Hemorrhoids the Bottom Line
Hemorrhoids, The Bottom Line
Author: Mark Parkinson RPh: President AFC-CE
Credit Hours 2- Approximate time required: 120 min.
Educational Goal:
To educate Adult Foster Care providers about hemorrhoids.
Educational Objectives:
Define hemorrhoids.
Present the signs and symptoms of hemorrhoids.
Instruct about the non-serious nature of occurrences
Provide caregiving and follow-up instructions
Procedure:
Read the course materials. 2. Click on exam portal [Take Exam]. 3. If you have not done so yet fill in Register form (username must be the name you want on your CE certificate). 4. Log in 5. Take exam. 6. Click on [Show Results] when done and follow the instructions that appear. 7. A score of 70% or better is considered passing and a Certificate of Completion will be generated for your records.
Disclaimer
The information presented in this activity is not meant to serve as a guideline for patient management. All procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this article should not be used by care providers without evaluation of their patients’ Doctor. Some conditions and possible contraindications may be of concern. All applicable manufacturers’ product information should be reviewed before use. The author and publisher of this continuing education program have made all reasonable efforts to ensure that all information contained herein is accurate in accordance with the latest available scientific knowledge at the time of acceptance for publication. Nutritional products discussed are not intended for the diagnosis, treatment, cure, or prevention of any disease.

Hemorrhoids, The Bottom Line
For a caregiver not too many events can cause more concern than finding blood coming from the bottom of one of your residents. What’s causing the blood to flow? Is it a minor scratch, a bad infection, or is it a symptom of something really serious like cancer? This has happened to me several times in my caregiving career. We sent the patients to the doctor and waited anxiously for the diagnosis. Most of the time, the diagnosis came back as a case of hemorrhoids. I remember the first time I had to deal with a case of hemorrhoids. I thought, “What’s a hemorrhoid and how am I supposed to take care of that? You can’t exactly put a Band-Aid on their bottom, can you?”


Definition
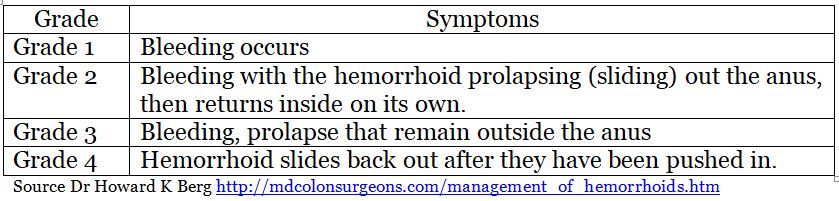
Hemorrhoids are swollen veins around the anus and lower rectum. They look like lumps of discolored purplish flesh giving rise to their other name, piles. There are two places where hemorrhoids form. The first is just under the skin around the anus. These are called external hemorrhoids. External hemorrhoids are usually asymptomatic and don’t cause any problems. The second place they are found is inside the rectum. These are called internal hemorrhoids. Internal hemorrhoids have several grades based on the severity of the symptoms experienced by the patient.
Both kinds of hemorrhoids are typically not serious. Often they resolve spontaneously within about a week. Sometimes when the swelling goes down, a skin tag (excessive skin) is left behind.
Signs and Symptoms
A physical description is not much use to an in-home caregiver. You’re not likely going to inspect your client’s bottom - that’s just plain weird. You can, though, be on the lookout for the outward signs of hemorrhoid trouble.
- Bright red bleeding when bearing down during bowel movements. Often painless.
- Leakage of feces and or poor control of defecation.
- Itching, irritation, pain, or discomfort in the anal region.
- Inflammation around the bottom causing difficulty in sitting.
- Sudden severe pain in the rectum caused by blot clot from pooled blood in external piles.
- Pain and irritation that resolves itself in about a week or less. Inflammation may take longer.
- Internal hemorrhoids can prolapse when straining. Wiping prolapse can cause damage to the delicate surfaces and cause profuse bleeding - a rare occurrence.
- A lump appears around the anus region that can be sensitive.
Causes and Risks
Everyone has the potential to get hemorrhoids because of how humans are built. Since up to 75 percent of humans may experience them in their lifetime, it has been speculated that this is just the price we must pay for being upright beings. We are subject to the pull of gravity that puts pressure in the anal region. The reason engorgement and swelling sometimes occurs in the rectal veins is not clearly understood. What is understood is that there is an increase in pressure in the lower rectum. Increases in pressure are caused by:
- Straining during bowel movement
- Chronic constipation or diarrhea
- Prolonged sitting on the toilet
- Obesity
- Anal sex
Skin and tissue tone weaknesses can also lead to engorgement. Age is definitely a risk factor and so is anal surgery. Other risk factors include events that force a lot of sitting like wheelchair- bound patients or paralysis victims. Of course, any lifestyle choices that lead to any of the above could be considered risk factors for hemorrhoids. For example, a low-fiber diet that leads to constipation or chronic use of diarrhea medicine as seen in anorexia and bulimia sufferers put these residents at greater risk.
Seriousness
Any time blood comes from the bottom, it’s a cause for concern among caregivers. Too many serious problems can cause rectal bleeding. It would be wise when blood or pain appears to send patients to the doctor just as a matter of course. If the diagnosis comes back as hemorrhoids, then caregivers can relax a bit. Most occurrences are not serious and considered minor problems by health professionals. According to one expert, Dr. Howard K Berg of the University of Maryland St. Joseph Medical Center, “treatment for hemorrhoids is only undertaken if they are truly symptomatic. The mere presence of hemorrhoids is not an indication for any therapeutic intervention.”
What’s a caregiver to do then?
Don’t be surprised if the doctor does little or nothing at all. The doctor knows that most cases will go away by themselves within a week. Caregiving mainly deals with patient comfort issues. This is where you as a patient advocate might have to kick up a bit of a fuss. If your patient is uncomfortable and needs attention and the doctor has done nothing, remind the doctor that you can’t treat the patient without doctor’s orders. That includes minor over-the-counter comfort therapy for hemorrhoids. It may be minor to a doctor but they still have to do something about it. If the doctor can’t be bothered with such trivial occurrences, get his nurse or even a home health nurse to follow up and get you the necessary orders.
When does it become serious?
Complications that can turn a minor irritation into a more serious concern are very rare, but you should know about them anyway. Events that require further medical intervention are:
- Anemia - Chronic blood loss causes a shortage of oxygen carrying red blood cells. Caregivers should watch for unusual pale skin, fatigue, and weakness. The resident won’t have their usual zip and appear to be uncooperative.
- Strangulated hemorrhoid - The blood flow to internal hemorrhoids could get cut off, leading to tissue death (necrosis). In the bacteria- rich environment of passing stools, an infection could easily set in (gangrene). Caregivers should manage prolapsed hemorrhoids as instructed and not ignore them.
- Thrombosis - Blood can pool in swollen hemorrhoids and coagulate into a blood clot. This will cause severe pain and irritation. If there is a sudden sharp increase of pain in the rectum and hemorrhoids are present, notify the doctor.
- Symptoms don’t resolve themselves - Hemorrhoids usually resolve themselves in about a week. If they don’t, that’s a red flag to caregiver warning that something more significant might be wrong. Notify the doctor and follow their instructions.
Other Caregiver Factors
There are some important anatomic facts that caregivers should know about. Where the hemorrhoids occur should matter to caregivers. External anal tissues have a lot more nerve endings than internal tissues. Pain and discomfort problems are more likely to occur. Internal hemorrhoids may be less painful but prolapsing outside the anal sphincter has its own problems to contend with. If internal hemorrhoids are associated with pain, then the seriousness factor has jumped significantly.
Dealing with the Diagnosis Process
There is a justifiable amount of embarrassment and fear when hemorrhoid symptoms first appear in patients both on the resident and caregiver’s part. No one want’s to talk about or inspect a bottom. Embarrassment leads to inaction, which leads to prolonged suffering on the part of your residents. Uncomfortable residents are bad for business and make caregiving harder. Experienced caregivers can help reduce embarrassment and fear by educating residents about what might be going on and what might happen when they go to the doctor’s office. If you suspect the resident has hemorrhoids, I suggest the following:
- Tell the resident that you suspect they have a non-serious case and you’re sending them to the doctor just to make sure and to get something for their comfort.
- Let the resident know that external hemorrhoids are diagnosed from a basic exam, which will probably include a visual exam. (Caregivers should dress the resident in easily removal garments.)
- If the doctor puts a scope up the resident’s bottom, it’s not a cause for alarm. Internal hemorrhoids are often too soft to be felt by a gloved hand so a visual inspection may be needed. It may require special equipment or procedures involving the rectum. It’s called an anoscopy, which involves interesting a small tube inside the anus (anoscope). The anoscope is lubricated and gently inserted a few inches into the rectum. This procedure enlarges the rectum to allow the doctor to view the entire anal canal with a light. If any suspicious areas are noticed, a piece of tissue can be biopsied.
- During the anoscopy procedure, there may be a feeling of pressure or the need to go to the bathroom. If a biopsy is taken, the patient may feel a slight pinch. The procedure is performed on an out-patient basis and takes approximately an hour to complete. Overall, the doctor’s visit should be very simple and easy to get through.
- Before the exam, the caregiver should record all symptoms that they have noticed and place in a file to be taken with the resident. This record should include:
- Color of the blood (bright red, dark red, coffee grounds look)
- Days of discomfort
- Description of pain symptoms (dull chronic ache, sharp intense pain)
- Bowel movement issues (constipation, diarrhea)
Caregivers could also include in the patient’s file any questions that they want the doctor to answer. The Mayo Clinic website suggests the following questions:
- What's the likely cause of the symptoms?
- Is the condition likely to be temporary or permanent?
- Is my resident at risk of complications related to this condition?
- What treatment approach will you order?
- If treatments we try first don't work, what will you recommend next?
- Is the resident a candidate for surgery? Why or why not?
- Are there any additional self-care steps that might help?
- If there are other medical problems present, how can I manage these along with hemorrhoids?
Source http://www.mayoclinic.org/diseases-conditions/hemorrhoids/basics/preparing-for-your-appointment/con-20029852 questions modified to fit article

Treatments
Most hemorrhoid occurrences are not serious health concerns and will resolves themselves in a week or so. Treatments ordered by the doctor will most likely be of a preventative nature or symptom relief. If in the rare case more aggressive treatment is required, there are simple surgical procedures that can be utilized, many done on an outpatient basis. If these procedures are done, recuperative therapies will need to be performed. So that you can more fully follow any doctor’s orders, let’s go over all the possible treatments that could be ordered.
Prevention
The best treatment is to not get hemorrhoids in the first place. But if they do occur, there will always be the chance that they will pop out again in the future so prevention should be taken seriously. Fortunately most prevention therapy is what you are doing already as part of your regular caregiving duties.
- Avoid added pressure in the rectum area.
- Keep stools regular through a high fiber diet and plenty of liquids. Cooking from scratch is an easy way to add fiber into a diet. The doctor may order bulk laxatives, which are nothing but fiber or stool softeners.
- Watch the over use of laxatives so diarrhea does not compound the problem. If this is an issue, for example with anorexia or bulimia in mental health homes, educate the residents about how the added strain and wiping could cause or aggravate hemorrhoids symptoms.
- Avoid long periods on the toilet. Be aware how long your resident stays in the bathroom. Bad habits may have been formed before they came to live with you that will need to be modified with your help.
- For those with mobility issues who need to sit for long periods of time or are wheelchair bound, shifting the center of gravity of the bottom will need to be done on a regular basis. This is easily accomplished with the use of foam wedges or towels rolled up like jelly rolls. Place them under one side then after a while switch them to the other side. This will comfortably rotate the pressure concentrated on the rectum. The jelly roll trick also promotes blood flow to the area and helps avoid bedsores.
- Exercise helps tone flabby tissues. I’ve said it over and over: daily walks by your residents work wonders in so many ways. I’m a big fan of walking.
Symptom Relief
You can count on the doctor first giving orders that have more do to with getting rid of patient discomfort than eliminating the hemorrhoids. As I stated earlier, the hemorrhoids will most likely disappear by themselves in a week or so. If they don’t, then it’s time to contact the doctor again. The doctor has many choices of medication to choose from. A lot of them are over-the-counter products that can be self- administered. Letting the resident apply medication to their own bottoms is a lot less embarrassing, but you still have to get doctor’s orders to cover your own bottom. You also have to make a judgement call of whether the resident has the mental capacity to apply the medication appropriately, as in the case of the developmentally disabled. If this is the case, it would be wise to get a nurse delegation, again to cover your own tush.
 Medications
Medications
There are 123 medications approved for hemorrhoids. Most are combination products. Each doctor will have their own favorite variety but usually are open to requests. They are sold in various forms, including creams, ointments, suppositories, and chemical wipes. I’ll explain all of them as group by major ingredient, what they do, and what to watch for as a caregiver. It will be up to you to read the ingredient list of the product that you use to determine what actions will be required by you.
Local anesthetics - benzocaine, benzyl alcohol, dibucaine, lidocaine, and pramoxine. These are all short-acting numbing agents. Since they wear off fairly quickly, frequent re-application might be needed. Some patients are allergic to the “caines” (drugs names ending with caine). If a red rash appears or increased irritation is felt, then avoid all the caines in the future. Notify the doctor and dentist of the allergy because the caines are used a lot by them. Wash hands after use because often people forget then rub their eyes or nose and have to deal the numbness that follows. This might sound kind of stupid, caregivers wear gloves to apply medicines after all, but residents do not. Residents applying it themselves will have to be reminded every time or even be supervised in their hand washing. If there are any open sores, the med will sting before the numbness kicks in. A very rare but life-threatening occurrence happens when too much lidocaine is absorbed through the skin and gets into the blood stream. Basically the heart muscle is numbed and the person can die. To avoid this, do not attempt to apply large amounts in an attempt to reduce the number of re-applications needed. Internal hemorrhoids don’t have very many nerve endings to numb so these drugs will mostly not be prescribed. If there is pain associated with internal hemorrhoids, that’s a red flag and should be brought to the attention of the doctor.
Vasoconstrictors - ephedrine, epinephrine, and phenylephrine. These medications shrink blood vessels. They also make them less leaky. It is easy to understand why the medication could be useful in reducing a swollen hemorrhoid. Unfortunately, the drug that is absorbed into the blood stream can constrict blood vessels throughout the body. Those residents with uncontrolled diabetes or hypertension, cardiovascular disease, hyperthyroidism, enlarged prostate, and glaucoma should avoid the use of preparations that contain vasoconstrictors. Residents taking monoamine oxidase inhibitors, tricyclic antidepressants, or high blood pressure drugs should avoid the use of topical vasoconstrictors because they can cause adverse drug events. If the doctor orders you to use them anyway, monitor the resident more closely for signs of trouble. In most cases, short-term use will cause no real problems.
Protectants - zinc oxide, shark liver oil, cocoa butter, topical starch, and lanolin. Think of these agents as barriers, just like diaper rash creams. They prevent nasty things from coming in contact with the protected area. They also keep the area from drying out and provide lubrication against abrasions and pain. They are well tolerated and don’t cause many caregiver concern in their use. Petroleum jelly could be used for this purpose as well. It could be applied after every bowel movement.
Analgesics/anesthetics/antipruritic - menthol, juniper tar and camphor. These are called counterirritants. They work by giving the body something else to focus on beside the pain from the hemorrhoid. I wouldn’t recommend using them by themselves and in my opinion have limited use in hemorrhoid treatments.
Astringents- calamine, zinc oxide, and witch hazel. These chemicals tend to shrink or constrict body tissues by coagulating the proteins on the cell’s surface. This provides temporary protection of irritated rectal areas and relieves the irritation and burning that hemorrhoids can cause. Calamine and zinc oxide have astringent activity (in addition to being protectants) and may be applied internally or externally. Witch hazel is applied only externally. Witch hazel pads are very convenient to use after every bowel movement. First wipe, and then use the medicated pads.
Corticosteroids - hydrocortisone 1%. Hydrocortisone is a weak member of the steroid anti-inflammatory class of drugs. It mimics the body’s own system for reducing inflammation. It can also help reduce itching (pruritus). It may be a mild form, but it is still a steroid and precautions must be taken when used. Keep hydrocortisone out of the eyes and other sensitive areas by proper hand washing after application. Do not apply it for more than two weeks without doctor approval. Prolonged use can thin the skin. If the skin is compromised already as in the case of the infirmed and the elderly, nasty skin tears may occur.
Caregiving Considerations 
Treating the hemorrhoid condition depends on the severity of the symptoms not the extent of the hemorrhoids. If they are not painful or bleeding, then don’t worry too much about them. If they prolapse, put on a glove and push them back in. If there is discomfort, get the resident to the doctor or get the home health nurse out so that you can get doctor’s orders for therapy. There are a few other things you can do beyond preventative efforts and medication. Some of these suggestions might be considered therapy, so if you’re worried about it, get prn doctor’s orders.
- Soak the bottom in a warm bath, 10 to 15 minutes - two to three times daily. Soaking in the tub probably is impractical in a care home setting but you can use a sitz bath to accomplish the same thing. A sitz bath is a specially designed basin that can fit on top of the toilet. They are much easier than giving the resident a bath. They can be purchased at your pharmacy, medical supply store, or online.
- Use wet wipes for bowel movements instead of dry toilet paper. Non-alcoholic or perfumed-based wipes will feel much better on irritated bottoms. You can find them in the diaper section of most stores.
- Pat bottoms dry instead of wiping dry, or better yet use a hair blow drier after soaks or baths.
- Appling an ice pack or cold compresses can numb pain and reduce inflammation in the hemorrhoids. You can cover the ice pack with a sock or cut off sleeve from an old sweater or stretchy shirt. You can remove the sock after use and wash it and keep the cold compress clean to use again.
- Don’t forget to use prn anti-inflammatory pain killer pills that are already prescribed by the doctor. Tylenol helps with pain but does not take down inflammation.
- Internal infections can be detected often by the foul smell that is given off that is different from the smell of a regular bowel movement.
- Pressure can be taken off of sensitive areas by using an inflatable donut to sit on. They can be purchased at any pharmacy or online. If you use one, do not inflate it fully. They will conform to the bottom a lot better if there is some floppiness in them.
Curative Therapies
Regardless of your good caregiving effort, sometimes hemorrhoids stubbornly won’t go away or cause more serious concerns. It is important for you to know what advanced therapeutic options are available so that you can help your residents deal with this embarrassing condition. Treatments are determined by the doctor based on the severity of symptoms. All but the most severe can be handled by minimally invasive procedures. They often can be done right at the doctor’s office or other outpatient setting and the patient can come home right after the procedure.
Pain Due to a Blood Clot
If there is a blood clot in an external hemorrhoid, the doctor can do a simple incision to remove the clot. The pain often is relieved right away. Proper wound care will be required until the incision heals.
Chronic Conditions
For persistent bleeding or chronically painful occurrences, there are a number of simple procedures the doctor can choose from.
- Rubber band ligation. The gold standard is rubber band ligation. The doctor will place one or two tiny rubber bands around the internal hemorrhoid. The rubber band constricts the blood flow and the hemorrhoid withers and falls off. It can take up to a week to fall off. It may cause additional bleeding and discomfort for the patient, developing two to four days after the procedure. An inflatable donut could be helpful. Be sure to get prn pain and bleeding instructions from the doctor in advance. This is also a good time for the home health nurse to get involved so you don’t have to deal with it as much.
- Injection (sclerotherapy). The doctor can also choose to inject a chemical into the tissue that causes the hemorrhoid to shrink. It is less painful but not as effective as rubber banding.
- Coagulation (infrared, laser, or bipolar). A laser, infrared light or heat can be used to harden and shrivel the hemorrhoid. These procedures have few side effects but are associated with more hemorrhoids returning than rubber banding.
Large Hemorrhoids
Surgery may be required for larger hemorrhoids or failures in other therapies. This is considered simple surgery and is performed in an outpatient setting or an overnight hospital stay.
- Hemorrhoid removal (hemorrhoidectomy). A surgeon can surgically remove the excess tissue that is causing the problems. The surgery is performed with a local anesthetic (numbing agent applied directly to the area) coupled with a spinal or general anesthetic while the patient is put to sleep. As a caregiver, you need to know that this is the most effective type of surgery but there is always a chance for complications. They could include temporary difficulty in emptying the bladder, urinary tract infections, and post-surgery pain. Be sure to get prn pain medication, and soaking in a warm bath can help.
- Hemorrhoid stapling. A less pain-inducing surgery is called stapling. It involves stapling tissues to block the blood flow to the hemorrhoid. Generally it allows a return to normal activities sooner that a hemorrhoidectomy. There is a greater risk though for hemorrhoid reoccurrence and rectal prolapse through the anus. In either surgery, getting the home health nurse involved as part of the follow up is a good idea.
Conclusion
There you have it - the subject of hemorrhoids from to top to bottom, and I really do mean the bottom this time. The bottom line for the resident is though the pain and bleeding can be troubling, if it’s caused by hemorrhoids it really is no big deal. The bottom line for caregivers is get the resident checked out by the doctor and helps your resident deal with an embarrassing subject and symptom-relieving therapies. If more advanced therapies are required, they are also simple in nature. Now I have said bottom way too much in one paragraph so I will simply finish by writing the end. (I bet writing the end made you think of something else.)
As always, good luck in your caregiving efforts.
Mark Parkinson RPh.
References:
- Hemorrhoids. The Mayo Clinic. Sept. 29, 2016. http://www.mayoclinic.org/diseases-conditions/hemorrhoids/home/ovc-20249172
- Johnathan Dufton MD. Hemorrhoids: You may not want to sit down. FreeCE.com Pharmaceutical Education Consultants. Universal Activity No.: 0798-0000-14-113-H01-P&T. December 26, 2014 http://www.freece.com/Files/Classroom/ProgramSlides/95bacf6d-a9b3-4c56-b082-40090372b7f5/Hemorrhoids%20Handout%20No%20Pictures%20EA.pdf
- Hemorrhoid. Wikipedia the Free Encyclopedia. April 2 2017. https://en.wikipedia.org/wiki/Hemorrhoid
- What Are Hemorrhoids?. WebMD.com. September 06, 2016. http://www.webmd.com/digestive-disorders/understanding-hemorrhoids-basics#2
- Yvette Terrie RPh. Hemorrhoid Preparations. Pharmacy Times. August 01, 2007. https://www.youtube.com/watch?v=CHV6BjuQOZQ&index=6&list=PL7j5iXGSdMwc7n8Tsjl-I8zEOEZsjWydx
- Hemorrhoids and what to do about them. Harvard Health Publication. Harvard Medical School. October, 2013. http://www.health.harvard.edu/diseases-and-conditions/hemorrhoids_and_what_to_do_about_them
- Christian Nordqvist. Hemorrhoids: Causes, treatments, and prevention. MedicalNews Today. Wed 22 March 2017. http://www.medicalnewstoday.com/articles/73938.php
- Hemorrhoids. The Free Dictionary by Farlex. http://medical-dictionary.thefreedictionary.com/hemorrhoids
- Howard K. Berg MD. Management of Hemorrhoids. University of Maryland, St. Joseph Medical Center. http://mdcolonsurgeons.com/management_of_hemorrhoids.htm
- Anoscopy. The Free Dictionary by Farlex.http://medical-dictionary.thefreedictionary.com/anoscopy
- W. Steven Pray, PhD, DPh. Gabriel E. Pray, PharmD. Counseling Patients With Hemorrhoids. US Pharm. 2011;36(12):12-15. https://www.uspharmacist.com/article/counseling-patients-with-hemorrhoids.
Exam Portal
click on [Take Exam]
Purchase membership here to unlock Exam Portal.
|
|
|
|
|
*Important*
Registration and login is required to place your name on your CE Certificates and access your certificate history.
Username MUST be how you want your name on your CE Certificate.
| Guest: Purchase Exam |


