Dealing with Migraines
Dealing with Migraines
Author: Mark Parkinson BsPharm: President AFC-CE
Credit Hours 2- Approximate time required: 120 min.
Educational Goal
Provide instruction about the Migraine disorder and how care to for residents who suffer from Migraine headaches
Educational Objectives
Provide migraine statistics
Define Migraine disorder and improve caregiver understanding
State the need a bridge between migraine suffers and proper care
Tell about the management principles of the Migraine disorder
Procedure:
Read the course materials. 2. Click on exam portal [Take Exam]. 3. If you have not done so yet fill in Register form (username must be the name you want on your CE certificate). 4. Log in 5. Take exam. 6. Click on [Show Results] when done and follow the instructions that appear. 7. A score of 70% or better is considered passing and a Certificate of Completion will be generated for your records.
Disclaimer
The information presented in this activity is not meant to serve as a guideline for patient management. All procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this article should not be used by care providers without evaluation of their patients’ Doctor. Some conditions and possible contraindications may be of concern. All applicable manufacturers’ product information should be reviewed before use. The author and publisher of this continuing education program have made all reasonable efforts to ensure that all information contained herein is accurate in accordance with the latest available scientific knowledge at the time of acceptance for publication. Nutritional products discussed are not intended for the diagnosis, treatment, cure, or prevention of any disease.
Dealing with Migraines
Making a difference in the lives of the most needy is what helps foster care providers get up each morning and face a new day. Sometimes, though, a caregiving challenge arises that seems overwhelming. Boy, I hated those days when I was a caregiver. Everyone looks at you like you’re some kind of miracle worker that should know what do to solve any problem.
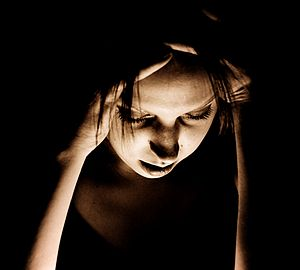
What do you do when the caregiving challenge is a resident with a headache so severe that it causes nausea and vomiting? What do you do when someone in your charge develops a searing, debilitating, throbbing head pain that almost totally incapacitates them? What do you do when the headaches happen over and over and over again despite your best efforts? That’s the foster caregiving nightmare called a migraine headache. What do you do about migraines? You get busy and learn about them and how to best manage them.
Migraine Facts
Prevalence
Migraine is a very common neurological disorder of the brain. It afflicts 39 million people in the U.S. and 1 billion worldwide, making it the third most prevalent illness in the world. In the United States, 12 percent of the population suffer from migraines. It is estimated that one in four households includes someone who has endured a migraine.
Gender
Men, women, and children can suffer from a migraine. In America 18 percent of women, 6 percent of men, and 10 percent of children have experienced an episode. Adult women are three times more likely than men to have a migraine. Up to 30 percent of women will have at least one episode in their lifetime.
Migraine can occur at any age, with cases having been reported in children as young as 18 months. Migraine headaches occur most frequently between the ages of 18 to 44. Before puberty, boys are affected more than girls, but during adolescence, the risk of migraine and its severity rises in girls. Half of all migraine sufferers have their first attack before the age of 12. After the age of 50 the frequency of headaches and the severity of the episodes seem to reduce.
Genetics
Migraines tends to run in families. Ninety percent of sufferers also have a family history of occurrences. Children who have one parent suffering from a migraine have a 50 percent chance of having one too. The chance of occurrence for a child who has both parents with a history of migraines increases to 75 percent.
Frequency
Every 10 seconds, someone in the U.S. goes to the emergency room complaining of head pain, out of which approximately 1.2 million visits are for acute migraine attacks. More than 4 million people have chronic daily migraines, with at least 15 migraine days per month. However, most patients only have 1 or 2 a month.
Costs
 It is estimated that migraines cost the U.S. economy 20 million a year due to direct health costs and lost time, though that figure could be a lot higher. Fewer than 5 percent of patients are seen by a healthcare provider, receive a proper diagnosis, and receive appropriate care.
It is estimated that migraines cost the U.S. economy 20 million a year due to direct health costs and lost time, though that figure could be a lot higher. Fewer than 5 percent of patients are seen by a healthcare provider, receive a proper diagnosis, and receive appropriate care.
More Than Just a Headache
Handling the nightmare that is migraine starts with gaining a proper caregiver perspective on what it is. Most of what  you probably know about migraine comes from popular cultural references and is probably wrong. Despite what caregivers have been told, migraine is not just a severe headache that comes and goes. It is a primary brain disorder that causes a headache. Even how you use the word is probably wrong. “I’m having a migraine” is no more accurate than saying “I’m having diabetes.” It is not an event, it is a condition.
you probably know about migraine comes from popular cultural references and is probably wrong. Despite what caregivers have been told, migraine is not just a severe headache that comes and goes. It is a primary brain disorder that causes a headache. Even how you use the word is probably wrong. “I’m having a migraine” is no more accurate than saying “I’m having diabetes.” It is not an event, it is a condition.
The migraine disorder is not fully understood yet by medical science. It most likely involves how the nerves and blood system of the brain develop in certain parts of the brain. Overactive or overly sensitive nerves send out signals to the trigeminal nerve, a major nerve that supplies sensations to the head and face. In turn, the trigeminal nerve stimulates other reactions including the release of chemicals that cause blood vessels in the lining of the brain to swell. The inflammation greatly contributes to the pain experienced in a migraine headache. This condition makes patients with migraine more suspectable to biological and environmental triggers that result in a special kind of moderate to severe headache called a migraine headache. There may yet be other contributing factors that remain undiscovered.
Having a migraine may be an inaccurate way to describe what is actually going on, but the concept is so ingrained in our society that there is little point in trying to correct it. As long as the caregiver starts off with the proper understanding, therapeutic efforts can be more effective. From now on in this article if I say “having a migraine” you’ll know what that I really mean.
Migraine Headaches
Migraine headaches are different from regular headaches. How you recognize them, how you treat them, and how you prevent them is all different. You don’t just give a resident an aspirin when the migraine comes on and expect that everything will be okay, because it won’t be. Fortunately, there are ways to manage migraines if caregivers can spot them and know what to do.
Recognizing Migraines
There is significant variability in how migraine headaches are experienced. There are patterns in the signs and symptoms, though, that set apart migraines from regular headaches. Typically, migraine headaches are felt on one side of the head, are throbbing, and can last from a few hours to three days. Often other symptoms accompany the headache; these may include nausea, vomiting, and sensitivity to light, sound, or smell. The pain is generally made worse by physical activity. Also, migraine headaches occur in phases. Certain signs and symptoms may happen before, during, and afterward the migraine. There are also predictable events that trigger the onset of a migraine. The phases of a migraine are:
Prodrome phase
Because the brain controls many things, when migraine disordered cells are triggered, other bodily effects can result before a headache occurs. Prodromal symptoms can be seen in up to 60 percent of patients. They can occur between two hours to two days before the pain phase and can be used as a sign that a migraine is coming on. The symptoms are as varied as individuals are, so it’s best to keep tract of events before the migraine comes on. Look for things like altered mood, irritability, depression or euphoria, fatigue, cravings for certain foods, stiff muscles (especially in the neck), constipation or diarrhea, and sensitivity to smells or noise.
Aura Phase
Up to one-third of people with migraine headaches experience what is called an aura — a short period of sensory disturbances that signals that the headache will soon occur. They usually last less than 60 minutes. Ninety-nine percent of aura cases involve impaired visual effects. Other sensory disturbances are seen in about 30–40 percent of auras.
Visual auras often affect just a portion of the field of vision and can flicker in and out. They can appear as zigzagging lines of black or white that start in the center of the field of vision and extend outward. Others experience blurred spots, while others lose a portion of the visual field. All visual auras can affect the resident’s ability to perform visual tasks.
Other sensory disturbances can be feeling pins and needles in the skin on one side of the body, starting at the hand and traveling up toward the nose and mouth area. Numbness usually follows. Some patients describe tasting, smelling, seeing, or hearing things that are not there. Also, language problems and dizziness may temporarily appear.
Rarely, an aura can occur without a following headache. Known as an acephalgic or silent migraine, they can be used as an indication of the migraine disorder.
Pain Phase
This is when the actual headache starts. It begins gradually and pulses into greater intensity. Because inflamed cranial blood vessels are involved, anything that makes blood pressure and flow increase, like physical activity, will make the throbbing pain worse. Typically, the pain is only felt on one side but over 40 percent of cases experience pain on both sides. Less commonly, pain may occur primarily in the back or top of the head. The pain phase can last from four to 72 hours. In younger children, the pain phase often lasts less than one hour.
As the headache intensity grows, other symptoms start to appear. In 90 percent of cases, nausea is felt, with one-third of those resulting in vomiting. The patient is aggravated by light, sounds, or smells. Dizziness, scalp tenderness, lightheadedness, confusion, blurred vision, nasal stuffiness, diarrhea, frequent urination, pallor, or sweating may also occur. These additional symptoms appear less frequently in the elderly.
Postdrome Phase
After the migraine headache resolves, rebound symptoms can occur, like weakness, confusion, mood changes (including euphoria), GI disturbances, and tenderness in the headache area. It has been described like being hung over and can last for several days. The emotional response can range from feeling refreshed or euphoric to general malaise and depression.
A final distinction in migraine is that it is a brain function disorder and is often associated with other brain function maladies. They can include major depression, bipolar disorder, anxiety disorders, and obsessive-compulsive disorder. These psychiatric disorders are approximately two to five times more common in people without aura, and three to ten times more common in people with aura than the general public.
Triggers
There are a number of things that can set off the cascade of cellular events that can lead to migraine headaches. They include:
- Hormones in women – Changes in the estrogen levels in women seen in menstrual periods, pregnancy, and menopause can trigger migraines and affect their severity. Medications that include hormones, like oral contraceptives and hormone replacement therapy, can also worsen migraines. Some women, though, find that taking hormones decreases the number of migraines they experience.
- Drinks – Drinks that contain alcohol and caffeine affect brain cells and thus are known triggers for migraine headaches.
- Stress – Increases in mental and physical stresses.
- Overstimulating the senses – Bright lights, glaring sunshine, loud sounds, strong smells, and secondhand smoke can all set off migraine-sensitive nerves.
- Changes in sleep patterns – Migraines can be triggered by getting too much sleep, not enough sleep, or jet lag.
- Physical activities – An increase in activity increases several brain functions including migraines. Feeling fatigued can also be a factor.
- Weather changes – A change of weather or barometric pressure can bring on a migraine.
- Medications – It is a given that drugs that affect hormone levels and blood pressure will affect migraine occurrences. They include oral contraceptives, vasodilators, and nitroglycerin.
- Foods and food additives – Ingredients in certain foods like aged cheeses, salty and processed foods, aspartame, and monosodium glutamate (MSG) have been observed in triggering headaches. There is also a link through the gut-brain axis and how our intestinal flora reacts with food that can send signals to the brain that will trigger a migraine.
Being the Bridge to Proper Care
It is one thing to make an overall list of the signs, symptoms, and triggers of migraine, but it’s a totally different thing diagnosing and treating the individual. If medical science doesn’t have a complete handle on what migraine disorder is, then the general public is particularly clueless. That is one of the reasons why only 5 percent of migraine patients receive proper treatment. Foster care providers can help fill the understanding gap that will lead to more patients receiving more appropriate care. It starts with recognizing that the moderate to severe headache that the resident is experiencing might be something more.
So, how can a caregiver tell a migraine headache is coming on and not just a regular headache? The answer? Being an expert on your residents and recognizing the migraine pattern of symptoms and behaviors.
- First, recognizing who’s most likely to have migraines. Pay attention to patient files and family histories. If there is a history of migraines, then those are the ones that are most likely to have future migraine headaches.
- Second, recognizing repeating events. If the patient does have oversensitive nerves, then headaches will occur frequently. You will notice that they may be triggered predictably by certain events.
- Third, recognizing the patterns in the headaches, including what happens before and after the headache. Remember, migraine headaches occur in phases.
The Diagnosis
 One of the great things about being a foster care provider is that we don’t have to come up with a diagnosis. All we have to do is suspect that the resident has migraine; the doctor has to make the diagnosis call. When our suspicions prove true, then we look like a hero for catching something that no one else did (that’s particularly satisfying, in my opinion). If the doctor doesn’t agree with your guess, it’s no big deal. Don’t stop monitoring; doctors have been known to be wrong before.
One of the great things about being a foster care provider is that we don’t have to come up with a diagnosis. All we have to do is suspect that the resident has migraine; the doctor has to make the diagnosis call. When our suspicions prove true, then we look like a hero for catching something that no one else did (that’s particularly satisfying, in my opinion). If the doctor doesn’t agree with your guess, it’s no big deal. Don’t stop monitoring; doctors have been known to be wrong before.
According to the International Headache Society, a migraine diagnosis can be made according to the following "5, 4, 3, 2, 1 criteria."
- Five or more attacks — for migraine with aura, two attacks are sufficient for diagnosis.
- Four hours to three days in duration
- Two or more of the following:
- Unilateral (affecting half the head)
- Pulsating
- Moderate or severe pain intensity
- Worsened by or causing avoidance of routine physical activity
- One or more of the following:
- Nausea and/or vomiting;
- Sensitivity to both light (photophobia) and sound (phonophobia)
I think it is important to point out a few things about this subject.
- The vast majority of migraine sufferers have not been properly identified, diagnosed, and treated. That means most
 will want to just hide in a dark, quiet place or go to the ER.
will want to just hide in a dark, quiet place or go to the ER. - Some, like mental health patients, developmentally disabled, and children who have communication problems, have never properly described what they are experiencing. You’ll have to do it for them.
- Those who have experienced multiple migraines will be engrained in a particular line of thought on what it is and what it is not. Their migraine reality is shaped by the fear of a painful headache episode. Going outside their comfort zone will be very hard because of the fear of that pain.
- Patients will have only called their doctor in the middle of a headache demanding an immediate remedy. Most likely, not much effort will have been made in treating migraine like a disease; rather, it’s treated like an emergency event.
- There is a tendency of inexperienced doctors to not diagnose migraines unless there is an aura. Gently remind the doctors that the majority of migraines are without aura, or ask questions about all the other symptoms that you see. For example, “What about the light sensitivity and nausea, doctor, what is causing that?”
- Not every migraine patient will have every phase of migraine.
Have patience with the resident, the family, and the doctor. Be the bridge between what is now happening and what needs to be happening in the future in regard to migraine disorders.
Caregiving in Migraine
There may be headache relievers but there is no cure for migraine, just management — management of the triggers, management of the patient, and management of the headache. The key to successful migraine management is you, the in-home caregiver. You are in the best position to manage all the factors that can reduce the severity and frequency of migraine episodes. The following are a few helpful suggestions and resources that I believe will be beneficial to your caregiving efforts.
Frame of Mind
Start off and continue in the right frame of mind: empathic, supportive, and flexible. Everyone experiences migraine differently and may need different kinds of support. Treatments may vary from medication, chiropractic care, alternative medication, special diets, or whatever. If it works, run with it. Don’t forget about expecting and managing the other the symptoms involved in migraine, for example vomiting. Remember, migraine is a disorder, not an event. Your emotional support during headaches will be very important.
Management of Triggers
Getting In-the-Know
The more involved you become in understanding your resident’s condition, the more likely you will be able to affect the course of the disease. A Migraine Diary will be a very effective caregiving tool in getting in-the-know. There are several free versions, or ones available at very low cost. Most are easily adaptable to a care home setting. They are designed to help identify what triggers a migraine and measure how effective therapy is. Doctors will love you if you send them patients with a filled-out migraine diary.
Check this one out, written by Hartford Healthcare.Org https://hartfordhealthcare.org/File%20Library/Services/PDFs/Headache-Center-Diary-and-Guide.pdf
The Menu
Cooking recipes from scratch helps manage ingredients that trigger migraine attacks. It will help you avoid having to prepare completely separate trigger-free meals. Nitrates, commonly found in processed meats, can be an issue. There are nitrate-free versions; you just have to look for them. Save time and just ask the grocer or butcher where they are. Once you get a good handle on food triggers, educate family members who want to bring food gifts or take their loved ones out to dinner.
Take Regular Walks
Those who read my CEs know how much I tout the benefits of taking residents for regular walks. It turns out walks are recommended for migraine trigger management, too. Mild physical activity reduces stress, a migraine trigger. It also strengthens the blood flood gradually. Those who regularly exercise become more capable of handling sudden demands on blood flow, also a known trigger of migraines.
Triggers Are Accumulative
Not all trigger events cause a migraine every time. The explanation is there seems to be a stimuli threshold that has to be crossed before migraine-effected brain cells are set off. So, if the resident accidently eats a trigger ingredient, manage all the other triggers and you might avoid the migraine. Also, if there is an increase of uncontrollable triggers like the weather or menstrual periods, be ready with extra trigger control.
Management of the Patient
Classification
Migraines are classified into several subclasses. A list of them is not that important right now, though if you do see the subclass name it might give you clues on how to manage the resident. The classifications I want to concentrate on is acute versus chronic. In the case of migraine, acute is defined as present or experienced in an intense, severe way. On the other hand, chronic is defined as having three or four acute attacks per month. These labels will help determine what medication is used. Everyone will get an abortive agent(s), which is the headache remedy. Chronic migraine sufferers might get a prophylaxis agent, which is a preventative medication. I was going to give you a list of meds but I will spare you from reading a long, boring list. Instead, I will give you a list of helpful caregiver medication management hints.
I know the PRN log is a pain to fill out, but in migraine it can give you very useful info. How often PRN meds are charted tells a lot about how migraines are experienced. It also helps alert you to overuse, which can actually lead to more migraines (ironic, isn’t it?). It might also be an indication that a med routine change is needed. It would be wise to get a “call the doctor” point in the frequency of PRN drug use from the prescriber.
When to Dose
Abortive agents work better if given early on. It’s easier to put out a one-alarm fire than a five-alarm fire. Don’t wait too long to give PRN meds.
Statistically, the onset of most attacks of migraine occur in the morning when you’re the busiest. The migraine may even have started before the resident woke up, so the early warnings may not be there. Be more aware of migraine symptoms in your morning routine and be ready with the abortive meds.
Preventative Medication Considerations
Medication used to prevent migraines will be familiar to you but applied in a different way. When a preventative medication is started, the doctor might begin with a fairly low dose and gradually increase the amount used depending on the patient’s response or side effects that occur. Feedback to the doctor is pretty important at this time. Monitor for effect with skill. In many instances, these agents are not used long enough. Frustration on the part of both the physician and the patient leads to frequent changing of medications. Some of these preventive agents, particularly verapamil and divalproex sodium, may take six to eight weeks before one sees a significant reduction of headache frequency and severity. Often patients have their drugs changed every couple of weeks and never give the medication an adequate trial. You can help by asking questions about sufficient trial times for each medication. Consulting a pharmacist might also help get the point across.
In migraine prevention, higher doses of calcium channel blockers and beta-blockers are needed than are used in treating hypertension so watch for side effects. Also, in tricyclic antidepressants, lower doses are used than what is seen in treating depression.
Many migraine relief medications contain aspirin (like Excedrin Migraine). Children and aspirin-containing products don’t mix well. The worry is about causing Reye’s syndrome. If you take care of infants, read the ingredients of all your headache remedies. If aspirin is present, bring it to the attention of the doctor. Educate family members not to give these products when the resident is with them.
Migraine Prevention Devices
There are nerve stimulation devices that are FDA-approved for migraine prevention. Insurance coverage is going to be an issue. The good thing is that there are no side effects and they can be used for children and teens.
Management of the Headache
Caregiver Tools for Headache Management
Once the migraine is triggered, caregivers have to switch gears from prevention to controlling the pain and other symptoms that you know are coming. The pressure is on you, the caregiver — not the doctor, not the home health nurse, and not the family. Here are a few ideas that I think will help you manage the headache.
Monitoring for Effect
Because of the PRN nature of headache remedies, you will have to use skill in when to apply them. That skill is developed as you pay attention to how effective the remedies are. The Migraine Diary is an essential tool in this effort. Record what you did and what effect it seemed to have. Include time frames as well. Review the records and discuss them with the resident and the doctor. Over time you can develop an effective treatment regime.
Stimulus Control
Now is the time when you have to control or eliminate all the things that can aggravate the headache that is coming on. Establish a place that is cool, quiet, and dark. Don’t make any demands on the resident and provide plenty of stress-free emotional support.
Drug Considerations
If the doctor has not spelled out a drug regime for migraine, get one. It should be more than just PRN Excedrin. Develop a more detailed plan. It’s going to be a work in progress as you report back to the doctor what works and what doesn’t. Don’t forget nausea control in the regime.
For headaches that happen at least 15 times per month, ask the doctor if medication overuse is contributing to the headache. If it is, it’s going to take two to six weeks to taper off the meds to get things under control again.
Non-Drug Therapies
Drugs are first-line therapies, but they are not the only tools in your caregiver toolbox. The following may or may not be thought of as therapy. When in doubt, get the doctor to add them to the PRN migraine management orders.
- Many people find that putting gentle pressure on the head, face, and neck during a migraine can help ease the pain.
 Techniques to try:
Techniques to try: - Press your brow line and under your eyes.
- Rub your temples and jaw in a circular motion.
- Massage the base of your skull with a tennis ball.
- A variety of head wraps and bands claim to ease migraine pain. They're inexpensive and might be worth a try.
- Relaxation techniques.
- Migraine masks. These are specially shaped cold packs worn over the face. A supply of cool compress rags would have a similar effect.
- Aromatherapy (lavender oil might help).
- Massaging the muscles in the neck and shoulders can help to relieve tension and alleviate migraine pain. Massage may also reduce stress.
- Residents can be given a tennis ball and use it for self-massage along the shoulders and back.
- Acupressure: application of pressure to specific parts of the body. Stimulating specific points of the body in this way is believed to release muscle tension and alleviate pain.
“One popular pressure point is the LI-4 point in the space between the base of the left thumb and pointer finger. Applying firm but not painful circular pressure to the LI-4 point, using the opposite hand for 5 minutes, may relieve headache pain. A 2012 study looked at 40 people who had migraines without aura. It found that pressure on the PC6 acupoint, which is located three fingers up from the base of the wrist on the inside of the arm, was effective in relieving migraine-associated nausea or vomiting associated with a migraine headache.”
Source https://www.medicalnewstoday.com/articles/322814.php#3
Conclusion
Dealing with a headache is not fun. Dealing with a migraine headache is particularly debilitating and those who suffer will need help. A resident who has migraine disorder is going to need caregiver management of their triggers, the prevention therapies, and the migraine headache themselves. Adult foster care providers will find that they are in a powerful position to manage all aspects of the disease that is called migraine. Remember, it is not an event, it’s a disorder.
As always, good luck in your caregiving efforts.
Mark Parkinson, BsPharm
References:
By S. Jähnichen (talk) - File:Brandenburger_Tor_Blaue_Stunde.jpg, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=6668865
Migraine, MayoClinic 2019. https://www.mayoclinic.org/diseases-conditions/migraine-headache/symptoms-causes/syc-20360201
Migraine Research Organization 2019. https://migraineresearchfoundation.org/about-migraine/migraine-facts/
Migraine Diary. Hartford Healthcare,org. https://hartfordhealthcare.org/File%20Library/Services/PDFs/Headache-Center-Diary-and-Guide.pdf
Migraine Headaches. WebMD. 2019. https://www.webmd.com/migraines-headaches/migraines-headaches-migraines#1
Migraine. Wikipedia. 2019. https://en.wikipedia.org/wiki/Migraine
How to Support Someone with Migraine. Migraine Foundation. https://cdn2.hubspot.net/hubfs/2611652/How%20to%20Support%20Someone%20with%20Migraine.pdf
Sai NR Chandamuri, MD, James Abbey, MD, Jesse Vance, PharmD. Migraine Headaches. InfantRisk Center, Texas Tech University Health Center. https://www.infantrisk.com/content/migraine-headaches
Migraine and Tension Headache Guideline. Kaiser Permanente.
https://wa.kaiserpermanente.org/static/pdf/public/guidelines/headache.pdf
Lifestyle Strategies That Might Help Your Migraine. WebMD. https://www.webmd.com/migraines-headaches/common-headaches-17/migraine/slideshow-nondrug-migraine-relief
Nicole Galan. What are some tips for instant migraine relief? MedicalNewsToday. Aug. 20, 2018. https://www.medicalnewstoday.com/articles/322814.php#3
Exam Portal
click on [Take Exam]
Purchase membership here to unlock Exam Portal.
|
|
|
|
|
*Important*
Registration and login is required to place your name on your CE Certificates and access your certificate history.
Username MUST be how you want your name on your CE Certificate.
| Guest: Purchase Exam |












