Vitamin E – An Advanced CE
Vitamin E – An Advanced CE
Author: Mark Parkinson BsPharm: President AFC-CE
Credit Hours 3- Approximate time required: 180 min.
Educational Goal
To provide an advanced discussion on Vitamin E
Educational Objective
- Provide a description of the chemical shape of the vitamin E molecule preferred by the body.
- Explain Vitamin E’s roll as an antioxidant.
- Supply the Recommended Daily Allowance and pertaining information
- List and explain Caregiver concerns
- Quote evidence based research
Procedure:
Read the course materials. 2. Click on exam portal [Take Exam]. 3. If you have not done so yet fill in Register form (username must be the name you want on your CE certificate). 4. Log in 5. Take exam. 6. Click on [Show Results] when done and follow the instructions that appear. 7. A score of 70% or better is considered passing and a Certificate of Completion will be generated for your records.
Disclaimer
The information presented in this activity is not meant to serve as a guideline for patient management. All procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this article should not be used by care providers without evaluation of their patients’ Doctor. Some conditions and possible contraindications may be of concern. All applicable manufacturers’ product information should be reviewed before use. The author and publisher of this continuing education program have made all reasonable efforts to ensure that all information contained herein is accurate in accordance with the latest available scientific knowledge at the time of acceptance for publication. Nutritional products discussed are not intended for the diagnosis, treatment, cure, or prevention of any disease.
Vitamin E – An Advanced CE
An advanced CE about vitamin E has been requested by a subscriber, and as you all know, I take requests. The requestor has a nursing degree and wanted to have a course with a little more meat on the bone to chew on. So as fair warning to all my other subscribers, this article will be a little more challenging. Struggle is good, though; it will make you stronger. As always, I will endeavor to make this pertinent to foster caregiving, with knowledge you can use in your homes. I also would like to think that this will not be beyond the understanding of the average caregiver. I do recommend that those without medical degrees take the CE The Vitality of Vitamins before tackling this one. If this is not your flavor of ice cream, then please enjoy my other CEs. So let’s get to it.
There is a lot of useless chatter or downright inaccuracies surrounding vitamins, none more so than vitamin E. Don’t believe everything you hear—especially from those who want you to send them money for their miracle cure. It’s true that vitamin E is an essential vitamin, but it is not the cure-all that everyone says it is. What is needed is a conversation that is backed up by good, solid evidence so that caregivers can use the information in their practice without concerns for its validity.
More Than One Vitamin E
Vitamin E is a chemical needed for good health that is not produced by the human body. It can be found naturally in foods, as a food additive, and as a dietary supplement. The fat-soluble organic compound known as vitamin E, chemically named tocopherol, comes in eight different isoforms. Isoforms are differentiated by slightly different shapes of the same organic compound. The version preferred by our bodies is alpha-tocopherol. When we consume vitamin E, it is absorbed through the wall of the small intestine and transported to the liver. In the liver, α-tocopherol is preferentially transported to the rest of the body via a special protein called the hepatic alpha-tocopherol transfer protein. All other versions are metabolized and removed by the liver. Natural, plant-produced, α-tocopherol comes as an RRR-shaped organic molecule. Synthetically produced vitamin E usually results in a combination of different racemic versions that may not be as bio-availably active as the naturally produced molecule.
To understand the impact different shapes of the same molecule have on your body, consider your hands. They are identical, but they come in a right- and a left-hand version. If you are right-handed and all you have available is a left-handed glove, it’s kind of hard to catch a baseball. The caregiver takeaway is that the natural version produced by plants is chemically better suited to be utilized by the body. Therefore, dietary intake of vitamin E in the foods we eat is medically preferred.
Antioxidation and Vitamin E
α-Tocopherol is used by the body primarily as a fat-soluble antioxidant. To understand the significance of this chemical property, let us consider the fat molecule. Fat molecules are utilized throughout the body. They are an integral part of all cell membranes. They are transported through the bloodstream as part of a larger molecule known as a lipoprotein. Unfortunately, fat molecules are highly susceptible to damage by other molecules called free radicals.
Free Radicals and Oxidation
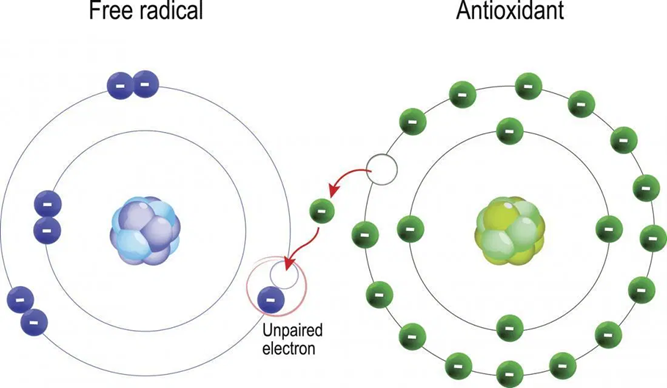
Free radicals are molecules that have lost at least one of their electrons. When free radicals come in contact with other molecules, they steal an electron away. When a molecule loses an electron, the reaction is called oxidation. With a missing electron, the affected molecule is not able to function as well. In addition, it becomes a free radical itself and tries to steal an electron from its neighbors. Thus, the damage is passed to other molecules. When the damaged molecules are part of a cell wall or part of the nucleus, the entire cell can become damaged. In addition to cellular damage, oxidized fat molecules are also known contributing factors of many disease states.
Free-radical molecules are all around us and in us. They are a natural byproduct of the chemical process of turning our food into energy. Our immune system produces free radicals as a weapon, to damage or kill bacteria and viruses. Free radicals are also found in our environment. They come from sources such as smoking, ultraviolet radiation, sunlight radiation, power lines, and air pollution. Fortunately, we have a protection against free radicals: antioxidants.
Antioxidants
Antioxidants are molecules that can give an electron away without becoming a free radical themselves. They stop the oxidation chain reaction that can cause so much cellular damage. Vitamin E is one of our most potent antioxidant protections. As a fat-soluble molecule, vitamin E can freely mix with the rest of the body’s fat molecules. Being thus positioned, it is available to stop oxidation when it starts to occur. Other antioxidants like vitamin C cannot mix with fats and thus are not as readily available to protect our fat molecules. In addition, vitamin A, another fat-soluble vitamin, is easily destroyed by oxidation. The antioxidant effect of vitamin E enables vitamin A to survive longer, thus potentiating its essential effect in the body.
The caregiver takeaway is that free radicals are bad and antioxidants are good.
Other Known Functions
Vitamin E is also involved in other bodily functions, such as our immune system, regulation of gene expression, and the chemical pathways of cell signaling.
A few examples are:
- It slows down the activity of protein kinase C, an enzyme involved in cell proliferation and differentiation in smooth muscle cells, platelets, and monocytes. In other words, it helps turn off those functions
- When vitamin E combines with endothelial cells lining the inside surface of blood vessels, they are better able to resist blood-cell components adhering to their surface, making it harder for plaque to build up. Plaque leads to hardened and clogged arteries.
- Vitamin E also increases the expression of two enzymes that suppress arachidonic acid metabolism. This reaction leads to an increase in the release of prostacyclin from the lining of blood vessel walls. Prostacyclin tends to dilate blood vessels and inhibit platelet aggregation.
Having Enough Vitamin E
Once the α-tocopherol molecule gives up its electron, it ceases to function as an antioxidant and must be replaced by the body. Also, the body’s regular metabolism will deplete its vitamin E stores. We find ourselves in a constant need to intake more vitamin E. But how much do we need?
Recommended Daily Allowance (RDA)
The Food and Nutrition Board of the U.S. Institute of Medicine publishes guidelines that tell us a recommended daily allowance (RDA) of the essential vitamins and minerals we need to maintain good health. In 2000, it revised its recommendation for the daily allowance of vitamin E as follows.
* IU – International Unit, as seen on the labels of some manufacturer’s bottles.
The RDA is based primarily on the concentration of α-tocopherol that protects red blood cells (erythrocytes) when exposed to hydrogen peroxide, a potent free radical source.
There are limitations to the usefulness of the RDA when it’s calculated using this method. It fails to measure the other needs of the body for vitamin E. There is also uncertainty caused by variability in what types of tocopherol are supplied to the body (remember the right- and left-hand molecule example above). In addition, the RDA amount will be inadequate when the need for vitamin E increases. For example, tobacco smoke puts extra free radicals into our bodies. Another example is that fat malabsorption conditions prevent normal absorption of vitamin E into the bloodstream. This is an important point that caregivers need to understand in greater depth.
Absorption into the Bloodstream
 The full explanation of how vitamin E gets into the bloodstream from the food we eat remains unclear. We do know that bile acids and pancreatic enzymes are required for vitamin E to get from our gut into our bloodstream. We also know that when we consume a tocopherol molecule, it is combined with our dietary fat. The combination results in a chylomicron molecule that is transported through the intestinal wall. It has also been discovered that vitamin E absorption increases with the amount of fat ingested in our foods. The chylomicron then travels to the liver, where it is processed further. It is then sent into the bloodstream. Once in the bloodstream, the molecule can combine with circulating lipoproteins and be transported throughout the body.
The full explanation of how vitamin E gets into the bloodstream from the food we eat remains unclear. We do know that bile acids and pancreatic enzymes are required for vitamin E to get from our gut into our bloodstream. We also know that when we consume a tocopherol molecule, it is combined with our dietary fat. The combination results in a chylomicron molecule that is transported through the intestinal wall. It has also been discovered that vitamin E absorption increases with the amount of fat ingested in our foods. The chylomicron then travels to the liver, where it is processed further. It is then sent into the bloodstream. Once in the bloodstream, the molecule can combine with circulating lipoproteins and be transported throughout the body.
Interference
There are numerous factors that can affect the absorption and transport of the vitamin E we consume. These factors are usually related to either genetic defects, or problems with the absorption or metabolism of dietary fats. For example, after the gall bladder is removed, the lack of bile acids will cause issues with fat- and fat-soluble vitamin metabolism. Symptoms of serious deficiencies are usually neurological problems, as seen in impaired balance and coordination, neuropathy, or muscle weakness. Retinopathy may also occur.
The caregiver takeaways are that the RDA intake of vitamin E is just the starting point—more may be needed. The caregiver should be ready to have a discussion with the resident’s doctor if deficiency symptoms start to appear.
Problems with Getting Enough Vitamin E
While serious deficiencies of vitamin E are rare, marginal deficiencies are quite common. The National Health and Nutrition Examination Surveys (NHANES) conducted by the National Center for Health Statistics demonstrated that vitamin E intake from the American diet is too low. In a series of studies conducted between 1980–1990 and 2003–2006, it was shown that more than 93 percent of American adults were below the RDA requirement. It can be concluded that a change in the average diet is needed. The question that remains is what specific changes are needed to consistently ensure that the RDA is achieved.
Vitamin E Food Sources
There are many foods that are rich in vitamin E that can be easily added to a normal diet. They include nuts, seeds, vegetable oils, green leafy vegetables, and vitamin-fortified cereals. Knowing how much of each item to add to the diet can be problematic. The FDA does not require food labels to list vitamin E content unless vitamin E has been added to the food. To determine how much of each food item to add to the diet, reference materials like the one listed below must be consulted.
Vitamin E Quantities in Food
|
Food |
Milligrams (mg) |
Percent DV* |
|
Wheat germ oil, 1 tablespoon |
20.3 |
135 |
|
Sunflower seeds, dry roasted, 1 ounce |
7.4 |
49 |
|
Almonds, dry roasted, 1 ounce |
6.8 |
45 |
|
Sunflower oil, 1 tablespoon |
5.6 |
37 |
|
Safflower oil, 1 tablespoon |
4.6 |
31 |
|
Hazelnuts, dry roasted, 1 ounce |
4.3 |
29 |
|
Peanut butter, 2 tablespoons |
2.9 |
19 |
|
Peanuts, dry roasted, 1 ounce |
2.2 |
15 |
|
Corn oil, 1 tablespoon |
1.9 |
13 |
|
Spinach, boiled, ½ cup |
1.9 |
13 |
|
Broccoli, chopped, boiled, ½ cup |
1.2 |
8 |
|
Soybean oil, 1 tablespoon |
1.1 |
7 |
|
Kiwifruit, 1 medium |
1.1 |
7 |
|
Mango, sliced, ½ cup |
0.7 |
5 |
|
Tomato, raw, 1 medium |
0.7 |
5 |
|
Spinach, raw, 1 cup |
0.6 |
4 |
Source: https://ods.od.nih.gov/factsheets/VitaminE-HealthProfessional/
About the DV
DV stands for daily value and is based on 15 mg per day from all food sources. It is a convenient way to compare which foods are good sources of vitamin E. Foods that contain 20 percent or more of the DV are considered to be rich sources.
Menu Planning
When considering vitamin E requirements, knowing which food and how much to add to the diet is the easy part. Trying to plan out a menu with a specific nutritional goal in mind is much more difficult. There are numerous factors that can interfere with achieving a nutritional goal, such as:
- Food preferences and food allergies of the residents
- Cooking skill of the chef
- Cooking methods that affect how much vitamin E is consumed
- Other dietary needs that affect vitamin E quantities (e.g., low-fat diets would reduce the amount of fat-dependent vitamin E absorption in the intestine)
- Health conditions that affect digestion and fat absorption.
The caregiver takeaway is unless you’re a registered dietitian, achieving the RDA with just menu planning will be challenging. Taking a vitamin supplement may be required.
Supplements
The average American diet supplies about 7.2 mg of vitamin E per day for adults. This level is well below the 15 mg per day RDA. In addition, the typical foster care resident is far from average. Your residents have extra needs and special circumstances that warrant taking vitamin supplements. If one of your residents is not taking vitamin supplements, it might be time to have a conversation with the doctor about that. But first, let me share with you a few details about vitamin E and supplements in general so that you can have an informed conversation with the doctor.
There is an overwhelming number of choices in purchasing vitamin supplements. There are liquid vitamins, naturally sourced vitamins, synthetic vitamins, and chewable and gummy varieties. I even remember seeing a chewing gum vitamin for children. Here are a few considerations that will help make sense of it all.
- Naturally sourced vitamins may be more potent. For example, vitamin E from plant sources will provide one form of α-tocopherol, while synthetic sources contain a variety of isoforms. The result is 100 IU of natural vitamin E provides 67 mg of RRR-α-tocopherol, the form preferred by the body, while 100 IU of a synthetic vitamin E provides only 45 mg of RRR-α-tocopherol.
- Vitamin supplements are just that—supplemental to what you take in from your diet. Don’t get caught up in the details of a particular brand or trying get the exact amount to satisfy the RDA. The effort is just not necessary. For example, vitamin E supplements typically far exceed the RDA. I randomly looked at two common multivitamin brands. One had 167 percent and the other had 150 percent of the RDA. That’s more than enough, even if they are synthetic sources.
- Vitamin supplements come in different forms that the caregiver can take advantage of, such as liquid and chewable varieties for those who have troubles swallowing, gummy varieties for those who hate pills, etc. Have the doctor write the prescription for that specific variety.
- As a supplement, vitamins are not regulated by the FDA. That means the government regulates the quantities but not the quality of the supplement.
 A Word About Topical Vitamin E
A Word About Topical Vitamin E
Vitamin E is added to many skin products. Its fat solubility and antioxidant properties make it a desirable ingredient in products that claim antiaging and healing abilities. There are some medical studies that back up some of these claims. The therapeutic effects of these products are mostly topical, though. Almost none of the vitamin E is absorbed into the bloodstream. The skin has both fat-soluble and water-soluble qualities. Being only fat-soluble, vitamin E cannot make it past the skin barrier. Since the effects are mostly cosmetic, I will not be covering any further details except for two items:
- There are those who like to pop the gel versions and spread the oil over the skin. Caregivers beware, that crosses over into the therapy zone and you have to get the doctor’s permission.
- There are some studies that show a therapeutic benefit of vitamin E for eczema and psoriasis sufferers. In these cases, it might be worth it to have the conversation with the doctor. See the following articles if you want more details.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4976416/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4755091/
Other Caregiver Considerations
Can you take too much vitamin E? The answer is yes. Normally, in a foster care setting, it’s very hard to do, so it’s not really a caregiver concern. But there are some circumstances that need careful caregiver considerations. Most of the time, there will not be any significant health issues, though it is an easy thing for the doctor to have overlooked tocopherol’s side effects. If there are any concerns, have a talk with the doctor.
Vitamin E may inhibit vitamin K-dependent carboxylase activity and interfere with the coagulation cascade. This will lead to impaired blood clotting. Normally at doses less than 1,000 mg a day, the effect will be negligible. It might even be helpful in preventing strokes cause by blood clots (ischemic strokes). But there are circumstances when things aren’t normal.
- Surgery – If the resident is scheduled for any type of procedure that may cause significant bleeding (including dental procedures), it may be wise to ask the doctor if they wish to discontinue the vitamin E supplement a few weeks before surgery.
- Blood thinners – The doctor should be consulted about vitamin E supplements if the resident is on any of the following drugs: Heparin, warfarin (Coumadin), clopidogrel (Plavix), ticlopidine (Ticlid), tirofiban (Aggrastat), and dipyridamole (Aggrenox).
- Painkillers – Non-steroidal anti-inflammatories (NSAIDS) and aspirin can also thin the blood. In my opinion, though, unless the resident is on a continual dose, it is not worth bringing the issue up with the doctor.
Retinitis Pigmentosa
Residents with retinitis pigmentosa should avoid higher doses of vitamin E. In a study of 601 patients with common forms of retinitis pigmentosa (RP) supplementation with 400 IU/day of synthetic vitamin E (equivalent to 180 mg/day of RRR-α-tocopherol) modestly but significantly accelerated the loss of retinal function compared to placebo. Any dose above the RDA of α-tocopherol would warrant a discussion with the doctor.
Other Health Concerns
Caregivers should talk with the doctor about vitamin E supplements if the resident has any of the following conditions:
- Liver failure
- Bleeding peptic ulcer
- Hemophilia
- History of hemorrhagic stroke (stroke caused by bleeding in the brain area)
Drug Interactions
Vitamin E, in all its isomeric forms, is a chemical that can interact with and change the effect of other chemicals in the body. There are many drugs that interact with vitamin E. In my opinion, the following are the ones that can have a significant interaction:
 Mephyton
Mephyton- Phenobarbital
- Phenytoin (Dilantin)
- Carbamazepine (Tegretol)
- Cyclosporine (Neoral, Sandimmune)
- Ketoconazole (Nizoral)
- Itraconazole (Sporanox)
- Cancer drugs (vitamin E might lessen their effects)
If you see any of these medications on the resident’s MARS, increase your side-effect monitoring until you’re satisfied that no issues are occurring. You can also bring up any drug concerns with your pharmacist.
Herbs
Just to be complete, there are herbs that can potentiate the blood-thinning side effect of vitamin E. These would be fish oil, garlic, or Ginkgo biloba supplements. In my opinion, they are not a big deal unless there are other serious underlying health concerns like the ones mentioned above.
The caregiver takeaway is that vitamin E supplements can have significant interactions with health problems and other drugs and herbs. The larger the dose of vitamin E or the more serious the resident’s condition, the greater the need for close patient monitoring.
The Role of Vitamin E and Diseases
Many health claims have been attributed to the taking of vitamin E supplements. The reason for these assertions needs to be examined first to help determine which to pay attention to and which to ignore.
As an antioxidant, and as a chemical component of cellular mechanisms, vitamin E has the potential of affecting every cell in our body. Whether it actually affects a cell is hard to determine. In order to determine an actual event, you have to be able to measure an effected biomarker. A biomarker is a measurable substance in an organism whose presence is indicative of a biological occurrence. Currently, it is very hard to find biomarkers relating to vitamin E metabolism. Without vitamin E biomarkers, there are many who make claims that are based on the potential effect of vitamin E without the actual evidence that proves it. When such claims come under the scrutiny of outcomes research, some of these claims are questionable at best.
 Research Evidence
Research Evidence
I am just an old country pharmacist who has spent a lot of time in care homes. I am in no way any kind of research specialist. I am uncomfortable writing in my own words about research studies I know little about. So, I am just going to quote verbatim from some trusted sources that I have found.
Vitamin E Fact Sheet for Health Professionals, National Institutes of Health (NIH)
Source: https://ods.od.nih.gov/factsheets/VitaminE-HealthProfessional/
Coronary heart disease
Evidence that vitamin E could help prevent or delay coronary heart disease (CHD) comes from several sources. In vitro studies have found that the nutrient inhibits oxidation of low-density lipoprotein (LDL) cholesterol, thought to be a crucial initiating step for atherosclerosis. Vitamin E might also help prevent the formation of blood clots that could lead to a heart attack or venous thromboembolism.
Several observational studies have associated lower rates of heart disease with higher vitamin E intakes. One study of approximately 90,000 nurses found that the incidence of heart disease was 30 to 40 percent lower in those with the highest intakes of vitamin E, primarily from supplements. Among a group of 5,133 Finnish men and women followed for a mean of 14 years, higher vitamin E intakes from food were associated with decreased mortality from CHD.
However, randomized clinical trials cast doubt on the efficacy of vitamin E supplements to prevent CHD. For example, the Heart Outcomes Prevention Evaluation (HOPE) study, which followed almost 10,000 patients at high risk of heart attack or stroke for 4.5 years, found that participants taking 400 IU/day of natural vitamin E (268 mg) experienced no fewer cardiovascular events or hospitalizations for heart failure or chest pain than participants taking a placebo. In the HOPE-TOO follow-up study, almost 4,000 of the original participants continued to take vitamin E or placebo for an additional 2.5 years. HOPE-TOO found that vitamin E provided no significant protection against heart attacks, strokes, unstable angina, or deaths from cardiovascular disease or other causes after 7 years of treatment. Participants taking vitamin E, however, were 13 percent more likely to experience, and 21 percent more likely to be hospitalized for, heart failure, a statistically significant but unexpected finding not reported in other large studies.
The HOPE and HOPE-TOO trials provide compelling evidence that moderately high doses of vitamin E supplements do not reduce the risk of serious cardiovascular events among men and women >50 years of age with established heart disease or diabetes. These findings are supported by evidence from the Women’s Angiographic Vitamin and Estrogen study, in which 423 postmenopausal women with some degree of coronary stenosis took supplements with 400 IU vitamin E (form not specified) and 500 mg vitamin C twice a day or placebo for >4 years. Not only did the supplements provide no cardiovascular benefits, but all-cause mortality was significantly higher in the women taking the supplements.
The latest published clinical trial of vitamin E’s effects on the heart and blood vessels of women included almost 40,000 healthy women ≥45 years of age who were randomly assigned to receive either 600 IU of natural vitamin E (402 mg) on alternate days or placebo and who were followed for an average of 10 years. The investigators found no significant differences in rates of overall cardiovascular events (combined nonfatal heart attacks, strokes, and cardiovascular deaths) or all-cause mortality between the groups. However, the study did find two positive and significant results for women taking vitamin E: they had a 24 percent reduction in cardiovascular death rates, and those ≥65 years of age had a 26 percent decrease in nonfatal heart attack and a 49 percent decrease in cardiovascular death rates.
The most recent published clinical trial of vitamin E and men’s cardiovascular health included almost 15,000 healthy physicians ≥50 years of age who were randomly assigned to receive 400 IU synthetic alpha-tocopherol (180 mg) every other day, 500 mg vitamin C daily, both vitamins, or placebo. During a mean follow-up period of 8 years, intake of vitamin E (and/or vitamin C) had no effect on the incidence of major cardiovascular events, myocardial infarction, stroke, or cardiovascular morality. Furthermore, use of vitamin E was associated with a significantly increased risk of hemorrhagic stroke.
In general, clinical trials have not provided evidence that routine use of vitamin E supplements prevents cardiovascular disease or reduces its morbidity and mortality. However, participants in these studies have been largely middle-aged or elderly individuals with demonstrated heart disease or risk factors for heart disease. Some researchers have suggested that understanding the potential utility of vitamin E in preventing CHD might require longer studies in younger participants taking higher doses of the supplement. Further research is needed to determine whether supplemental vitamin E has any protective value for younger, healthier people at no obvious risk of CHD.
Cancer
Antioxidant nutrients like vitamin E protect cell constituents from the damaging effects of free radicals that, if unchecked, might contribute to cancer development. Vitamin E might also block the formation of carcinogenic nitrosamines formed in the stomach from nitrites in foods and protect against cancer by enhancing immune function. Unfortunately, human trials and surveys that have attempted to associate vitamin E intake with cancer incidence have found that vitamin E is not beneficial in most cases.
Both the HOPE-TOO Trial and Women’s Health Study evaluated whether vitamin E supplements might protect people from cancer. HOPE-TOO, which followed men and women ≥55 years of age with heart disease or diabetes for 7 years, found no significant differences in the number of new cancers or cancer deaths between individuals randomly assigned to take 400 IU/day of natural vitamin E (268 mg) or a placebo. In the Women’s Health Study, in which healthy women ≥45 years of age received either 600 IU of natural vitamin E (402 mg) every other day or a placebo for 10 years, the supplement did not reduce the risk of developing any form of cancer.
Several studies have examined whether vitamin E intake and/or supplemental vitamin E affects the risk of developing prostate cancer. A prospective cohort study of >29,000 men found no association between dietary or supplemental vitamin E intake and prostate cancer risk. However, among current smokers and men who had quit, vitamin E intakes of more than 400 IU/day (form not specified) were associated with a statistically significant 71 percent reduction in the risk of advanced prostate cancer. In a clinical trial involving 29,133 male smokers, men randomly assigned to take daily supplements of 111 IU of synthetic vitamin E (50 mg, as dl-alpha-tocopheryl acetate) for 5–8 years had 32 percent fewer prostate cancers compared to subjects who did not take the supplements. Based in part on the promising results of this study, a large randomized clinical trial, called the SELECT trial, began in 2001 to determine whether 7–12 years of daily supplementation with 400 IU of synthetic vitamin E (180 mg, as dl-alpha-tocopheryl acetate), with or without selenium (200 mcg, as L-selenomethionine), reduced the number of new prostate cancers in 35,533 healthy men age 50 and older. The trial was discontinued in October 2008 when an analysis found that the supplements, taken alone or together for about 5.5 years, did not prevent prostate cancer. Results from an additional 1.5 years of follow-up from this trial (during which the subjects no longer received vitamin E or selenium), showed that the men who had taken the vitamin E had a 17 percent increased risk of prostate cancer compared to men only taking placebos, a statistically significant difference. The risk of developing prostate cancer was also slightly increased in subjects taking vitamin E plus selenium or selenium alone, but the differences were not statistically significant. No differences were found among groups in the incidence of lung or colorectal cancers or all cancers combined. Study staff members will continue to monitor participants’ health for up to 5 more years. The National Cancer Institute website provides additional information on the SELECT trial.
One study of women in Iowa provides evidence that higher intakes of vitamin E from foods and supplements could decrease the risk of colon cancer, especially in women <65 years of age [34]. The overall relative risk for the highest quintile of intake (>35.7 IU/day, form not specified) compared to the lowest quintile (<5.7 IU/day, form not specified) was 0.32. However, prospective cohort studies of 87,998 women in the Nurses’ Health Study and 47,344 men in the Health Professionals Follow-up Study failed to replicate these results. Although some research links higher intakes of vitamin E with decreased incidence of breast cancer, an examination of the impact of dietary factors, including vitamin E, on the incidence of postmenopausal breast cancer in >18,000 women found no benefit from the vitamin.
The American Cancer Society conducted an epidemiologic study examining the association between use of vitamin C and vitamin E supplements and bladder cancer mortality. Of the almost one million adults followed between 1982 and 1998, adults who took supplemental vitamin E for 10 years or longer had a reduced risk of death from bladder cancer; vitamin C supplementation provided no protection.
Evidence to date is insufficient to support taking vitamin E to prevent cancer. In fact, daily use of large-dose vitamin E supplements (400 IU of synthetic vitamin E [180 mg]) may increase the risk of prostate cancer.
Eye Disorders
Age-related macular degeneration (AMD) and cataracts are among the most common causes of significant vision loss in older people. Their etiologies are usually unknown, but the cumulative effects of oxidative stress have been postulated to play a role. If so, nutrients with antioxidant functions, such as vitamin E, could be used to prevent or treat these conditions.
Prospective cohort studies have found that people with relatively high dietary intakes of vitamin E (e.g., 20 mg/day [30 IU]) have an approximately 20 percent lower risk of developing AMD than people with low intakes (e.g., <10 mg/day [<15 IU]). However, two randomized controlled trials in which participants took supplements of vitamin E (500 IU/day [335 mg] d-alpha-tocopherol in one study and 111 IU/day (50 mg) dl-alpha-tocopheryl acetate combined with 20 mg/day beta-carotene in the other or a placebo failed to show a protective effect for vitamin E on AMD. The Age-Related Eye Disease Study (AREDS), a large randomized clinical trial, found that participants at high risk of developing advanced AMD (i.e., those with intermediate AMD or those with advanced AMD in one eye) reduced their risk of developing advanced AMD by 25 percent by taking a daily supplement containing vitamin E (400 IU [180 mg] dl-alpha-tocopheryl acetate), beta-carotene (15 mg), vitamin C (500 mg), zinc (80 mg), and copper (2 mg) compared to participants taking a placebo over 5 years. A follow-up AREDS2 study confirmed the value of this and similar supplement formulations in reducing the progression of AMD over a median follow-up period of 5 years.
Several observational studies have revealed a potential relationship between vitamin E supplements and the risk of cataract formation. One prospective cohort study found that lens clarity was superior in participants who took vitamin E supplements and those with higher blood levels of the vitamin. In another study, long-term use of vitamin E supplements was associated with slower progression of age-related lens opacification. However, in the AREDS trial, the use of a vitamin E-containing (as dl-alpha-tocopheryl acetate) formulation had no apparent effect on the development or progression of cataracts over an average of 6.3 years. The AREDS2 study, which also tested formulations containing 400 IU (180 mg) vitamin E, confirmed these findings.
Overall, the available evidence is inconsistent with respect to whether vitamin E supplements, taken alone or in combination with other antioxidants, can reduce the risk of developing AMD or cataracts. However, the formulations of vitamin E, other antioxidants, zinc, and copper used in AREDS hold promise for slowing the progression of AMD in people at high risk of developing advanced AMD.
Cognitive Decline
The brain has a high oxygen consumption rate and abundant polyunsaturated fatty acids in the neuronal cell membranes. Researchers hypothesize that if cumulative free-radical damage to neurons over time contributes to cognitive decline and neurodegenerative diseases, such as Alzheimer’s disease, then ingestion of sufficient or supplemental antioxidants (such as vitamin E) might provide some protection. This hypothesis was supported by the results of a clinical trial in 341 patients with Alzheimer’s disease of moderate severity who were randomly assigned to receive a placebo, vitamin E (2,000 IU/day dl-alpha-tocopherol), a monoamine oxidase inhibitor (selegiline), or vitamin E and selegiline. Over 2 years, treatment with vitamin E and selegiline, separately or together, significantly delayed functional deterioration and the need for institutionalization compared to placebo. However, participants taking vitamin E experienced significantly more falls.
Vitamin E consumption from foods or supplements was associated with less cognitive decline over 3 years in a prospective cohort study of elderly, free-living individuals aged 65–102 years [49]. However, a clinical trial in primarily healthy older women who were randomly assigned to receive 600 IU (402 mg) d-alpha-tocopherol every other day or a placebo for ≤4 years found that the supplements provided no apparent cognitive benefits. Another trial in which 769 men and women with mild cognitive impairment were randomly assigned to receive 2,000 IU/day vitamin E (form not specified), a cholinesterase inhibitor (donepezil), or placebo found no significant differences in the progression rate of Alzheimer’s disease between the vitamin E and placebo groups.
In summary, most research results do not support the use of vitamin E supplements by healthy or mildly impaired individuals to maintain cognitive performance or slow its decline with normal aging. More research is needed to identify the role of vitamin E, if any, in the management of cognitive impairment.
Vitamin E, Oregon State University, Linus Pauling Institute
Source: https://lpi.oregonstate.edu/mic/vitamins/vitamin-E
Age-Related Deterioration of Immune Function
A randomized, placebo-controlled trial in 617 nursing home residents (≥65 years of age) reported that daily supplementation with 200 IU of synthetic α-tocopherol (90 mg of RRR-α-tocopherol) for one year significantly lowered the risk of contracting upper respiratory tract infections, especially the common cold, but had no effect on lower respiratory tract (lung) infections. More research is needed to examine whether supplemental vitamin E might enhance immune function and reduce risk of infection in older adults.
Type 2 Diabetes Mellitus
Oxidative stress contributes to the progression of type 2 diabetes mellitus and causes damage to many organs and tissues, including the pancreas, brain, eyes, peripheral nerves, and kidneys. Evidence from animal studies suggests that vitamin E supplementation could mitigate the role of oxidative damage in the occurrence of diabetes complications. In the Alpha-Tocopherol Beta-Carotene cancer prevention (ATBC) trial in male smokers, supplementation with 50 mg/day of synthetic α-tocopherol (25 mg/day of RRR-α-tocopherol) had no effect on the risk of incident type 2 diabetes mellitus during the 19-year post-intervention follow-up. Likewise, supplemental vitamin E intake during the trial made no difference on the incidence of macrovascular complications or mortality in participants with established type 2 diabetes. In addition, a meta-analysis of 14 heterogeneous randomized controlled trials, including 714 type 2 diabetic individuals, found that supplementation with vitamin E (200-1,800 IU/day for 6-27 weeks) had no effect on markers of glycemic control, including glycated hemoglobin A1c (HbA1c) level and measures of fasting glucose and fasting insulin concentrations. Further subgroup analyses indicated that higher doses of vitamin E (>400 IU/day) supplemented for longer periods (>12 weeks) significantly reduced HbA1c level and fasting insulin concentration, suggesting that vitamin E could possibly enhance insulin action and glucose disposal in type 2 diabetic individuals. Another recent meta-analysis of randomized controlled trials found that endothelial function in normal-weight and overweight—but not obese—patients with type 2 diabetes was significantly improved by supplementation with vitamin E and/or vitamin C. Although there is reason to suspect that vitamin E supplementation may have utility in the management of type 2 diabetes, evidence for benefit from large, well-controlled clinical trials is still lacking.
The caregiver takeaway is that many health claims of vitamin E products are in actuality just unproven theories of potential benefits. Only those claims based on actual clinical outcome studies are worth your attention.
Conclusion
 How’s that for a CE with some meat on the bone? I hope that satisfied the appetites of my more advanced subscribers without losing the interest of everyone else. To recap, the topics I have covered are as follows:
How’s that for a CE with some meat on the bone? I hope that satisfied the appetites of my more advanced subscribers without losing the interest of everyone else. To recap, the topics I have covered are as follows:
- Vitamin E is an important component in maintaining the good health of your residents. The antioxidant properties and other chemical interactions are just too important to take for granted.
- As caregivers who control the menu, you are in a good position to plan diets that are rich in naturally occurring alpha-tocopherol. Even with good menu planning, supplementation may be required.
- Taking a vitamin E supplement is not the end to caregiver concerns. Monitoring the resident may be required if there are underlying conditions that warrant closer observations.
- With so many vitamin E products making medical claims, caregivers should concern themselves only with those whose claims are backed up by hard clinical evidence.
As always, good luck with your caregiving.
Mark Parkinson, BS Pharm.
References
Jane Higdon, Ph.D. Victoria J. Drake, Ph.D. Vitamin E. Oregon State University, Linus Pauling Institute. Micronutrient Information Center. Nov 2008
https://lpi.oregonstate.edu/mic/vitamins/vitamin-E
Vitamin E, Fact Sheet for Health Professionals. National Institute of Health, Office of Dietary Supplements. 2020 https://ods.od.nih.gov/factsheets/VitaminE-HealthProfessional/
Vitamin E. MayoClinic.org. 2020 https://www.mayoclinic.org/drugs-supplements-vitamin-e/art-20364144
Zawn Villines. Ten benefits of vitamin E oil. MedicalNewsToday.com. Jan 29, 2020 https://www.medicalnewstoday.com/articles/318168#Risks-and-considerations
Exam Portal
click on [Take Exam]
Purchase membership here to unlock Exam Portal.
|
|
|
|
|
*Important*
Registration and login is required to place your name on your CE Certificates and access your certificate history.
Username MUST be how you want your name on your CE Certificate.