Pink Puffers and Blue Bloaters – COPD
Pink Puffers and Blue Bloaters – COPD
Author: Mark Parkinson RPh: President AFC-CE
Credit Hours 3- Approximate time required: 180 min.
Educational Goal:
To educate Adult Foster Care providers about Chronic Obstructive Pulmonary Disease.
Educational Objectives:
Explain what COPD is
Explain how Emphysema and Chronic Bronchitis relate to COPD
Describe to new conditions that COPD suffers have to live with
Tell about how to care for COPD patients
List and explain COPD Therapies and Medicines
Provide additional sources of information and resources for residents and caregivers
Procedure:
Read the course materials. 2. Click on exam portal [Take Exam]. 3. If you have not done so yet fill in Register form (username must be the name you want on your CE certificate). 4. Log in 5. Take exam. 6. Click on [Show Results] when done and follow the instructions that appear. 7. A score of 70% or better is considered passing and a Certificate of Completion will be generated for your records.
Disclaimer
The information presented in this activity is not meant to serve as a guideline for patient management. All procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this article should not be used by care providers without evaluation of their patients’ Doctor. Some conditions and possible contraindications may be of concern. All applicable manufacturers’ product information should be reviewed before use. The author and publisher of this continuing education program have made all reasonable efforts to ensure that all information contained herein is accurate in accordance with the latest available scientific knowledge at the time of acceptance for publication. Nutritional products discussed are not intended for the diagnosis, treatment, cure, or prevention of any disease.
Pink Puffers and Blue Bloaters − COPD
Pink puffers and blue bloaters; they sound like characters from a children’s cartoon, but they are something far more serious. They are actually physical descriptions of patients who suffer from emphysema and chronic bronchitis. In emphysema, the patient has lost some of their ability to breathe out regularly. They have to exert themselves harder to puff out each breath, turning pink in the process. Those who suffer from chronic bronchitis find it difficult to get oxygen in and CO2 out of their blood from clogged lungs. It can cause their skin to have a bluish tint. The lower blood oxygen level impairs the circulatory system, and fluids build up, bloating the extremities. What is really intriguing and confusing is, they are both different manifestations of the same condition—Chronic Obstructive Pulmonary Disease or COPD.
 |
What is COPD?
Chronic Obstructive Pulmonary Disease is a broad descriptive term. It refers to a collection of long-term conditions that permanently damage the pulmonary system. The condition leads to an impaired air flow into and out of the lungs. If the COPD conditions continue, lung function gets progressively worse over time. Compromised air flow is a serious condition that can interfere with every aspect of normal living, lead to complications in other disease states, and even cause death. COPD is the third leading cause of death in the United States and burdens the health care system with tens of billions of dollars’ worth of costs a year. There is no cure for the disease, but if you understand what is going on in the lungs, the disease can be managed, and activities of normal life can continue.
Normal Lung Conditions
 The pulmonary system of the body is a series of organs designed to bring air in contact with the circulatory system. That contact allows oxygen to be taken in, and CO2 and other waste gases can be expelled. The process is called gas exchange. Getting enough gas exchanged to meet the needs of the body requires a very large thin surface area between the lungs and the blood system and a large surface area. To achieve the required surface area, the lungs branch several times, ending in many tiny air sacs. Each air sac is surrounded by a system of thin-walled blood capillaries.
The pulmonary system of the body is a series of organs designed to bring air in contact with the circulatory system. That contact allows oxygen to be taken in, and CO2 and other waste gases can be expelled. The process is called gas exchange. Getting enough gas exchanged to meet the needs of the body requires a very large thin surface area between the lungs and the blood system and a large surface area. To achieve the required surface area, the lungs branch several times, ending in many tiny air sacs. Each air sac is surrounded by a system of thin-walled blood capillaries.
Airflow through the lungs is created by intercostal muscles of the rib cage and the diaphragm muscle below. When the muscles contract, the lungs expand, creating a vacuum that pulls in air. As the muscles relax, the lungs, which are made up of a spongey elastic material, spring back into place, forcing the air out.
When you breathe in, air travels down your windpipe or trachea and branches into your lungs via two large tubes called bronchi. Inside your lungs, these tubes divide many times, like the branches of a root. The smaller tubes are called bronchioles. At that end of the bronchioles are clusters of tiny air sacs known as alveoli.
The pulmonary system has a defense system that protects the delicate structures of the lungs. It cleans the air of pollutants and irritants and removes them from the lungs. It includes:
- Specialized cells that produce a protective mucus layer that traps particles in the air.
- Surface cells that have tiny hair-like structures called cilia. The cilia constantly move, sweeping the mucus and its trapped particles out of the lungs.
- Nerve cells that sense foreign material in the air or excess mucus − They trigger the muscles to suddenly contract, creating a sneeze or a cough that expels the unwanted material.
- Immune cells that sense damage − They trigger the protective inflammatory process.
COPD Lung Conditions
The lungs operate efficiently and automatically as long as the tissues remain healthy. If the lungs get damaged, they can repair themselves. Unfortunately, if the lungs continue to be damaged, the repair mechanisms can get overwhelmed and wear out. Over time, the damage becomes permanent, and lung function is compromised. Breathing becomes difficult. Wheezing or crackly breaths can be heard. Breathlessness and/or chest tightness is felt. It becomes harder and harder to get enough oxygen to maintain normal activity levels. Coughing happens more frequently. The body feels tired and lacks energy, and low-grade fevers are often felt.
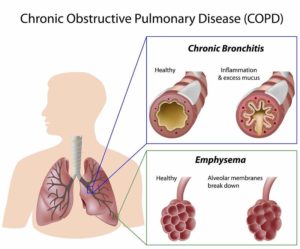
Emphysema
Emphysema is a form of COPD where the lung tissues lose some of their elasticity. Over time, the walls of the alveoli (tiny air sac) weaken and rupture. This creates larger and larger air spaces, reducing the surface area needed for gas exchange. Also, the walls of the bronchioles weaken and are easily collapsed, trapping old air. The trapped air is of poor quality and prevents fresh air from reaching the alveoli. This further reduces the needed gas exchange, and the patient becomes weaker and weaker. The collapsed bronchioles also make it harder and harder to exhale. Those who suffer from emphysema find it easier to breathe by pursing their lips together and puffing out their breaths. This move creates more pressure in the bronchioles, keeping them open. Puffing requires more effort than normal breathing, and the strain tends to turn the skin pink. Over time, the extra exertion takes its toll, and the patient starts to lose weight. In addition, the combination of emphysema symptoms eventually causes the chest to become more barrel-shaped.
Chronic Bronchitis
Chronic Bronchitis is a form COPD where a combination of swelling and extra mucus production closes off airway passages in the lungs. In an effort to protect itself from constant exposure to irritants, the lungs produce more and more mucus. Unfortunately, at the same time, the cilia hairs that move the mucus out of the lungs become damaged by the irritants, leading to mucus build-up. The body has to rely on coughing to remove the excess mucus. The clinical hallmark of chronic bronchitis is a productive (mucus-producing) cough that lasts for at least 3 months out of the year for 2 years. Coughing is not a very efficient way to get rid of mucus. Consequently, the patient often presents with the wet sounding breaths of wheezing and crackles. As more and more bronchioles are closed off, the tissues of the body start to lose their needed oxygen supply. The skin tends to take on a bluish tint in a condition called cyanosis. The extra moist warm conditions of the lungs become a breeding ground for bacteria. Chronic bronchitis makes it easier to get lung infections and fevers.
COPD is both
In almost all incidents of Chronic Obstructive Pulmonary Disease, the patient presents with both emphysema and chronic bronchitis. It is now the common practice of doctors to refer to most cases as just COPD, except in the most severe occurrences of differentiating symptoms.
COPD is a slow, progressive disease that gradually gets worse over time. Most patients who have COPD start having symptoms in their 50s and 60s. There are times, though, when there is a sudden increase in symptoms—referred to as exacerbations. The more often exacerbations occur, the faster the disease progresses. Controlling exacerbations becomes a major focus of therapy.
What causes COPD?
COPD occurs when the lungs are constantly exposed to irritating and noxious substances over a period of decades. In most instances, that means tobacco smoke. In the U.S., 80−95% of those with COPD are current smokers or have previously smoked long-term. Additionally, second-hand smoke exposure has caused COPD in up to 20% of reported cases. Other contributing factors are the genetics of the patient and long-term exposure to workplace chemicals and dust. Women are more susceptible to the harmful effects of tobacco smoke than men.
There is a rare genetic condition called Alpha-1 Antitrypsin Deficiency. The patient is born with a defect in the protective mechanism of the lungs. Without the protein Alpha-1 Antitrypsin, white blood cells begin to break down healthy lung tissues, and COPD can develop, even without exposure to harmful chemicals.
What causes Exacerbations?
The sudden worsening of symptoms or exacerbations is usually triggered by exposure to irritation or inflammation-causing events. Infections are a major risk factor, appearing in 50 to 75% of cases. Other causative factors are poor indoor and outdoor air quality, second-hand smoke, cold weather conditions, and an increase in physical or emotional stresses.
COPD Caused Complications
COPD conditions in the lungs and circulatory systems cause extra stresses in the body of the patient. These stresses can create or contribute to the worsening of other illnesses and harmful circumstances.
- Pulmonary Hypertension − To compensate for localized low oxygen levels, the lungs can shunt blood flow to other areas of the lungs. If low oxygen levels occur everywhere, then hypertension occurs throughout the lungs and causes damage over time.
- Cor Pulmonale − Pulmonary hypertension causes the right side of the heart to work harder and become abnormally large. This leads to right-sided heart failure.
- Heart Problems − For reasons not fully understood, other heart problems can occur with COPD.
- Lung Cancer − The more lung tissue is forced to repair itself, the greater the chance of cell reproduction errors occurring, which can lead to lung cancer.
- Sedentary lifestyle − The lack of oxygen leads to muscle weakness, which encourages a sedentary lifestyle. Without enough activity, other conditions get worse; for example, obesity, osteoporosis, diabetes, constipation, and mental illness.
- Depression − Chronic worry and anxiety caused by breathing problems can overtask the coping mechanism of the patient, leading to clinical depression.
New Realities of COPD
Worldwide, the incidents of COPD are increasing. In the U.S., it is estimated that 30 million people are affected by COPD symptoms. It is believed that over half of the cases do not realize that their lungs have become permanently damaged. In some cases, 50 to 70% of lung capacity is lost before symptoms become problematic. It is a common problem that COPD sufferers believe symptoms they are experiencing are just a part of getting old.
COPD is an insidious and slow-progressing disease. The early signs of increased breathlessness and frequent coughing are easily ignored. As more and more permanent damage occurs, more severe symptoms start to emerge. Wheezing and crackling breaths appear, and lung infections start to occur more frequently. Normal activities of daily living start to become more difficult to maintain.
If any of these symptomatic conditions start to manifest, it is recommended that the patient sees a doctor for a spirometry test. In a spirometry test, a breathing device is used to measure how much air is inhaled (Total Lung Capacity-TLC), how much air is exhaled (Forced Vital Capacity- FVC), and how quickly exhalation occurs (Forced Expiratory Volume in second- FEV1). The doctor can compare these measurements to a norm and determine how much lung damage has occurred.
There is no cure for COPD-damaged lungs. Once the doctor has established that a condition of COPD exists, the patient has to come to terms with a new reality dictated by how much lung function remains. The goals of COPD therapy is to stop or curb exposure to lung irritants (smoking cessation), prevent exacerbations, control symptoms to increase lung function, and learn new ways to maintain activities of normal living.

Caring for those with COPD
The possibility of caring for residents with Chronic Obstructive Pulmonary Disease in care homes stretches across the entire spectrum of the disease. Starting from the rare occurrence of a genetic defect or second-hand smoke, which caused cases in the developed mentally disabled, to the insidious stage where symptoms are just beginning to show in mental health homes where cigarette smoking is such a factor, to dealing with living with the aftermath of permanently damaged lungs in adult foster care homes. Caregivers must learn to recognize those at risk, help eliminate causative agents (stop smoking), watch for developing symptoms, and assist the resident in managing the disease once it is diagnosed. Because care home providers live with the resident 24 hours a day, 7 days a week, they can have a greater impact on COPD cases than any other medical profession.
Recognizing Symptoms and Seeking Treatment
It is impractical and cost-prohibitive to screen the general public for COPD. That is not the case in care homes, though. Care providers can review each client for risk factors and diligently watch for developing symptoms. If a caregiver has their suspicions of a developing COPD case, they can take their client to the doctor for a spirometry test.
The first caregiving step − screen each resident for the following risk factors:
- Family history of COPD or other breathing problems.
- Long-term exposure to second-hand smoke.
- Long-term job exposure to air pollutants or noxious industrial dust (coal mining, tire factory worker, painter).
- Past or current smoker.
- Asthma or other breathing problems.
The second caregiving step − watch for the signs and symptoms of COPD for those at risk:
- Easily out of breath from normal exercise
- Chronic cough
- Regular sputum production (lung mucus)
- Cold weather breathing problems
- Anyone who is smoking or has smoked over the age of 35, especially females
- Frequent flu and colds
- Wheezing or crackling breaths
- Unusually sensitive to changes in air quality
It is essential for caregivers to remember the insidious (hidden) nature of COPD. For those residents with the greatest risk factors, a major portion of the resident’s lungs can be permanently damaged before the more obvious signs of the disease can be seen. The sooner a diagnosis can be given, the more lung function can be saved. The sooner the therapy starts, the easier it will be to maintain a normal lifestyle.
The third caregiving step − communicating your observations to the doctor:
Before sending their clients to the doctors, it is important for caregivers to document their observations and write down their concerns. Include the client’s medication in a printout and place it in the folder. Make sure the folder will accompany the patient to the doctor’s office. It is my experience that a printout in a folder is the best way to communicate with the doctor. They tend to pay attention to written documents more than verbal interactions. If family members are the ones transporting the resident to the doctor, your observations will not get lost in translation. If the caregiver is the one transporting the resident to the doctor, the file folder makes you look more professional. You get more respect and cooperation from the doctor, not only now but in the future as well. Be brief but thorough in your notes and try to include measurable facts.
For example—(you have my permission to copy this format in your own form):
Webster’s Golden Heritage Home
1234 Anywhere St, Anyplace Or -phone 503-555-7418
- Licensed Adult Foster Care Home -
Resident − Jane Smith
Age − 72
Medications − med 1 2 and 3 PRN med
Caregiver’s notes −
Doctor Jones, I am concerned about the possibility of COPD in Jane Smith. I have observed the following: Family history of breathing problems and father was a smoker. She also smoked for at least 20 years before quitting. She is cold intolerant, had a productive cough the last 3 months and tends to have crackling breaths in the morning. She has also had 3 colds in the last year. Do you think it would be wise for Jane Smith to have a spirometry test? Would you please include any follow-up caregiving instructions you have for Jane Smith in this folder and send it back with the patient?
Thank You.
Follow up instructions −
Caregiving Goals of Therapy
After a diagnosis of COPD has been made, the goals of therapy are to reduce problematic symptoms, maintain remaining lung function, and prevent exacerbations from occurring. To accomplish these goals, you as a caregiver have to help the residents understand and follow all medical orders. In addition, you have to find and take full advantage of all available therapies and resources. The emphasis of your COPD caregiving efforts falls into three categories: managing the patient, managing the therapy, and managing the environment.
Managing the Patient
The loss of lung function and the subsequent reduction of the oxygen supply to the blood forces the COPD patient to make changes in the way they live their life. The impact of those changes can be kept to a minimum if they take advantage of all the resources at their disposal. You, the caregiver, are in the best position to support these efforts to ensure the best possible outcomes are achieved.
Educate
It is my firm belief that the more knowledge a patient has about their condition, the better choices they will make on their own. Their efforts will be more consistent because they ‘know’ they are working for their own good. Take the time to inform the resident of what is going on in their lungs. Give instructions on how the lungs work, what has changed that has resulted in their COPD, and what that means for their future. Reassure them that you will help them learn ways to breathe better, slow the progression of the COPD, keep them from getting sick, and find ways to live a normal life. Here are some further resources that might help you educate the patient:
 |
 |
 |
 |
 |
- COPD Foundation- https://www.copdfoundation.org/What-is-COPD/Understanding-COPD/What-is-COPD.aspx
- YouTube Emphysema- https://www.youtube.com/watch?v=TEuSV_7gWA8
- YouTube Chronic Bronchitis-https://www.youtube.com/watch?v=Y29bTzKK_P8
- COPD Mayo Clinic- https://www.mayoclinic.org/diseases-conditions/copd/symptoms-causes/syc-20353679
- COPD- WebMD https://www.webmd.com/lung/copd/tc/chronic-obstructive-pulmonary-disease-copd-overview#1
Identify self-care deficits
Living with COPD creates many new challenges for your resident to overcome. Some will be easy to cope with, while other aspects might be too difficult to handle alone. Some residents may even have developed coping habits that are actually counterproductive. You, the caregiver, should know in advance what to monitor for and know ways to help. When you identify the difficulties they are having, you can get the additional equipment, training, or therapy they need.
Lifestyle Support
Helping residents live a normal life when extra care is needed is what foster caregivers do better than any other health profession. Who else actually lives with the patient? You will see what is needed before anyone else and notice areas of need that others might miss. But this will only happen if you are actively looking. You are also in the best position to help the patient make healthy lifestyle choices and continue with needed therapy, even when it becomes difficult. You should also be prepared to battle with the powers that be to get what your residents need and to help the residents do what is necessary to live a normal life. In the end, it will make your job easier and help you retain customers longer in your home. The following are areas where you can supply support for those with COPD:
Physical support − There are a number of things that caregivers can do to increase the patient’s activity tolerance:
- Canes and other stability aids can be used to reduce the amount exertion it takes to accomplish normal activities of daily living. They may not be needed for stability, but they will help reduce the physical strain that contributes to breathlessness. Insurance may cover some of the costs of obtaining such devices, but it will require a prescription by the doctor.
- Pacing or altering schedules can also help not to overtask residents. Caregivers should extend schedules and break up activities into smaller actions, with rest in between. You should allow the COPD resident to have more time to do regular activities.
- Always being there to assist. For example, helping a resident to stand or transfer and lifting objects.
Exercise support − There is a natural tendency to avoid exercise when you’re breathless. This leads to muscle wasting and weakness, contributing further to activity intolerance. In a twist of irony, it’s actually better for the patient to exercise. Fit muscles use oxygen more efficiently, and the added strength increases activity levels. In care homes, general exercise conditioning is easiest to accomplish in taking walks (my personal preference because it’s therapeutic on many different levels), using stationary bikes or simple steppers. Used exercise equipment can be purchased cheaply at thrift stores like the Salvation Army or Desert Industries. Caregivers should make exercise a part of the regular daily routine.
Nutritional Support − COPD symptoms tend to create nutritional imbalances. COPD creates a loss of appetite in many people. Additionally, in the more advanced stages of COPD, caloric requirements may not be met in a regular diet. Caregivers should start measuring the patient’s weight. If it starts to drop, then diets will have to change accordingly. It is recommended in such cases that additional high-protein, high-calorie snacks be given throughout the day. High-fat and high-protein are better than high-carbohydrate snacks, likewise bodybuilder supplements or adding a raw egg to nutritional drinks like Ensure or Boost, which are easy to purchase and supply to the resident. Snack resistance may occur due to appetite loss and flavor boredom. A way to combat this tendency is to allow the resident to choose additional ingredients like adding jams or jellies to the drinks or having a deviled egg instead of a raw one. Your creativity combined with the resident’s ability to choose will go a long way in overcoming resistance.
Emotional Support − It’s frightening to be breathless, and it’s frustrating to not be able to function like you used to. It’s easy for COPD residents to slip into depression or lash out in anger when their emotions get the better of them. Caregivers can:
- Help the patient feel more in control through education and reality checks.
- Be an empathetic listening ear so residents can vent their emotions in a more healthy fashion.
- Push for psychiatric therapy when it’s needed.
- Help the resident stay active and be involved despite their reduced abilities.
Quit smoking − The most potent and important COPD therapy is to stop smoking. Unfortunately, tobacco addictions are among the strongest addictions that there is. The residents will need your assistance to be successful in quitting. As a caregiver helping the smoker resident, you need to consider the following:
- Addiction is not a deficiency of willpower. It is a ‘rewiring’ of the brain so that the sufferer will automatically crave tobacco before thought or reason kicks in. It actually takes more willpower to overcome an addiction. The caregiver can be the source of that extra willpower and the timely reason that is needed to ‘undo the rewiring.’
- Smoking is three strong habits in one. In addition to the chemical addiction, smoking also involves social and emotional habits. A smoker wraps their life and all their social interactions around smoking. Smoking’s effect on the nervous system turns it into a chemical crutch that a smoker turns to in times of emotional struggles. Chemical dependency can leave the body in as little as two weeks, but if the other habits are not dealt with, there is a reduced chance of quitting for good.
- Quitting is a process, not an event. There is no such thing as a failure; just a prolongation of quitting efforts. Caregivers can help rekindle efforts by identifying the triggers that caused the smoking to occur. Once the trigger is eliminated or dealt with, start smoking cessation again and again and again. Never give up.
Managing the Therapy
COPD is an incurable disease, but its symptoms can be managed. Therapies that reduce the impact of symptoms and slow the progression of the disease can be applied. If managed properly, COPD therapies can help the patient lead a fairly normal life. Foster care providers are positioned at the focal point between the patient and the medical community at large. They can push for needed therapies and help the resident understand and accomplish each therapy as it’s prescribed. Caregivers also play a major role in monitoring the therapy for effect and help report and manage any side effect problems that may arise. It would be wise for the care provider to learn about each new therapy along with the patient and, whenever possible, be trained in delegating therapeutic tasks.
COPD Therapies:
Oxygen Therapy
Supplying extra oxygen can help reduce most ill effects of COPD. It reduces the strain on the heart and shortness of breath, helps keep the resident active and thinking clearly, and it helps them sleep and feel better. Oxygen therapy requires a prescription that will need to be presented to a durable medical equipment or a medical gas supplier.
Each prescription will include:
- When the oxygen is to be used (for rest, exercise, and/or sleep) and how much in liters per minute (lpm) for each activity.
- How many hours a day oxygen should be used.
- What type of oxygen system you should use.
Ultimately, the doctor will decide on which type of oxygen equipment that will be used. In order to make an appropriate choice, the doctor should be informed about the following factors:
- How often and for how long will the resident leave your home, and what activities will they do while they are out.
- If there are any physical limitations (patient’s strength and dexterity, wheelchairs, stairs, transportation, home layout, etc.).
- If the resident has any personal preferences (mouth or nose breather, ease of use, level of service from local suppliers).
According to UCSF medical center, there are three types of oxygen systems currently available: compressed gas systems, portable oxygen concentrators (POCs), and liquid oxygen systems.
|
Type of System |
Ambulatory Component |
Stationary Component |
|
Compressed gas system |
Small, pre-filled tanks delivered to you on a weekly basis, depending on how much oxygen you are using, or tanks that fill overnight at home (aka a home-fill system) from your concentrator. These small tanks must be used in conjunction with an oxygen conserving device or regulator (OCD) that delivers the oxygen in pulses so that the oxygen supply lasts longer. |
Oxygen concentrator with 50-foot tubing |
|
Liquid oxygen system |
Small, refillable tank that you fill from the reservoir as needed. |
Oxygen reservoir with 50-foot tubing |
|
Portable oxygen concentrator (POC) |
A small electric device that can be worn on the back or wheeled around, runs on regular electricity or a battery, is easily recharged even in a car, and requires no tanks or filling. The maximum tubing length for proper delivery of oxygen is 7 feet. These units can be taken onto airplanes. |
Source: https://www.ucsfhealth.org/education/supplemental_oxygen/your_oxygen_equipment/
The oxygen supplier is the expert on the system they deliver. Keep asking questions of them until you and your resident are comfortable with the equipment. Here are some questions to consider: How do I clean the equipment? What is the maintenance schedule? What do I do in power outages? How can they be reached after business hours? How can I order supplies and accessories (nasal cannula, masks, humidifiers, tubing, carrying cases, etc.)?
Monitoring oxygen therapy is a matter of monitoring the activity level of the patient and appearance of low oxygen symptoms. A pulse ox is a device that measures oxygen saturation levels. It is an important caregiver’s device to monitor blood oxygen levels and a deviation from the norm-needs to be reported to the doctor.
One side effect of oxygen therapy is that it dries out nasal passages. Ask the oxygen supplier what nasal moisturizer works well with their equipment. They may supply a humidifier attachment. If they have no suggestions, I recommend a saline nasa l gel like Ayr, Nasogel, or Rhinase. Petroleum jelly is not recommended for use with oxygen therapy. The petroleum jelly tends to dissolve nasal cannulas, and droplets of jelly are inhaled and collect in the lungs.
l gel like Ayr, Nasogel, or Rhinase. Petroleum jelly is not recommended for use with oxygen therapy. The petroleum jelly tends to dissolve nasal cannulas, and droplets of jelly are inhaled and collect in the lungs.
Medication Therapy
There are several classes of medications that can be used to relieve and/or control COPD symptoms. They are expectorants, bronchodilators, and corticosteroids. Older medications come as a pill or in liquid form and are taken orally. Most newer medications are breathed directly into the lungs from a hand-held inhaler device or in mist form from a nebulizing machine. Inhaled drugs generally require less medication and have fewer side effects than oral COPD prescriptions.
Expectorants − Expectorants thin mucus and stimulate more productive coughing. The most effective expectorant in COPD is water. It may be unusual to think of water as a drug, but in COPD, adequate hydration is a very effective therapy. Unfortunately, it is possible to get too much water, and therapy can stray into harmful fluid overload conditions. Consult with the doctor for daily amounts of therapeutic fluid intake; remember that quantity is the total from all sources.
Bronchodilators − Bronchodilators work on the nerves that relax the smooth muscle layer of the lungs. They are designed to reduce bronchospasms and open up the lung’s passageways. There are short-acting ‘rescue inhalers,’ long-acting inhalers, and brochodilating oral medications.
Long-acting bronchodilators are the mainstay of COPD therapy. They are taken once or twice a day on a regular basis. Short-acting bronchodilators have a quick onset of action (seconds to minutes) but wear off too quickly to be used as regular therapy. They are usually taken on an as-needed basis when extra breathing help is required.
Normalized breathing patterns are what to monitor for when these drugs are used. Side effects are tachycardia, anxiety, headache, insomnia, nervousness, tremors, and restlessness. When a rescue inhaler is used, these side effects may become more pronounced temporarily.
The oral bronchodilators theophylline and aminophylline are older maintenance therapies that are usually only used when costs are an issue or when other alternatives have failed. They have a more prominent side effect profile, which includes dyspepsia, nausea, vomiting, diarrhea, headache, dizziness, and tachycardia. They also can interact with other medications (including caffeine), which will interfere with therapy and cause more side effects.
Corticosteroids − Inhaled corticosteroids are used to reduce the inflammation in the lungs. They have less effect on the course of COPD symptoms, so they are usually used in combination with a bronchodilator or as an add-on therapy. Again, breathing patterns are what to monitor for. The side effects are oral candidiasis (thrush or oral fungal infection), hoarse voice, skin bruising, and pneumonia. Rinsing the mouth after each use reduces the chance of side effects. Oral corticosteroids are usually reserved for exacerbation control.
Monitoring for the long-term effect − COPD is a progressive disease that could get worse over time. The medication regime might need to be changed to compensate. Watch for long-term trends in exacerbations, PRN med use, pulse ox readings, and increases in coughing; then report your observations to the doctor.
Inhaler use
Inhalers are a very efficient method of medication delivery but only if they are used correctly. The doctor and the pharmacist are supposed to give instructions and make sure the patient understands, but that doesn’t always happen. Instructions can be forgotten or misunderstood, and often the pharmacist never even sees the patient. That leaves you, the caregiver, as the final back-up to ensure inhalers are being properly used.
Here are a few ideas that might help:
- Send the inhalers with the patient when they go to the doctor, even on follow-up visits. Send a note in the patient’s file requesting the doctor to review inhaler use with the patient.
- Ensure the patient sees a pharmacist for instructions after a doctor’s visit. That means that you will have to give additional instructions to whoever is taking the resident to stop by the pharmacy before coming home.
- If you have a consulting pharmacist coming to your home to review medical records, have them give inhaler use instructions right then.
- Look up instructional videos on your computer. Here is a good source: https://use-inhalers.com/,or you can simply type in the search field “video [name of drug] user guide.” I strongly recommend that you, the caregiver, watch the videos and compare them with how your resident is using their inhaler.
Therapeutic Breathing Techniques
Being out of breath occurs more frequently and is harder to resolve in COPD. Normal methods of ‘catching your breath’ don’t work like they used to. That naturally leads to increased anxiety. Being stressed leads to faster, more forceful breathing. The extra air pressure leads to collapsed bronchioles, which traps more bad air, contributing to more breathlessness. It’s a downward cycle that needs to be broken by more therapeutic breathing techniques. When breathlessness occurs, the caregiver can be there to coach the resident in the proper way to catch their breath and help reduce anxiety.

Pursed-Lip Breathing − “Breathe in through your nose (as if you are smelling something) for about 2 seconds. Pucker your lips like you’re getting ready to blow out candles on a birthday cake. Breathe out very slowly through pursed-lips, two to three times as long as you breathed in. Repeat” (Source: COPD foundation). The goal of pursed-lip breathing is to slow rapid breathing, prevent small airway collapse, and help get rid of more bad air from the lungs.
Here is a video example: https://www.youtube.com/watch?v=7kpJ0QlRss4
Diaphragmatic Breathing − “This technique is best used when you’re feeling rested and relaxed, and while sitting back or lying down. Relax your shoulders. Place one hand on your chest and the other on your belly. Inhale through your nose for about two seconds. As you breathe in, your belly should move outward. Your belly should move more than your chest. As you breathe out slowly through pursed-lips, gently press on your belly. This will push up on your diaphragm to help get your air out. Repeat” (Source: COPD foundation). The goal is to utilize the diaphragm more efficiently to breathe and slow the respiratory rate.
Here is a video example; https://www.youtube.com/watch?v=wai-GIYGMeo
Better breathing tips:
- Relax − When stressed, it’s normal to tense muscles, throw your shoulders back, and make your spine straight—all of which makes it harder to breathe in COPD. To relax, close your eye and concentrate on relaxing your muscles and slow your respiratory rate.
- Tripod position − Have the resident relax, leaning forward. Allow the shoulders to sag, with the arm extended forward, creating a tripod effect. Place the feet about 1 foot apart. The tripod helps the resident with upper body relaxation and helps the diaphragm work better.
- Activity reset − When activity creates breathlessness, purposely stop and relax. Use therapeutic breathing to catch your breath. Then continue with the activity using pursed-lip
Managing the Environment
COPD sufferers are more sensitive to environmental changes than other residents. Caregivers will have to learn how to recognize those effects that trigger an increase in COPD symptoms and control them. Once learned, the caregiver will have to pass on their knowledge to others—like family members. To help, care home owners could change heating filters more frequently, install HEPA air filters and have their air ducts cleaned.
|
Potential triggers:
|
 |
Exacerbations
Even with proper caregiving, an exacerbation can occur, which could send the patient to the hospital. An acute exacerbation is a sudden increase in COPD symptoms that lasts days to weeks. If left uncontrolled, it could cause permanent damage that would hasten the progress of the disease. It would be wise to get standing orders from doctors that instruct the caregiver on what to do at the onset of symptoms.
The signs of a COPD exacerbation are:
- Wheezing, coughing, or shortness of breath that is worse than usual
- An increase in the amount of mucus or changes in its color to yellow, green, tan, or bloody
- Shallow or rapid breathing, more than what’s normal for you
- Fever
- Confusion or excessive sleepiness
- Swelling in your feet or ankles
The most common causes of exacerbations are upper respiratory infections. The caregiver can reduce this risk by ensuring the resident’s inoculations are up to date. Consult with the doctor or pharmacist on which shots are needed and keep an up-to-date record in the patient’s file.
Advanced Therapies
There will be times when you, or the resident, get frustrated and ask, “Isn’t there anything else that we can do?” At these times, it is important to remember that the lung damage is permanent, but there are a few advanced therapies that you could ask the doctor about:
Pulmonary Rehabilitation − Pulmonary rehabilitation is a disease management program run by a multidisciplinary team of specialists. They educate the patient, provide counseling when needed, develop and supervise exercise and nutritional programs. They are designed to help the patient and their caregivers manage the disease the best way possible.
Surgical options − For very serious cases, or for younger aged individuals, lung transplantation or lung volume reduction surgery may be considered. In lung volume reduction surgeries, the most damaged parts of the lungs are removed, allowing the rest of the lung to expand and work better. Both are considered major surgeries and have their own risks and possible complications.
Conclusion
Chronic Obstructive Pulmonary Disease is a progressive lung disease where the air flow is permanently compromised. It is a serious condition that can interfere with every aspect of normal living. The patient is going to need help learning a new lifestyle and managing the disease to slow its progression. Adult Foster Care providers are in the best possible position to help with the 24/7/365 activities that will be required of the patient. For the best possible result, the caregiver should learn, along with the resident, about all aspects of the disease. Caregivers should monitor all the therapies for effect and side effect and communicate their observations to the doctor. They should also provide social and emotional support for their client and help procure any needed resource or therapy.
As always,
Good Luck with your caregiving efforts!
Mark Parkinson BS Pharm
References:
COPD (Chronic Obstructive Pulmonary Disease). Physiopedia. https://www.physio-pedia.com/COPD_(Chronic_Obstructive_Pulmonary_Disease)
Your Oxygen Equipment. University of California San Francisco Health . https://www.ucsfhealth.org/education/supplemental_oxygen/your_oxygen_equipment/
COPD. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/copd/symptoms-causes/syc-20353679
Chronic Obstructive Pulmonary Disease. Wikipedia. https://en.wikipedia.org/wiki/Chronic_obstructive_pulmonary_disease
Emphysema (chronic obstructive pulmonary disease). Osmosis. https://www.youtube.com/watch?v=TEuSV_7gWA8
What is COPD? COPD Foundation. https://www.copdfoundation.org/What-is-COPD/Understanding-COPD/What-is-COPD.aspx
COPD (Chronic Obstructive Pulmonary Disease) - Topic Overview. WebMD. https://www.webmd.com/lung/copd/tc/chronic-obstructive-pulmonary-disease-copd-overview#1
Charles Patrick Davis, MD, PhD. COPD (Chronic Obstructive Pulmonary Disease) Symptoms, Causes, Stages and Life Expectancy. MedicineNet.com. https://www.medicinenet.com/copd_chronic_obstructive_pulmonary_disease/article.htm
Ana Gotter. Pursed Lip Breathing. Healthline Jul. 3, 2017. https://www.healthline.com/health/pursed-lip-breathing#benefits
Unit 6 Respitory Problems. Pg 680-684. http://www.coursewareobjects.com/objects/evolve/E2/book_pages/monahan/pdfs/NursingManagement.pdf
Marianne Belleza, RN. Chronic Obstructive Pulmonary Disease (COPD). Nurse Labs Sep. 14 2016. https://nurseslabs.com/chronic-obstructive-pulmonary-disease-copd/
Gerene S. Bauldoff, PhD, RN,. When breathing is a burden: How to help patients with COPD. American Nurse Today August 2012 Vol. 7 No. 8.https://www.americannursetoday.com/when-breathing-is-a-burden-how-to-help-patients-with-copd-2/
Lindsay A. Brust-Sisti, PharmD, Changing the Paradigm: Focus on Preventing Exacerbations in COPD. Power-Pak CE. Aug. 23 2017. http://www.powerpak.com/course/content/115436
Exam Portal
click on [Take Exam]
Purchase membership here to unlock Exam Portal.
|
|
|
|
|
*Important*
Registration and login is required to place your name on your CE Certificates and access your certificate history.
Username MUST be how you want your name on your CE Certificate.
| Guest: Purchase Exam |




