will come with its own specific set of instructions. You will find them tucked inside of the box that the inhaler comes in, written on a small paper insert. Take it out and become familiar with the device’s requirements. In my opinion, though, that is not good enough. The patient needs a demonstration. That is where you and your computer come into play.
There are thousands of demonstration videos on inhalers published by the drug manufacturers and knowledgeable health-care providers. The ways to find the good ones are:
- Type in a browser search field (for example, Google) the phrase “(brand name) demonstration video”.
- There will be a list of video websites that come up. Skip the “ad” ones unless it is the manufacturer’s website. Choose a likely candidate. Almost always, the video will be published on YouTube.
- Select the video and review who presented the video. Choose only reputable sources, for example, medical or professional organization websites.
- See how many views the video has. The larger the number, the more likely it will be a quality video.
- View several videos and choose the best ones to show your resident.
After watching the video, have the resident use their inhaler. This show-and-tell session will be critical for you in evaluating their understanding of the instructions. Work with the resident until they get it right. It may take several sessions. Some habits are just hard to break.
Remember to be humble and helpful. After all, you are no therapy expert. You are just someone who is supporting the resident’s efforts to get it right. If there are difficulties, first evaluate your own understanding and communication techniques. Are you getting it right? If there are still difficulties that are too hard to overcome, report them to the doctor. When you talk to the doctor, be specific in reporting your observations.
I recommend that you repeat the video or demonstrate sessions periodically. Once or twice is never enough to ensure continued proper inhaler technique.
Conclusion
Asthma and COPD are significant health concerns in many residents of foster care homes. Inhaled medications are the gold standard for treating these conditions, but these devices require a greater effort from the patient to comply with therapy requirements. Studies have shown that the majority of patients are not compliant with their therapy, thus leading to increased mortality and morbidity issues.
The reasons for non-compliance are complex and are either intentional or unintentional. There is a great need to assist the patient in becoming compliant with therapy that is just not being met. Foster care providers are uniquely situated to effectively take care of this need. They can observe and evaluate the resident’s understanding and compliance with therapy. Facilitate the resident’s effort to become compliant and report back to the prescriber any significant difficulties the resident is having.
Caregivers are also best suited to ensure continued compliance over the course of the therapy. I hope that this CE has helped the caregiver along with internet resources to become THE expert on “getting it done.”
As always, good luck in your caregiving efforts.
Mark Parkinson, BS Pharm.
References:
Stephanie Watson. Inhalers for COPD. Healthline, Aug 14, 2018. https://www.healthline.com/health/copd/inhaler-nebulizer
Laura Koppen PharmD, BCPS. Advances in Inhaler Technology: Helping Patients Increase Adherence. Power-Pak CE. UAN: 0430-0000-19-138-H01-P. Dec 20, 2019 https://www.powerpak.com/course/preamble/119037
Aimee Simone. Many Caregivers Unable to Demonstrate Proper Use of Kids' Asthma Inhalers. Pharmacy Times. 2013-11-11 03:06:17.
How to Use a Metered Dose Inhaler. Family Doctor.org. American Academy of Family Physicians. 2020. https://familydoctor.org/how-to-use-a-metered-dose-inhaler/
Jane Scullion. The Nurse Practitioners’ Perspective on Inhaler Education in Asthma and Chronic Obstructive Pulmonary Disease. Hindawi. Canadian Respiratory Journal. Volume 2018 |Article ID 2525319. https://www.hindawi.com/journals/crj/2018/2525319/
Toby GD Capstick & Ian J Clifton. Inhaler technique and training in people with chronic obstructive pulmonary disease and asthma. Expert Review of Respiratory. Medicine, 6:1, 91-103, DOI: 10.1586/ers.11.89. https://www.tandfonline.com/doi/pdf/10.1586/ers.11.89
Lynn B Gerald, PhD, MSPHRajiv Dhand, MD. Patient education: Inhaler techniques in adults (Beyond the Basics). Up To Date, Sep 29, 2020.https://www.uptodate.com/contents/inhaler-techniques-in-adults-beyond-the-basics
Exam Portal
click on [Take Exam]
Purchase membership here to unlock Exam Portal.
|
|
|
|
|
*Important*
Registration and login is required to place your name on your CE Certificates and access your certificate history.
Username MUST be how you want your name on your CE Certificate.