Bringing Your Residents to Tears – Remedying Dry Eyes
Bringing Your Residents to Tears –
Remedying Dry Eyes
Author: Mark Parkinson RPh: President AFC-CE
Credit Hours 2- Approximate time required: 120 min.
Educational Goal:
To teach about the dry eye condition and tell how to relieve it.
Educational Objectives:
Define the chronic dry eye condition.
Tell about the anatomy and physiology of the eye and tears
List Foster care issue in regards to dry eye relief
Tell about the therapies for dry eye relief
List and explain the drugs designed for dry eye relief
Procedure:
Read the course materials. 2. Click on exam portal [Take Exam]. 3. If you have not done so yet fill in Register form (username must be the name you want on your CE certificate). 4. Log in 5. Take exam. 6. Click on [Show Results] when done and follow the instructions that appear. 7. A score of 70% or better is considered passing and a Certificate of Completion will be generated for your records.
Disclaimer
The information presented in this activity is not meant to serve as a guideline for patient management. All procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this article should not be used by care providers without evaluation of their patients’ Doctor. Some conditions and possible contraindications may be of concern. All applicable manufacturers’ product information should be reviewed before use. The author and publisher of this continuing education program have made all reasonable efforts to ensure that all information contained herein is accurate in accordance with the latest available scientific knowledge at the time of acceptance for publication. Nutritional products discussed are not intended for the diagnosis, treatment, cure, or prevention of any disease.
Bringing Your Residents to Tears –
Remedying Dry Eyes
How often do you think about the moisture covering your eyes? If you’re like me, that would be never. That is until there is not enough moisture, and my eyes become dry. It’s then hard not to think of anything else but my dry eyes. If the condition continues, the problem becomes distractingly irritating. That is how some of your residents feel when they are afflicted with chronic dry eyes, sometimes referred to as dry eye syndrome. The goal of this CE course is to help you, the care provider, deal with dry eye syndrome whenever it occurs.
What is going on in dry eyes?
At its simplest, dry eyes are the sensations we feel in our eyes when there is an inadequate amount of tears to lubricate and nourish the surface of the eye. It is caused by either an insufficient quantity of moisture in the eyes or the tears are of such poor quality that they fail to meet the needs of the eye.
A more in-depth look at chronic dry eye presents a much more complex picture. Let’s start with the official name of the condition. Chronic dry eyes are medically known as dry eye disease, dry eye syndrome, keratoconjunctivitis sicca, dry eye disorder, ocular surface disease, and dysfunctional tear syndrome. Why are there so many names for the same thing? The reason is, there is not a single definition of dry eye disease that has been accepted by all medical practitioners. A general characterization was set forth by the International Dry Eye WorkShop which states, "Dry eye is a multifactorial disease of the tears and ocular surface that results in symptoms of discomfort, visual disturbance, and tear film instability with potential damage to the ocular surface. It is accompanied by increased osmolarity of the tear film and inflammation of the ocular surface." In plainer language, it says that it is a condition that results in discomfort and vision problems that could be caused by serval different factors. Let’s take a look at the eye to see what they mean.
Anatomy and Physiology of the Tears
The eyes, as they are commonly referred to, are actually a complex combination of bodily structures. They are comprised of the eye organ itself, eyelids, lashes, tear glands, muscles, blood vessels, and nerves. The structures associated with tears are the lacrimal gland, Meibomian gland, and goblet cells of the conjunctiva (inside portion of the eyelid).
Just as with the eyes, the substance commonly referred to as tears are also very complex, containing fatty oils, water, mucus, and more than 1,500 different proteins.
The moisture covering the eye is called the tear film. It serves to hydrate and lubricate the eye surface. It also provides a protective barrier and makes a smooth ocular surface that helps our sight, similar to a lens. It inhibits microbial growth, supplies nutrients to those portions of the eye surface that have no blood supply, and supports wound healing.
The tear film is generally composed of three layers:
The outermost layer is derived from meibomian glands in the eyelid margins. It contains lipids like cholesterol, fatty acids, and triglycerides. The meibum slows down evaporation of the water tear layer and provides barrier protection against foreign matter like dust and microbes.
The middle layer is called the aqueous layer. It is produced by the lacrimal glands. It makes up most of the tear film (approximately 98%) and contains water-soluble substances such as electrolytes, proteins, nutrients, and immunoglobulins.
The innermost mucin layer is composed of a mucus-like substance produced by specialized skin cells called goblet cells. It provides a cushiony surface that lubricates the eye and helps evenly secure the water layer to the eye surface.
The tear film is not a static thing. It is constantly being replenished with every blink. It is estimated that a majority of the tear film is replaced with every two blinks. The tears normally drain into the ducts linked to the nasal cavity.
Wow! Who knew that tears were so complicated? It is no wonder that there is no consensus in properly naming chronic dry eye problems. With thousands of components in tears and tear production, accurately naming all the things that could go wrong is quite the daunting task. Add to that complexity, the small size of the structures and quantities involved, and the difficulties in taking samples, doctors are forced into dealing with generalities rather than specifics when treating dry eye problems.

Pathophysiology of Tears (what has gone wrong)
In writing this CE course, I, like the doctors, have been forced into writing in generalities rather than specifics. If you desire specifics, then I suggest you consult with your local eye care professional. So, in general terms, dry eye problems can be caused by the low quantity and or low quality of tears. The disturbance of the base tear film leads to hyperosmotic conditions (the concentration of solids in the water increases). This causes cell damage, which triggers the inflammation process. Inflammation usually results in red, irritated eyes. Increased tissue swelling can squeeze off tear duct openings, further reducing the tear volume in the eye. If conditions continue to spiral down, then the compensation mechanisms of the eye can get overwhelmed, and a significant eye tissue damage can result. What brought about these conditions in the first place could have been triggered by a single problem or multiple factors.
Severity
Care providers should take every case of eye problems seriously, though some are more critical than others. There is always the possibility that chronic dry eyes can lead to permanent vision impairment.
- Mild symptoms are usually transitory and are caused by environmental factors or minor disease conditions. They are easily treated with proper eye care or over-the-counter eye drops.
- Moderate conditions start to affect the eyes in a way that impacts the quality of life of the patient. The symptoms start to cause chronic pain or discomfort and vision problems.
- Sever issues lead to desiccation (dried-out eye tissues) that can cause permanent sight problems.
Possible Contributing Factors
Hopefully, by now, if I have done my educating job right, you can appreciate the complexity of dry eye problems. I can easily make a list of contributing factors, but for a person to point at one and say “That is the root of the problem” is not so easy. Doctors and caregivers should be open to the possibility of multiple triggers.
- Environmental factors − Exposure to smoke, dust, and other particles increases the osmolality of the tear film. Wind and dry environments can increase evaporation. Failure to blink reduces the replacement of the tear film, leading to drier eyes. Reduced blinking can be caused by concentrating on computer or TV screens and reading. Sleeping with the eyes partially open or sagging eyelids caused by advanced age causes similar results.
- Age − As we age, overall body functions start to wear down. Dry eye complaints start to increase after the age of 50. After the age of 65, dry eye conditions become more commonplace.
- Hormone changes − For reasons not entirely understood, certain hormone changes result in dry eyes, especially estrogen. Pregnant and post-menopausal women are at greater risk for dry eye problems.
- Diseases − There are several autoimmune diseases where the body attacks its own tissues, consequently leading to dry eyes. Among them are Sjögren’s syndrome, lupus, scleroderma, and rheumatoid arthritis. Inflammatory diseases such as Rosacea and blepharitis can also cause problems. Systemic diseases like diabetes and low thyroid can affect optical tissues and increase the risk of dry eye conditions.
- Optical devices and surgery − Prolonged or improper contacts use and LASIK surgery can lead to dry eyes.
- Medication − The basic premise of drugs is that they alter the body’s performance. It is a rare occurrence where we can wall off the eyes from the effects of the medication we take. Drugs that can cause the side effect or exacerbate dry eyes are antihistamines, decongestants, blood pressure meds, hormone replacements, antidepressants, antipsychotics, and
|
Table 1. Medications Involved in the Etiology of Dry Eye Disease (DED) |
|
|
Medications/therapies/conditions |
Target and/or effect |
|
Drugs with antimuscarinic effects · Antihistamines · Antipsychotics · Anticholinergics (e.g., oxybutin) · Tricyclic antidepressants · Selective serotonin reuptake inhibitors |
Inhibition of cholinergic receptors to lacrimal glands, leading to hyposecretion (reflex motor block) |
|
Beta adrenergic blockers |
Reflex sensory block, leading to tear hyposecretion |
|
Topical anesthetics · Proparacaine drops |
Reflex sensory block, leading to reduction in blink rate and tear hyposecretion |
|
Androgen deficiency, anti-androgen therapy |
Dysfunction of meibomian and lacrimal glands, leading to DED |
|
Elevated estrogen levels, estrogen replacement therapy |
Associated with DED; exact mechanism not clear |
|
Retinoid therapy |
Structural and functional damage to meibomian glands, leading to evaporative losses and increased tear viscosity |
|
Diuretics |
Associated with DED; exact mechanism not clear |
|
Vitamin A deficiency |
Unstable tear film and lacrimal hyposecretion |
|
Oral corticosteroids |
Clinical observation: increased risk of DED |
Source: Stop the Rub: The Treatment of Dry Eyes Catherine A. Opere, Karen K. O'Brien
Prevalence (especially in care homes)
I hope that the course has been interesting so far, but I want to move beyond interesting. The rest of the course is where the rubber meets the road, or, in other words, why you should care about dry eyes as a care home care provider.
It has been estimated that 1/3 of the population will experience some form of dry eye in their lifetime. The prevalence of dry eye is 11% for men and 17% for women. Those figures in and of themselves indicate that the condition is a significant health concern in the general population. But your residents aren’t the general population, are they? They are the weak and infirm. Just compare the list of contributing risk factors and the general condition of your typical elderly resident. It doesn’t take a genius to figure that you’re almost 100% guaranteed to have to deal with multiple cases of dry eyes in your caregiving career. That holds true for Developed Disabled and Mental Health homes as well.
Foster Care Issues
For foster care providers, it’s not a matter of ‘if’ you’ll have to deal with dry eyes; it’s more a matter of ‘when’ it’s going to happen. In my book, it’s always better to be prepared before it happens rather than reacting after the fact.
Monitoring − Be on the lookout for the symptoms of dry eye, especially in those residents with multiple risk factors.
Watch for:
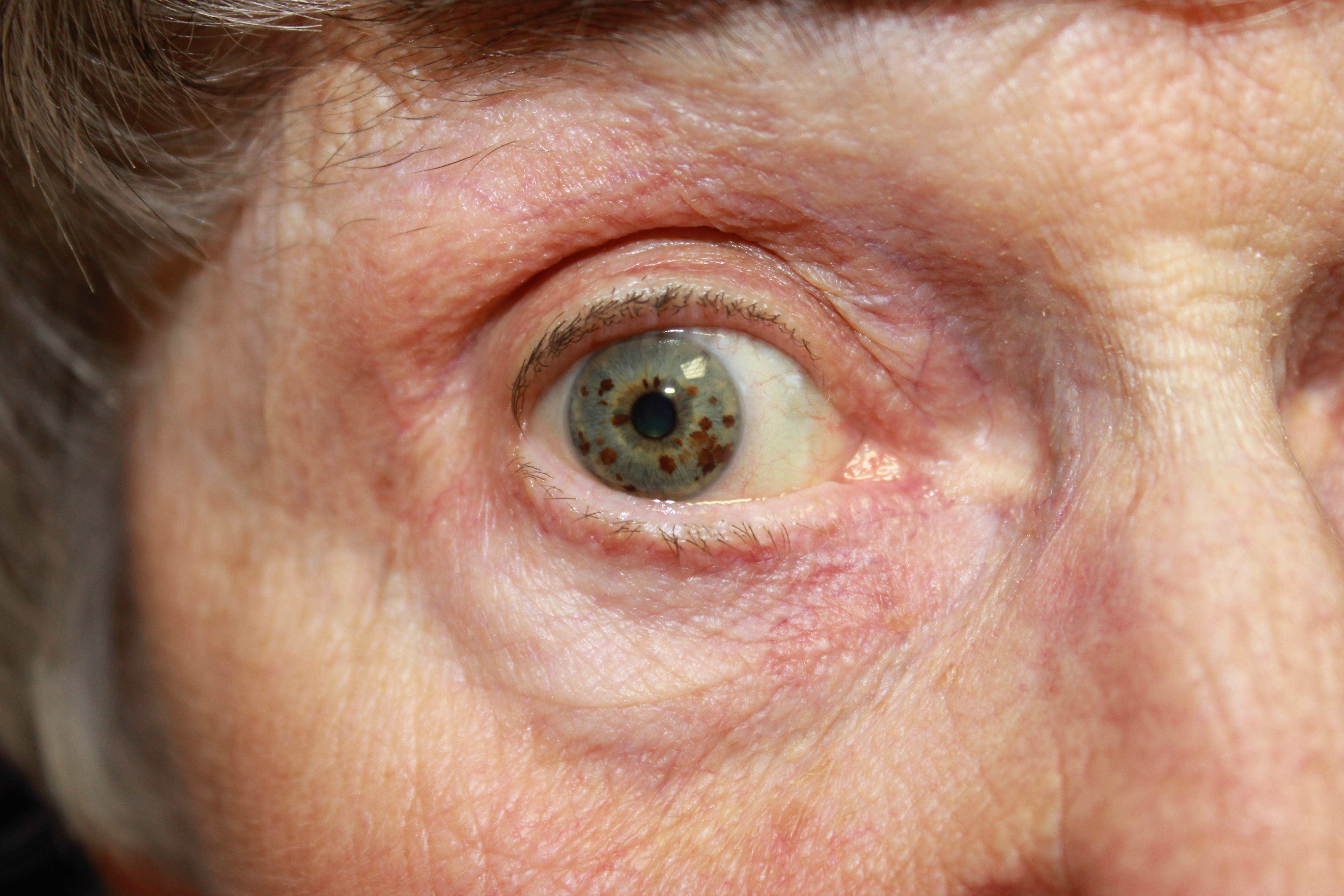
- red, inflamed eyes
- goopy or crusty eyelids
- sagging eyelids that expose the conjunctiva
- sleeping with the eye partially open
- complaints of irritated eyes or tired eyes
- blurred vision
- over-watery eyes (the body’s response to dryness)
- the sensation that something is in the eye
- troubles with contact lens
Therapy − Unlike other disease states, the goal of therapy is not to cure or manage the underlining physiological events, which is quite difficult as mentioned before. The goal is to make the patient comfortable. In care homes, achieving that goal presents some grey areas in caregiving. The lines blur between what is considered basic caregiving, activities for daily living, and therapy. In eye care, what is considered basic caregiving, delegated nursing duty, and medical treatment? For example, is it considered therapy to wash the goop out of crusty eyelids in the morning for residents who sleep with their eyes open? Do you have to get a nurse to delegate putting in over-the-counter eye drops in a resident’s eyes if it’s only done occasionally? In my opinion, it’s a matter of several factors: how often the activity happens, if there is a diagnosis of dry eye disease in the resident’s record, and how severe the condition is. For mild occasional cases, err on the side of good caregiving. For moderate to severe cases, err on the side of medical treatment. As always, when in doubt, err on the side that won’t get you in trouble with county licensors and doctors (better safe than sorry).
If the dry eye symptoms are occurring on a regular basis, get your resident to an eye care professional. Be sure to get clear instructions on what to do back from the doctor and get them into the resident's file and MARS. If they don’t readily cooperate, I suggest the trick of writing what you think is needed and faxing it to the doctor with just a yes or no checkbox attached.
For example,
Instill over-the-counter eye drops as per manufacturer’s instructions PRN in Mary Smith’s eye. ____ Yes, _____ No
Prescriber’s signature _____________________.
Medications
There are very few prescription medications for the treatment of dry eye disease. They mainly stimulate tear production or are anti-inflammatory drugs.
|
Anti-inflammatory or immune system modulators |
|||
|
Generic name |
Brand name |
Dose |
Side effects caregivers should watch for |
|
Cyclosporine |
Restasis |
1 drop in affected |
Relatively well tolerated; the most common side effect is ocular burning (17%); less common are, redness, discharge, watery eyes, eye pain, foreign body sensation, itching, stinging, and blurred vision |
|
Lifitegrast |
Xiidra |
1 drop in affected eye(s) twice daily |
Most common effects (5% - 25%) are instillation site irritation, dysgeusia, and decreased vision effects. |
|
Caregiver administration notes: Contact lenses should be removed prior to application of drops and reinserted no sooner than 15 minutes after administration of drug. Individual dose vial contents should be applied into the eye(s) immediately after opening and remaining contents should be discarded. Side effects most likely will be temporary and manageable but if they interfere with activities of daily living notify the prescriber. |
|||
|
Tear stimulators (used mainly in severe cases due to side effects) |
|||
|
Generic name |
Brand name |
Dose |
Side effects caregivers should watch for |
|
Cevimeline |
Evoxac |
30 mg by mouth 3 times daily; total daily dose should not exceed 90 mg |
Possible side effects include sweating, flushing, increase urination and nausea; side effects occur less frequently with cevimeline than with pilocarpine |
|
Pilocarpine |
Salagen |
5 mg by mouth 4 times daily; total dose should not exceed 10 mg/dose and 30 mg/day |
Common side effects include sweating, increase urination, flushing, headache, and nausea |
You may also see prescribers use ointments occasionally. The ointments prescribed most often are purified petrolatum, or a saline gel. They are commonly used in geriatrics when the resident sleeps with their eyes open or they have severely sagging eyelids. The caregiver concerns that you should watch for are a temporary blurred vision that can lead to falls and interference with other medicated eye drops. It’s just a matter of timing of applications and monitoring the resident after use. Caregivers should instill eye drops before ointments and wait for at least 10 minutes before applying the salve.
Over-the-Counter Artificial Tears
By far, the most common therapy for dry eyes is tear supplementation with over-the-counter artificial tears. We all have used or are very familiar with OTC eye drops. It’s a $2 billion-a-year global industry. One of the caregiving issues with such a prevalent drug product is that some of your residents will be used to applying the product themselves. They are certainly allowed to continue the practice if they want to, but you have to get all the necessary medical permissions and documentation that are required of care homes. Don’t let this one slip by you, or it could come back to haunt you at inspection time.
Another issue that caregivers might have to deal with is product selection. On the off chance the prescriber just writes OTC eye drops PRN, or the resident self-medicates and wants you to buy the eye drops for them, you might have to choose which artificial tear product to purchase. In doing so, there are a couple of factors you need to be familiar with:
- Bacteria and Fungi − Artificial tears are basically standing water. Eventually, microorganisms will grow in it. The more often you handle the container, the greater the chances are that critters are swimming in it. Very old bottles or expired products should be replaced.
- Preservatives − To make the product last longer, manufacturers add chemicals that inhibit microbial growth. Unfortunately, anything powerful enough to kill things off is going to have side effects. For the average person, it’s not going to be an issue. But, like we talked about before, your residents are not the average person. It would be wise for you to read the ingredient list and monitor the resident for side effect issues, even if the doctor or pharmacist made the product selection.
|
Preservatives Used in Artificial Tear Substitutes |
|
|
Preservative |
Comments |
|
Benzalkonium chloride (BAK) |
Can cause cytotoxic effects in eye tissues and disrupt tear film. Try to avoid BAK if possible. |
|
Edetate disodium (EDTA) |
Stimulates allergic and inflammatory responses in ocular tissues; most often combined with other preservatives. If the eye turns red after use look for this in the ingredients |
|
Sodium chlorite |
Considered relatively safe to ocular tissues |
|
Polyquaternium-1 |
Polymeric quaternary ammonium compounds are less toxic than BAK |
|
Sodium perborate |
Considered relatively safe and it eventually breaks down to water and oxygen when it contacts the tears |
- Preservative-free − You can buy preservative-free drops and avoid side effect monitoring altogether. You will notice that those products tend to be more expensive and are single-use Proper storage and application techniques naturally become more critical issues. You will have to read and strictly follow package instructions. Naturally, they expire faster, so you will have to keep track of the expiration date after the purchase.
- Storage − Read the package instruction on how to properly store the product to increase shelf life and to remain bacteria-free, especially if the product is kept in the resident’s room. Single-use vials will be quite bulky. A 90-day prescription will take up a significant portion of your medicine cabinet. Throw away any unused portion of single-use Don’t be tempted to try to use up leftovers to save on costs.
- Frequency of Administration − Some products have longer lasting effects than others. If you find the resident in need of frequent dosing (consult the PRN log), it might be wise to choose another product. Products that have gel-forming qualities last longer in the eye but may also cause temporary blurring. Look for products that have the following ingredients for longer lasting effects: polyethylene glycol, polyvinyl alcohol, povidone, carbopol, polyguar, HP guar, hyaluronic acid and sodium hyaluronate. If the doctor or pharmacist have chosen the product, they will probably be open to suggestion if the eye drops are just not lasting long enough to make the resident's eyes comfortable.
- Contact Lens − If the resident wears contacts, you must read the label instructions concerning contact lens.
- Multi-symptom, Allergy, or Redness Relievers − These products are not designed for chronic dry eye relief, even if the box claims dry eye relief. Prolong use could cause irritations. The extra medications they contain are really for other eye symptoms like allergies. Why take allergy medicine when the problem is something else? You also could get into a lot of trouble. If you chose these products, you could be acting as a doctor and choosing a medication that is not needed. If you have a resident absolutely insisting on a product that is designed for other things, that’s when you get a doctor involved. Who knows, there just might be an underlying problem that the multi-symptom relief eye drops are covering up.
When artificial tears are not enough
There is a drug option for the doctor to choose when the use of artificial tears isn’t doing enough to bring comfort to the patient. It’s an insert that looks like a tiny grain of sand called Lacrisert (hydroxypropyl cellulose). It is placed in the eye once a day. As it slowly dissolves, it releases chemicals that can lubricate the eye. If artificial tear therapy is failing, you could ask the doctor if Lacrisert is an option. There are also surgical options: plugs that block the tear ducts from flowing into the nasal cavity and making tear supplements from the patient’s own blood. All of the above are expensive and quite involved, so they are reserved for very serious cases.
Non-drug Therapies
The environment the resident lives in has a huge impact on dry eyes. It is the area the caregiver has the most control over. Dry Eye Disease can be minimized by paying attention to the environment immediately around the patient. Here is a checklist of caregiving activities for you to go through periodically:
- Eliminate tobacco or other smoke.
- Divert air drafts from the face. Check heaters, air conditions, fans, furnace outlets, and wind from windows. Wraparound sunglasses and safety glasses are great for direct draft protection for the eyes and for outdoor activities.
- Increase ambient humidity by the use of well-placed humidifiers.
- Interacting frequently with the resident—this interrupts concentration, which increases the blink rate automatically while they are diverted.
- For patients with paralysis conditions like Parkinson’s disease and Bell’s Palsy, it might be wise the actually tell the patient to blink.
- Lowering computer and TV screens automatically lowers the gaze position of the eyes naturally, decreasing the rate of tear film evaporation from the eye surface.

Caregivers should pay attention to eyelid hygiene. Wash the eyelids regularly with a mild soap. It removes the eye goop that can interfere with tear production. No-tears baby shampoo is great for this task. Massage gently the eye with a warm soft cloth or towel to stimulate the meibum gland flow. Of course the resident could do this by themselves, but I recommend the caregiver at least supervise the activity. The task becomes easier if you stick a clean cloth in the resident's shirt pocket. Then it becomes more convenient to massage the eye several times a day.
Medication Administration Techniques
There are right and wrong ways to instill eye medications. Regardless of how you or the resident has used eye products in the past, the following are the tried and true medication administration techniques that should be used. They will ensure the medication gets to where it is needed with the fewest concerns.
The patient:
- Tell the resident what you are about to do.
- Place the patient in a stable sitting or lying position.
- Make sure there is adequate lighting to safely accomplish the task.
- Assess the eyes and clean the area as necessary. Use baby shampoo for heavier encrustations. For lighter accumulations, eye contact saline solutions and clean bandage gauze will do. Gently move the gauze from the nose outward toward the ear.
- The caregiver should wash their hands before and after the medication administration procedure.
- Remove contacts if required.
- After administration, chart in the MARs as needed and record any side effects that occur.
The medication container:
- Check on the expiration date of the product
- Inspect the nozzle of the bottle for damage
- Do not touch the tip of the container
- Shake suspensions before use
Eye Drops:
- Tilt the head back and lower the eyelid slightly to expose the conjunctiva
- Hold the bottle upside down and instill drops into the conjunctival sac
- Close the eye or allow the resident to blink
- Following administration, wipe excess tears from the eye with a clean tissue
Gels and Ointments:
- Tilt the head back and lower the eyelid to expose the conjunctiva.
- Squeeze a thin ¼ to ½ inch ribbon of the preparation into the lower conjunctiva.
- Do not touch the tip of the container to the patient. Stop squeezing the tube and pull it quickly down and away from the patient in a fish hook motion. This will naturally break the ribbon of gel.
- Close the eye and allow the resident to blink.
- After a minute or two, remove excess ointment with a clean tissue.
- Make sure vision has cleared before allowing the resident to get up.

Conclusion
The eyes are complex bodily structures that are lubricated and maintained by equally complex solutions we call tears. When there are not enough tears, or the tears are of poor quality, dry eye conditions manifest themselves. If the condition becomes chronic or severe, permanent damage can occur to the eye. Due to multiple risk factors, residents in care homes are at greater risk of suffering from dry eyes. Caregivers in care homes should be able to recognize those who are at greater risk and monitor for dry eyes. Caregivers should also help maintain good eye care hygiene. Most often dry eyes are treated by altering environmental conditions and the use of artificial tears.
The caregiver should be able to keep their residents comfortable by understanding what affects their resident’s eyes to make them dry. Also, they should know how to select and use artificial tears and eye ointments and monitor for side effects. I hope this CE course has helped you in your eye care efforts.
As always, good luck with your caregiving!
Mark Parkinson BS Pharm
References:
Catherine A. Opere, B Pharm, Karen K. O'Brien, PharmD. Stop the Rub: The Treatment of Dry Eyes. Power-Pak.CE.com. Dec.16, 2016. https://www.powerpak.com/course/content/113825
Markk B. Abelson, MD,. 3, 500 Years of Artificial Tears. Review of Ophthalmolog. Dec. 8 2014. https://www.reviewofophthalmology.com/article/3500-years-of-artificial-tears
Dry Eye. American Optometric Association. https://nei.nih.gov/health/dryeye/dryeye
Dry Eys. Mayo Clinic http://www.mayoclinic.org/diseases-conditions/dry-eyes/basics/definition/con-20024129
Dan Alalouff. Dry Eye Syndrome. Nursing In Practice Feb 3 2012 https://www.nursinginpractice.com/article/dry-eye-syndrome
Gail P. Mooney, MSc,. Eye Care. Nursing Times. Jun 21 2007https://www.nursingtimes.net/clinical-archive/assessment-skills/eye-care/199389.article
Exam Portal
click on [Take Exam]
Purchase membership here to unlock Exam Portal.
|
|
|
|
|
*Important*
Registration and login is required to place your name on your CE Certificates and access your certificate history.
Username MUST be how you want your name on your CE Certificate.
| Guest: Purchase Exam |


