The Caregiver’s Roles in Managing Constipation
The Caregiver’s Roles in Managing Constipation
Author: Mark Parkinson RPh: President AFC-CE
Credit Hours 3- Approximate time required: 180 min.
Educational Goal:
To explain how to manage constipation issues in Adult Foster Care homes.
Educational Objectives:
Define the role of caregiver in managing constipation
Debunk myths that have arisen about constipation
Explain how bowels work
Discuss how chronic constipation occurs and pseudo-constipation occurences
List effective therapies and medications and their management
Provide suggestions for effect communication about constipation and its management
Procedure:
Read the course materials. 2. Click on exam portal [Take Exam]. 3. If you have not done so yet fill in Register form (username must be the name you want on your CE certificate). 4. Log in 5. Take exam. 6. Click on [Show Results] when done and follow the instructions that appear. 7. A score of 70% or better is considered passing and a Certificate of Completion will be generated for your records.
Disclaimer
The information presented in this activity is not meant to serve as a guideline for patient management. All procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this article should not be used by care providers without evaluation of their patients’ Doctor. Some conditions and possible contraindications may be of concern. All applicable manufacturers’ product information should be reviewed before use. The author and publisher of this continuing education program have made all reasonable efforts to ensure that all information contained herein is accurate in accordance with the latest available scientific knowledge at the time of acceptance for publication. Nutritional products discussed are not intended for the diagnosis, treatment, cure, or prevention of any disease.
The Caregiver’s Roles in Managing Constipation
Being constipated is one of the most common complaints of residents in foster care homes. It certainly was in the homes that I was in. Some of my residents almost seemed obsessed by the idea. If they didn’t consistently have a bowel movement every day, they would start demanding a laxative. I remember buying prune juice by the case, and my medicine cabinet was crammed full of bulk laxative powders and stool softeners. The normal breakfast routine was: set the table, prepare the food, and then mix the bulk laxative drinks. I was always in a rush to try to get the laxative drinks down the resident before it turned into a thick to mush. Before I became a care provider, I did not think I would be spending so much time thinking about other people’s bowel movements. It’s funny to think of it now—so many years later, I became a bowel movement expert.
Like it or not, the reality in care homes is, caregivers have to deal with constipation. Wikipedia, the online encyclopedia, reports that “Among elderly people living in a care home the rate of constipation is 50–75 percent.” Caregivers have to be concerned about the frequency and consistency of their residents’ bowel movements. They have to dispense laxative medication and monitor it for effect and possible side effects. When there is a laxative on the PRN (take as needed) med list, the caregiver has to determine, is there actually a need for the drug?
Another reality of caregiving is that since virtually everyone has been constipated and taken a laxative at multiple times in their life, they think they are the experts when it comes to their bowel movements. In actuality, a lot of that supposed expertise is based on myth and old wives’ tales—and this has led many to suffer from a condition called pseudo-constipation, the perception of constipation where actually none exists. If the resident does not experience a bowel movement on schedule, they think they are becoming ‘irregular,’ and they reach for a laxative to become ‘regular’ again. In their minds, the lack of consistency in bowel movements equals constipation, and the result—overuse of laxatives. The more often a laxative is used where none is needed, the more likelihood that a dependency on the laxative for normal bowel movements will develop. The caregiver often finds themselves trying to dispel myths and struggling to break bad laxative use habits. If the caregiver does not have a good understanding of bowel movements themselves, their resident behavior modification efforts become so much hard to accomplish.
Mental health homes and other caregivers have to deal with the added complication of laxative abuse. The resident’s overuse of laxatives is tied to larger psychological issues. Some good examples are laxative abuse stemming from the eating disorders anorexia and bulimia.
So, let’s start by giving you the needed basic education you need to fulfill your dual roles of bowel movement expert and resident behavioral modification support specialist.
How Do Bowels Work?
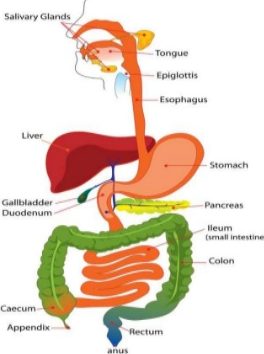 We get the nutrients we need from the food we eat as it passes through the alimentary canal within our body. The alimentary canal or gastrointestinal tract (GI tract) is basically a tube within our bodies made up of several different organs. Each organ is responsible for a different step in the process of extracting what we need from what we eat.
We get the nutrients we need from the food we eat as it passes through the alimentary canal within our body. The alimentary canal or gastrointestinal tract (GI tract) is basically a tube within our bodies made up of several different organs. Each organ is responsible for a different step in the process of extracting what we need from what we eat.
The upper GI tract is comprised of the mouth, throat, and stomach. Their function is to mash up the food and inject liquids and digestive fluids. The digestive fluids contain enzymes and acids that further chemically break down the mashed-up food into a more easily absorbable food slurry.
The lower GI tract is made up of the accessory organs, the small intestine, large intestine, and rectum. The main accessory organs are the liver, gallbladder, and pancreas. They aid in the further breakdown of the flood slurry. The small intestine is a long, folded and coiled tube (about 10 feet in adults). It receives the food slurry and absorbs about 90% of the nutrients we need from it. What is leftover is indigestible and is passed to the large intestine as waste. The large intestine reabsorbs the water from the slurry waste, turning it into a paste. The more time the waste stays in the large intestine, the more water is reabsorbed. The paste becomes more and more solid, making it easier to expel. The solid waste is pushed into the rectum. As the rectum expands, stretch receptor nerves send signals to the brain that it’s time to go to the bathroom.
How Does Constipation Occur?
Food travels through the GI tract and is moved by three main factors: gravity, regular body movements, and peristalsis.  Peristalsis is defined as “successive waves of involuntary contraction passing along the walls of a hollow muscular structure (such as the esophagus or intestine) and forcing the contents onward” (source: Merriam-Webster). While gravity and peristalsis are, for the most part, constant forces, food passage caused by body movement is dependent on how active the body is. Under normal conditions, material passes through the GI tract automatically and without difficulty.
Peristalsis is defined as “successive waves of involuntary contraction passing along the walls of a hollow muscular structure (such as the esophagus or intestine) and forcing the contents onward” (source: Merriam-Webster). While gravity and peristalsis are, for the most part, constant forces, food passage caused by body movement is dependent on how active the body is. Under normal conditions, material passes through the GI tract automatically and without difficulty.
Constipation occurs when something interferes with the three main forces involved in bowel movements. The result is, fecal matter stays in the large intestine for longer periods of time. The more time spent in the large intestine, the more water is reabsorbed. The fecal matter collects and becomes more and more solid, resulting in constipation. The same results happen when the urge to defecate is ignored. Constipation can also be caused by disturbances in the underlining physiology of the GI tract. An easier way to comprehend that is, there is something broken in the machinery that runs the plumbing in the bowels. Some of the parts just don’t work right.
Chronic Constipation
Occasional constipation is quite common. Random events conspired to cause a temporary bout of constipation. The events are usually self-limiting. The body can make the required adjustments that will take care of the problem by itself. The caregiver doesn’t have to worry about such events. Chronic or frequently-occurring constipation is a different matter; it becomes a problem when it does not go away by itself. It can make your resident very miserable and create several complications. Along with the discomfort in the lower GI, the resident could also experience bloating, flatulence, nausea, loss of appetite, headaches, frustration, and irritability.
Other complications caused by chronic constipation are:
- Behavioral Problems − For those residents with limited or reduced mental capabilities, prolonged bouts of constipation can be the cause of sudden increased behavioral problems. One of the tricks of the trade in caring for the mentally handicapped (including dementia, Alzheimer’s disease, and certain mental health conditions) is this: keeping the patient’s bowels regular keeps the resident calmer.
- Fecal impaction − Impaction is when stools become so hard that they are impossible to pass. It forms a plug that backs up the fecal matter. As the peristaltic pressure builds up, extreme nausea and vomiting can occur. Also, ironically, the more liquid parts of the backed up stool can squirt around the plug, causing a bout of diarrhea. Impacted bowels require a pair of gloved hands or even surgery to manually remove the plug. Not a pleasant thought for the resident or the caregiver. Impactions can even affect blood circulation, breathing and cause death.
- Tissue damage caused by straining − Your residents’ bodies can only take so much stretching and straining. Bowels can be permanently distended, hemorrhoids can appear, bowels can prolapse and protrude out of the rectum, tissues can tear and bleed (anal fissures), and weakened hearts can fail. There are many heart attacks each year caused by bathroom straining.
The seriousness of constipation was shown to me in a very real and tragic way. When I was a pharmacist practicing in Coos Bay, we had a bathroom next to the pharmacy that both the staff and the public used. One day, there was a customer that would just not leave the bathroom stall. Eventually, his wife came looking for him. I went into the bathroom to check on him. I didn’t want to cause embarrassment, so I just took a peek under the stall door. I saw an arm, which had turned blue clear up to his elbow, dangling near his feet. He supposedly had a heart attack while straining and died right there on the public toilet. What a way to go, and how sad it was for the worried wife!
Causes of Chronic Constipation
Chronic constipation is not a disease unto itself. It is a symptom of other issues. Frequent or long bouts of constipation are a red flag warning the caregiver that something is going wrong, or a condition is getting worse. A savvy caregiver can use this to their advantage and nip potential problems in the bud. In regards to constipation, these are the things that caregivers should be thinking about:
- Dehydration − It takes a lot of water to keep the body functioning. If the body doesn’t get enough from the fluids we drink, it’s going to take it from the foods we eat in greater quantities than normal. The result—more solid stools and eventually constipation if the dehydration continues. How much water does a resident need daily?
|
Demographic |
Daily recommended amount of water (from drinks) |
|
children 4–8 years old |
5 cups, or 40 total ounces |
|
children 9–13 years old |
7–8 cups, or 56–64 total ounces |
|
children 14–18 years old |
8–11 cups, or 64–88 total ounces |
|
men, 19 years and older |
13 cups, or 104 total ounces |
|
women, 19 years and older |
9 cups, or 72 total ounces |
|
pregnant women |
10 cups, or 80 total ounces |
|
breastfeeding women |
13 cups, or 104 total ounces |
Source: https://www.healthline.com/health/how-much-water-should-I-drink#recommendations2
- Loss of Body Salts − Many bowel functions depend on chemical processes involving body salts. If there is a loss of body salts through the kidneys or through vomiting or diarrhea, constipation may occur. The caregiver should monitor residents for constipation, especially in those who have had a long bout of sickness involving large amounts of fluid loss. Sport drinks that replace electrolytes can be useful in such cases.
- Opioid-Induced Constipation- A side effect of opioid painkillers is that they slow down GI tract peristalsis. The more time the stool stays in the large intestine, the more fluid is pulled out. The lack of motility, as well as the more solid the stools are, makes it harder to pass the stools. Caregivers should be vigilant for constipation if they see an opioid or narcotic on the med list.
Opioid/Narcotic Drugs that Cause Constipation:
- codeine (only available in generic form)
- fentanyl (Actiq, Duragesic, Fentora)

- hydrocodone (Hysingla ER, Zohydro ER)
- hydrocodone/acetaminophen (Lorcet, Lortab, Norco, Vicodin)
- hydromorphone (Dilaudid, Exalgo)
- meperidine (Demerol)
- methadone (Dolophine, Methadose)
- morphine (Astramorph, Avinza, Kadian, MS Contin, Ora-Morph SR)
- oxycodone (OxyContin, Oxecta, Roxicodone)
- oxycodone and acetaminophen (Percocet, Endocet, Roxicet)
- oxycodone and naloxone (Targiniq ER)
- Poor Diet − A low-fiber, high-carb diet changes the composition of the fecal matter. There is less water retained in the stools. Also, less bulk in the stools means less volume. Without the volume, the stretch receptors aren’t triggered, reducing the urge to void. Poor diet causes chronic constipation frequently in the ill and the infirm. Their condition leads to poor eating habits. It would be wise for caregivers to question new move-ins about their bowel conditions. Most likely, you’re going to have to work on getting the new resident regular again right from the start.
- Irritable Bowel Syndrome (IBS) and Crohn's − These are diseases of the digestive tract. They can cause bowel spasms and interfere with normal peristalsis which slows down bowel movements. There is no cure for IBS or Crohn’s disease—just control. Caregivers can help the patient manage by controlling the diet and monitoring bowel movements.
- Hormonal Changes − Our bodies rely on hormones to control various bodily functions. Many are involved in bowel movements. Changes in hormone levels can induce constipation. Keep your eyes open if you see, on the patient’s records, estrogen, progesterone, and thyroid meds, or a history of diabetes and hyperparathyroidism. In these cases, the appearance of constipation can be used as a red flag warning to caregivers that things need to be looked into. When constipation starts to become more frequent, start asking the doctor questions about hormone levels. Make lab tests requests on behalf of the resident to the doctor.
- Paralysis − The loss of control of muscle movement reduces fecal matter motility and reduces the body’s movements that help move the stool through the intestine. There are several disease states that have paralysis symptoms—like Parkinson’s disease, stroke, multiple sclerosis, spinal cord injury, and autonomic neuropathy. Here again, constipation symptoms can be utilized as a way of seeing warning signs that the disease is getting worse, and the patient needs more medical attention from the doctor. Wheelchair-bound residents should be monitored particularly closely.
- Drug Side Effects − Drugs have unintended effects; it can’t be helped. One of them is constipation. If constipation becomes problematic, the drug might have to be reduced, changed, or discontinued. It’s impractical to list all the drugs that could cause problems; there’s too many. If constipation starts to be a problem, it would be wise to take a look at the drug information sheet that comes with your prescriptions. (You know, those papers that you never pay attention to and keep throwing away each month.) If constipation becomes a problem, contact the doctor and start asking, “Is the drug causing the issue?” After that, it becomes a balancing act. Which is the worse problem, constipation or the underlying issue of the offending drug?
Some of the major medication culprits are:
Antidepressants − amitriptyline, imipramine
Anticonvulsants − phenytoin, carbamazepine
Mineral supplements − iron and calcium
Antacids that contain aluminum and calcium
Antipsychotics − clozapine, thioridazine, chlorpromazine
Calcium channel blockers − verapamil, diltiazem, nifedipine
Parkinson’s disease medication − levodopa
- Damaged Bowel Tissue − When parts of the bowel plumbing itself are broken, there’s going to be problems. Hemorrhoids, anal fissures, hernias, diverticulitis (pouches in the intestine), bowel prolapses, tumors, and scarring can all interfere with peristalsis, bowel function and cause pain that encourages the resident to avoid going to the bathroom. The condition and the pain increase constipation, and constipation further aggravates the condition and causes more pain. It can become a downward spiral of bowel problems that the caregiver has to contend with. Caregiver understanding, encouragement, and support of normal bowel behaviors can go a long way in breaking the cycle.
- General Infirmities- When the overall patient is in a weakened state, it does not take much to push them into constipation problems. The elderly, the bedridden or sedentary, tube feeders, and out-of-control mental health residents should all be monitored for constipation problems. Caregivers should increase monitoring when there is any major change. You should anticipate problems when there is a change in routine, a hospitalization, or when there is an increase in stress.
The Roles of the Caregiver in Constipation Care
Having a basic knowledge of the working of the bowels and constipation is only the beginning. In order to be a good caregiver, you have to be able to apply that knowledge for the betterment of your residents. The proper application of knowledge is what I will call ‘being a savvy caregiver.’ Let’s see if I can help turn you into that savvy caregiver!
The bottom line (excuse the pun) of constipation care is to recognize it as a symptom that has resulted from a number of possibilities, not as a disease that needs a cure. When constipation occurs, the first thoughts of a truly efficient and effective caregiver are: “What has gone wrong, and how can I control it?” If you reach for the laxative first without this first step, you might have doomed the resident to further constipation once the laxative wears off. In plain terms, you resolve constipation, not cure it.
The savvy caregiver will realize that this change in emphasis has added several layers of complexity to their job. They are going to have to become a researcher, monitor, patient advocate, and symptom manager. But the savvy caregiver will also realize that if they get those roles right, their job will actually get easier. Bouts of constipation will become fewer and be more easily managed. Let’s talk about these different caregiver roles that will be required of you:
The primary goal of bowel care in foster care is maintaining bowel regularity. That first involves knowing what ‘regular’ means for each resident. Unpleasant as it sounds, you will be required to pay attention to when the resident goes to the bathroom and research what goes on in there. I know it might be an embarrassing and uncomfortable thought. Take comfort in knowing that this is the role the resident expects from you. It will be a natural occurrence for you to ask questions about their bowel movements. Being pleasant, confident, consistent and professional takes the edge off of the task.
Here are a few other ideas that I think will help:
- Pay attention to what is in the commode in the morning before cleaning it.
- Ask the resident not to flush the toilet and then notify you when they are done.
- Listen for sounds of straining.
- Take note of the frequency of trips to the bathroom.
- Phrase questions in professional terms. For example, use bowel movement or BM instead of ‘going potty.’
Once you get a handle on what being regular means for each resident, it’s time to switch roles to that of a monitor. Monitoring involves always being aware of what is going on in the lives of your residents. Savvy caregivers are always on the lookout for the signs that something has changed.
The signs of constipation include:
- Lower abdominal discomfort
- A sense of incomplete evacuation (the feeling that you still have to ‘go’)
- Straining to have a bowel movement
- Nausea
- Rectal bleeding and/or anal fissures caused by hard stools
- Physiological distress and/or obsession with having bowel movements
- Headaches that accompany bowel discomfort
- Loss of appetite
- An increase in flatulence
A major portion of the information you gather while monitoring will come from communications with the resident. A savvy caregiver knows monitoring does not end there. You are going to have to interpret what the resident is saying and compare it to what you are observing. Most often you will believe what they are reporting to you, though that is not always the case. Sometimes, what you see in your monitoring will be more important than what the resident tells you when you question them. The following are some of the special cases that I have observed in my caregiving and pharmacy careers:
Over Reporting
Very few of your residents will have had any medical training. When you question them about constipation, their answers will be tainted by what they think they know—what they know about the bowels they picked up from who knows where. Some of their perceptions are correct, some are correct but described wrong, and some are a just flat-out myth. You won’t be able to do your job right until you get accurate information from them. That will happen only after you get rid of their misconceptions.
Misconceptions are driven by fear and myth. The truth will cut through misconception but only if it is given with empathy, patient explanation, and good communication techniques. In other words, your residents will not listen until they know you care and sympathize with them. Talk to your residents in ways they understand and give them enough time to assimilate the information—that is done by a consistent, proper follow-up.
“What does all that fluff and stuff mean?”, you ask. The first couple of times you ask them about their bowels, what they tell you will most likely be wrong or inaccurate. You will have to verify and clarify their answers with your own observations. For those bits of info you find wrong, you’ll have to properly educate them on what is actually going on. This is one of those tricks that turn caregivers into savvy caregivers.

Constipation Truth and Myth
- Pseudo constipation
One of the most common resident misconceptions about constipation is what is called pseudo constipation. It’s one of those “correct but described wrong” events. What they call constipation is actually a lack of consistency in bowel movements. The myth is, if you don’t have a bowel movement every day, you’re getting constipated. Some residents get fixated on daily consistency and try to achieve it through the misuse of laxatives. The misuse leads to laxative dependency, and the body loses its ability to regulate itself.
The truth is, being irregular is not the same as constipation. Bowel movements are variable and are dependent on what we have eaten and how active we’ve been. The truth is, if nothing has collected in the rectum, you don’t need a bowel movement. Modern medicine has observed that among healthy people, bowel movements can vary between three times a day and three times a week. Using this as a guideline, true constipation in healthy adults would only start to occur after about three days.
As a caregiver, if the resident reports that they are constipated, you have to ask yourself, “Is this a matter of consistency or constipation?” To find out, you’ll have to ask follow-up questions: “When was your last bowel movement?” “How active have you been?” Are there any contributing factors to consider? How healthy are they, or can the resident’s body take care of the problem itself? How psychologically stressed do they get if they don’t get a laxative? How solid is the stool when they do go? That’s a lot of questions. Over time, and with practice, you’ll get good at finding the true answers. At first, I recommend erring on the side of resident comfort. If there is pseudo constipation going on, it will take time to ease the resident out of it.
- Constipation is a sign of illness
Constipation is an illness that needs a cure (laxative). That is a flat-out myth. The truth is, constipation is not a disease that one catches like a cold. It is a symptom, which is to say that it is a natural consequence that is the result of other processes. The correct way to understand constipation as a symptom is, it is either a primary or secondary result of other events. Primary constipation is caused by natural body processes like not eating enough fiber. Secondary constipation is the result of separate disease processes like Irritable Bowel Syndrome or Chron’s disease. Sometimes, constipation is described as idiopathic, or the cause is just unknown.
It may seem like I am splitting hairs here, but this is actually a very important point to drive home to the resident. It means that instead of reaching for a laxative to ‘cure’ constipation, you work on correcting the underlining causes, and constipation goes away by itself. It’s a matter of trusting the body to take care of itself. Enforcing proper daily habits and good caregiving techniques will be your most powerful tools in fighting this myth. If there is a strong fear of constipation as a disease in the resident, reassure them that constipation only causes harm if it gets out of control. Tell them that you won’t let that happen.
- Toxins
Toxins in the stool is a fear myth. It leads the resident to believe that constipation causes toxins to build up in the bowels, and they will cause harm. As a pharmacist, this myth kind of makes me mad. You’ll notice that the persons pushing this myth the hardest are the ones trying to sell you something. They are trying to make money by whipping up a fear that constipation is causing the patient to poison themselves. What a bunch of hogwash! There have been pseudo scientists pushing this quackery for well over a century. They even went as far as creating clinics that administered coffee enemas and high colonics. If you take a closer look, you won’t find much credible scientific evidence to back up their claims. If you find yourself having to deal with this myth, start by telling them that a pharmacist told you that the main ingredients of these ‘de-toxifying’ products are just plain laxatives. Then ask them how many ‘local’ doctors do they personally know who actually prescribe detoxifiers, or how many pharmacists recommend their purchase. The answer is, “None do.”
Underreporting
There are times when constipation issues keep reoccurring without any apparent medical reason. Full-blown bowel problems just seem to appear out of nowhere. In my experiences, I discovered three possible root causes of these mysterious occurrences:
- Suffering in silence
 Modesty is a powerful social consideration. At its core is the expectation of privacy. You just don’t let others see you in the bathroom with your pants down. Also, you don’t talk about what goes on in the bathroom. Some of your residents would rather suffer physically than suffer embarrassment. This leads to residents downplaying their symptoms and underreporting problems associated with their bowels.
Modesty is a powerful social consideration. At its core is the expectation of privacy. You just don’t let others see you in the bathroom with your pants down. Also, you don’t talk about what goes on in the bathroom. Some of your residents would rather suffer physically than suffer embarrassment. This leads to residents downplaying their symptoms and underreporting problems associated with their bowels.
- Fear and avoidance
Privacy concerns can lead your residents to fear going to the bathroom in public or unfamiliar places. As a result, residents ignore their bowel urges, causing constipation issues in normally regular clients. This is a particular concern in certain mental health and dementia cases and when the developmentally disabled are required to go into unfamiliar settings.
- Emotional stress
Emotional stress in mentally venerable populations can cause constipation. It’s part of the ‘flight or fight’ hormonal response to stress. Talking about it just adds to the stress, so they avoid the subject.
In these cases, monitoring for constipation can be problematic. The resident’s silence, emotions, and fear put up a wall that’s hard to see through. The solution to this problem is found in the realization that there are two exceptions to the modesty, privacy, and stress concerns. It is allowed and even expected to talk about bathroom concerns with your mother and medical professionals. Fortunately, adult foster care providers are naturally a little of both. The savvy caregiver can handle underreporting problems by:
- Looking for the social and physical clues that identify potential under-reporters.
- Establishing channels of open communications through empathetic and competent medical care.
- Setting expectations of regular bowel movement behaviors through a little bit of compassionate motherly bossing.
Being a Patient Advocate
Your caregiving role in constipation will be, for the most part, monitoring the patient and following doctors’ orders. There are times, though, when you have to take on the additional role of patient advocate. Constipation is a common occurrence and is easily solved through the use of laxatives. It is easy to lose sight of the fact that constipation is a symptom, and its chronic occurrence might be a sign of more serious concerns. Doctors are taught to actively look for critical concerns, but they are hampered by two problems:
- Doctors only see the patient every so often and only for a few minutes at a time. They have to rely on the patient and other caregivers to report problems.
- They are extremely busy and preoccupied with everyone’s problem. It’s easy to miss the lame pony when you have to corral a whole herd of horses. It’s understandable that mundane, easily remedied constipation issues are not taken very seriously.
Savvy caregivers know that it’s up to them to report serious concerns when they arise. They also know that they might have to become a bit of a thorn in the doctor’s foot. Sometimes, you’ll have to push a little bit to get the problem looked at seriously.
Communications with the Doctor
When interacting with other medical professions, it’s very important to be crystal clear in your communications. Just saying “My resident is constipated” is not going to be good enough to get the doctor’s attention. You are going to have to give facts and quantifiable details. Timeframes, the frequency of occurrences, numerical level of pain and discomfort on a 1−10 scale, and other related symptoms like nausea and vomiting should be in your communications and paperwork.
Blood in the stools or on underpants is an automatic trip to the doctor. The blood is going to be bright red or pink if it is from a surface cut or a major bleed internally. If it is a minor or moderate bleed internally, it will be mixed with the fecal material, giving it a distinctive order and texture. Look for black tarry stools or stools that look like coffee grounds.
In your communications, you will not be telling the doctor what the diagnosis is, but you can ask all the questions you want. It’s a polite way of being a pushy patient advocate. Put the question in writing, with a place for a written response. For example, “Could the increase in constipation be related to the new iron supplements you ordered? If so, what changes will you want me to follow-up on?” or “There has been a threefold increase in this month’s PRN laxative use. Could this be an indication that the increased stress behavior (or insert any other possible concern) needs to be looked at? Yes ___ No ____.” Don’t be afraid to use medical terminology. If you know it, use it. That will get the doctor’s attention faster.
Another important factor in communicating with doctors is: telling them what has changed. This will give the doctor important clues that will help them make a proper diagnosis. In order to know what is different, it is very important to know your resident inside and out. When thinking about the bowels, that ‘inside out’ statement takes on a whole new literal meaning.
Savvy caregivers will know which questions to periodically ask which resident. They will know that paying close attention to the PRN medicine logs makes it easier to see subtle changes in their residents. They will notice changes in behaviors and will not ignore an increase in a resident’s complaints. They will take note of a resident’s difficulty in accomplishing normal activities of daily living. They will also be on the lookout to see physical changes in the resident.
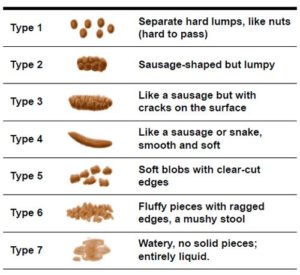
To help you recognize changes in stools and give a clearer report to the doctor, I recommend using the Bristol Stool Form Scale:
Being a Symptom Manager
There are two considerations in being a symptom manager in a care home. The first is: managing the lifestyle of the resident to prevent the problem. The second is: to manage the medical therapy ordered by the doctor to resolve the issue. But you already knew that it’s what the average adult foster caregiver does every day. I don’t want you to be average. My goal is to tell you what the savvy caregiver does to excel at what they do.
Prevention
To excel in bowel care, savvy caregivers should take the time to understand how the bowels work and set up their homes to maximize the body’s own bowel regulating processes. While there is no way to ensure never experiencing constipation, setting up your home routines using the following guidelines should help prevent constipation:
- Know what is normal for your residents − This includes knowing the difference between ‘wanting to go’ and ‘needing to go.’ Educating the resident about the difference can help gain their cooperation in your prevention efforts.
- Plan a well-balanced diet that includes plenty of fiber − Fiber retains water in the stools, and the extra bulk will help trigger the urge stretch receptor nerves in the rectum. Fiber can be found in bran, whole grains, dried beans, fresh fruits, and vegetables.
- Supply plenty of fluids − The thirst drive slackens as we age. To compensate, make drinking water part of the daily routine.
- Exercise regularly − Getting up and moving around also moves the stool around in the bowels. You also get a gravity assist when the resident is standing.

- Prunes and prune juice contain ingredients that make them a nutraceutical food. They are considered a natural drug-free laxative.
* A special note about the use of prunes as a therapy:
If you intend to add prunes or prune juice to resolve a case of constipation, you have come dangerously close to crossing the forbidden ‘choosing a therapy’ line. Keep yourself out of trouble by communicating with the doctor. The doctor should also know if you intend to add prune products as a regular daily menu item.
- Use daily routine to establish good bowel habits.
* A special note on habits as a caregiving tool:
Good habits are the caregiver’s best friend. Don’t underestimate the power of habit in the lives of your residents. Savvy caregivers actively work at setting routines and consistently enforce them.
- Schedule bathroom visits − Set aside time after breakfast or dinner for undisturbed visits to the toilet. Encourage residents not to ignore the urge to have a bowel movement.
- Regularly check on how much fluid is consumed − Remind them to drink when they are lacking.
- Schedule exercise time − Walking with the resident is my favorite recommendation to establish a habit. It is a beneficial activity on so many levels.
Medical Therapy
You might think that your role in medical therapy is to just follow doctors’ orders. The savvy caregiver knows that this is only part of their role. Following orders is not a robotic event. It’s not good enough to just blindly follow orders. You have to understand what the doctor is trying to do, ensure resident compliance, monitor for effect, and report your observations back to the doctor. In effect, the savvy caregiver turns themselves into the doctor’s advocate with the resident.
 Understanding what the doctor is trying to do
Understanding what the doctor is trying to do
The therapeutic choices made by the doctor are determined by what they think is needed to be done to resolve the underlying issues. Sometimes, the doctor’s rationale is not readily apparent. Caregivers should research and ask questions until they have a good handle on what the doctor is trying to do. It will help determine what to monitor for and how to educate the patient.
Here are few general things I have noticed that influence a doctor’s decision about constipation (it will help you in doing your research):
- Doctors differentiate between acute (recent onset) and chronic (long duration) constipation. They are treated differently.
- Prevention is always preferred overcorrection.
- If medication is needed, the choice pattern is least to the strongest. It is a stepwise methodology designed to preserve and utilize natural body processes and avoid chemical dependency for bowel function.
- Choosing products are always guided by what the prescriber is familiar with. If a patient wants a different medication, it’s going to be harder to get the doctor to agree.
Ensuring Resident’s Compliance
As the doctor’s advocate in the home, it is your job to help the patient cooperate with the doctor’s orders. Cooperation is a lot easier to obtain if the resident knows what is actually going wrong and has a realistic expectation of what the doctor can do about it. Translate what you know into a language the resident understands and dispel any myths you encounter.
For example, it is unrealistic to expect instant relief of constipation. Let the patient know that most laxatives take a day or two to start working. It is unlikely the resident will be harmed if they have to wait for relief. If that is not fast enough for the resident, and they start to demand an enema, teach the resident about item number 3 above. Knowing the facts helps the resident to have less anxiety and increases the resident’s confidence in the doctor’s recommendations.
Monitoring For Effect
As the doctor’s advocate, you are their eyes and ears. You have to watch to see if the choices they have made are actually doing what the doctor intended. You also have to watch for any unwanted side effects.
The acute resolution of constipation is easy enough to monitor, but what about chronic therapy? That’s where PRN logs come in handy. Watching the pattern of PRN med use can help you understand what is normal for your resident. If the PRN log entries start to show changes, it is a red-flag signal. Start looking closer at what is causing the change. It’s the old “a stitch in time save nine” thing.
There is one more thing I would like to note before getting into the actual constipation medication: Doctors don’t have crystal balls; they are always in the dark about what goes on with your resident. They can’t see your PRN logs. They will assume that everything is all right until somebody has a complaint. So, if things aren’t going right, let the doctor know. The more information you can provide to them, the better doctors they will be to your residents.

Medications
Most of the medications used for constipation are available ‘over the counter’ (OTC). That does not make them automatically a milder form of therapy. Some are very strong and carry with them dangers of misuse and dependency. Fortunately, selecting the appropriate drug is the doctor’s worry; your job is to monitor for effect and watch for unwanted side effects.
OTC Constipation Medications by Drug Effect
Lubricant/Emollient
Docusate (Colace, Surfak) softens the stools by adding fats and pulling in water. It does not have a laxative effect and is used mainly to help prevent straining. It is very well tolerated with little side effects and may take 1−3 days for effects to be seen.
Mineral Oil also has a softening effect but is mainly used as a lubricant. It can be taken orally, though it is most often used as an enema. It can be swallowed into the lungs (aspiration), where it will cause problems. It also tends to block absorption of vitamins in the bowels, so it is not for long-term use. If used as an enema, it can take up to 6−8 hours to work.
Bulk-forming
Psyllium (Metamucil, Konsyl), calcium polycarbophil (FiberCon), methylcellulose (Citrucel) are fiber supplement laxatives that work by pulling in water and adding bulk to the stools. The added bulk triggers the stretch receptor nerves that stimulate peristalsis and increases the urge ‘to go.’ They may take several days to start to work. In my experience, they are mainly used as a preventative. There is a danger that they could contribute to fecal impactions. They will also tend to create a bloated feeling and produce more gas.
Osmotic laxatives
Magnesium hydroxide (Milk of Magnesia), magnesium citrate (Citroma), polyethylene glycol (Miralax), sodium phosphate (Fleet Saline Enema), glycerin (Fleet Suppository) are stronger saline laxatives. They work by retaining water in the stool and pulling in more from the intestines. Their actions can be seen in as little as 30 minutes up to overnight. Be warned: they can cause cramping and add to dehydration problems. In some people, osmotic laxatives stop working if used continuously, so monitor for effect, even if they have been on it for a while.
Stimulant laxatives
Bisacodyl (Dulcolax Correctal), senna/sennoside (Senokot) stimulate the muscles of the intestines to contract, pushing the stools through faster. They take 6−8 hours to start working. Obviously, cramping may be an issue. There is also a strong possibility of tolerance and dependence developing with long-term use.
Some final notes:
- Chronic use of laxatives, especially enemas, can create dependency. If you are trying to help the resident regain normal function, it’s going to take time and patience.
- Watch the combination products Peri Colace and Sennakot S; even though they contain stool softeners, they are still stimulant laxatives.
- I always found that mixing bulk laxatives with orange juice, instead of water, made the taste more tolerable. You can get fiber supplements in pill form and graham cracker-like wafers, but they cost more. They can be used as alternatives if the residents don’t want to drink their fiber. Miralax is also an alternative; it’s supposed to be flavorless, but the texture may still be an issue.
Prescription Medications
Anti-constipation prescription drugs are usually used only when first-line therapy fails, or there is a specific need. If you are struggling with your current OTC therapy, they can be used as an alternative or as an add-on therapy. Before starting that conversation with the doctor, there are a few thoughts to keep in mind. Prescription drugs will cost more than OTC meds. In my opinion, they are not a more powerful alternative; most are a more specifically targeted therapy. Some are relatively new drugs, so the doctor might not have much experience with them.
Sugar syrups
Lactulose and Maltose are chemicals similar to sucrose (table sugar). They have a sweet taste, but we have a hard time digesting them. Most of it goes straight through to the bowels, where it pulls in extra fluids by osmosis. They can be used as sugar substitutes, but when taken in larger quantities, they have a laxative effect. Unfortunately, the bacteria in our gut have no problem digesting the chemical sugars, so there might be the extra side effects of gas, bloating, and cramps. As a prescription, they come in a thick maple syrup-like liquid. Adding active cultured yogurt to the diet might help control the gas.
Naclotide (Linzess)
Linzess mimics some of the body’s own mechanisms to draw water into the bowels. It has been approved for use in IBS and Idiopathic constipation. It should be taken 30 minutes before breakfast. It can cause severe dehydration in children, so it is not approved for children under 6. The side effects are diarrhea, gas, stomach pain, and headache. Linzess should not be crushed or chewed, but it can be taken apart and sprinkled over food or given via the NG tube.
Lubiprostone (Amitiza)
Amitiza works on the chloride channels of the gut, drawing in more fluid. It is used in a variety of conditions, including opioid-induced constipation. Common side effects may include nausea, stomach pain, diarrhea, gas, bloating, or a headache. Taking Amitiza with food can help control nausea if it becomes a problem.
Plecanatide (Trulance)
Trulance also mimics some of the body’s mechanisms to draw water into the bowels. Plecanatide is a new drug approved for chronic idiopathic constipation, with more disease therapy approvals likely to follow. It can be crushed and taken with or without food. The most common side effect is diarrhea.
Conclusion
We’ve covered a lot of material fairly extensively. You will notice that the skills required for resolving constipation problems will help improve the rest of your caregiving efforts. Those who master managing constipation therapy become better all-around caregivers.
It requires you to:
- understand the workings of the body
- adjust the resident’s lifestyle to maximize the natural bodily processes
- manage the chosen therapy—which includes researching, monitoring, educating, communicating, and understanding the chosen therapies
- being a patient and a doctor’s advocate
Hopefully, I have done my job and given you the potential to become a savvy caregiver. Now, it’s up to you to become one.
As always,
Good Luck with your caregiving efforts!
Mark Parkinson BS Pharm
References:
Dr Ananya Mandal, MD. Drugs that Cause Constipation. News Medical Life Sciences . Aug 3, 2017 https://www.news-medical.net/health/Drugs-that-Cause-Constipation.aspx
How the bowel works. Coloplast Stoma Care. Apr 5, 2013.https://www.youtube.com/watch?v=6CoIDScAzog
Tim Taylor,. Digestive System. Innerbody. http://www.innerbody.com/image/digeov.html
Constipation. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/constipation/symptoms-causes/syc-20354253
Gil Wayne, RN. Constipation. Nursing Labs. Aug 9 2012. https://nurseslabs.com/constipation/
Understanding Constipation. AGA Institute. brochure 375-057IND_12-1. http://www.gastro.org/patient-center/Understanding_Constipation_Brochure_Jan_2013.pdf
- Steven Pray, PhD, DPh. Gabriel E. Pray, PharmD Candidate. Counseling Patients About Constipation. US Pharmacist. US Pharm. 2013;38(12):8-11.https://www.uspharmacist.com/article/counseling-patients-about-constipation
Jeannette Y. Wick, RPh,. Finding Effective Relief for Constipation. Pharmacy Times. Jun. 24, 2013. http://www.pharmacytimes.com/publications/otc/2013/otcguide-2013/finding-effective-relief-for-constipation
Jay W. Marks, MD. Constipation (Relief, Home Remedies, Treatment Medications). MedicineNet.com. https://www.medicinenet.com/constipation/article.htm
Over-the-Counter and Prescription Constipation Medications. Healthline. https://www.healthline.com/health/constipation-medication#otc-medications2
Medicines to Treat Constipation. WebMD. https://www.webmd.com/digestive-disorders/prescription-medications-to-treat-constipation#1
Exam Portal
click on [Take Exam]
Purchase membership here to unlock Exam Portal.
|
|
|
|
|
*Important*
Registration and login is required to place your name on your CE Certificates and access your certificate history.
Username MUST be how you want your name on your CE Certificate.
| Guest: Purchase Exam |