What’s the Big Deal with Naloxone
What’s the Big Deal with Naloxone
(Opioid overdose kits)
Author: Mark Parkinson BsPharm: President AFC-CE
Credit Hours 1 - Approximate time required: 60 min.
Educational Goal
Instruct Adult Foster Care Providers on how to use the drug Naloxone for opiate overdose.
Educational Objectives
- Tell why caregivers should care about Opioid Overdose.
- Tell readers what Naloxone is.
- Instruct how to use Naloxone for opioid overdose.
- Provide additional information relevant to AFC providers about Naloxone.
Procedure:
Read the course materials. 2. Click on exam portal [Take Exam]. 3. If you have not done so yet fill in Register form (username must be the name you want on your CE certificate). 4. Log in 5. Take exam. 6. Click on [Show Results] when done and follow the instructions that appear. 7. A score of 70% or better is considered passing and a Certificate of Completion will be generated for your records.
Disclaimer
The information presented in this activity is not meant to serve as a guideline for patient management. All procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this article should not be used by care providers without evaluation of their patients’ Doctor. Some conditions and possible contraindications may be of concern. All applicable manufacturers’ product information should be reviewed before use. The author and publisher of this continuing education program have made all reasonable efforts to ensure that all information contained herein is accurate in accordance with the latest available scientific knowledge at the time of acceptance for publication. Nutritional products discussed are not intended for the diagnosis, treatment, cure, or prevention of any disease.
This CE comes at the request of an AMH provider. (Yes, I do take requests.)
Opioid drugs are very beneficial in controlling major pain symptoms resulting from injury and disease. When administered under trained medical professionals' supervision, a lot of suffering can be alleviated. BUT there are some issues…… (Darn it all, why does there always have to be a But involved). Everyone’s got one and they’re often stinky. Pardon the pun, I couldn’t resist.
Opioids are very powerful. Take too much at one time and you’ll stop breathing. Take too much over a long period of time and you will become dependent on them to feel normal. Take them to feel euphoria instead of for pain and you will become addicted. Darn it all….again. Why does the human animal always mess things up trying to seek pleasure? It seems to be a weakness we have. And you know that there will always be some bad guy willing to take advantage of that weakness to make a buck.
You might be thinking, “Yeah, I’ve heard of people overdosing on Opioids and dying. What’s that got to do with me? I’m a professional. I take good care of my residents, and I always follow the doctor’s orders. There will be no opioid overdoses in my home. So why should I care.” A perfectly reasonable thought…… But, (there’s always a but)
- Accidents happen. You can get distracted and hand the pain meds to the wrong person. The wrong person grabs the pain meds while your back is turned. The curious, mentally disabled, resident takes the meds of another.
- There always seems to be a bad apple in the barrel. A co-worker or employee may not be as trustworthy as you are.
- You are part of the larger professional health community. As part of the team, it falls on all of us to battle this epidemic that is causing so much harm.
All of these things have happened to me, as an In-home caregiver and as a pharmacist. So- yeah, you should care.
What’s that I hear? A grumbling “ok ok- I admit, I should care. Ya’ happy now….BUT….(snicker,) What can I do about it? ” One word, Naloxone.
What is Naloxone?
That was a pretty good video….But, it misses some important points. Let me fill in the missing parts.
- Naloxone has been shown to be safe and effective for over 50 years. It is so safe and effective that the federal government has made naloxone available over-the-counter at most pharmacies. Naloxone can be obtained without a prescription in 43 states, including Oregon.
- The cost of OTC nasal spray is from 20 to 40 dollars and is available for purchase online. Some insurances may pay for OTC naloxone. You never know until you try. For example, use the Payflex card from Aetna Insurance at the cash register.
- Naloxone can be used to determine how addicted someone is to opioids. It also can be used to reduce itching in some cancer therapies and chronic kidney disease.
- Injectable versions act faster, I.V. versions in as little as 1 minute. The nasal spray is the easiest to use.
- Approximately 25% to 40% of naloxone is eliminated as metabolites in urine within 6 hours post-administration, with up to 70% excreted within 72 hours. Patients with kidney problems slow down these excretion times.
- Naloxone is used to get the overdosed victim breathing again. For those who are addicted to opioids, it can also trigger withdrawal symptoms. That could include severe headache, grouchiness, anxiety, vomiting, diarrhea, upset stomach, muscle pain, runny nose, and suicide ideation.
Suggestion for Adult Foster Care Use
 In Foster Care Homes Naloxone would be used as a first aid response, so you would be covered by the first aid Good Sam laws. But….. (you’re probably getting tired of that joke). AFC homes have some guidelines for over-the-counter drugs that you must follow. To avoid all the hassles, I suggest the following.
In Foster Care Homes Naloxone would be used as a first aid response, so you would be covered by the first aid Good Sam laws. But….. (you’re probably getting tired of that joke). AFC homes have some guidelines for over-the-counter drugs that you must follow. To avoid all the hassles, I suggest the following.
- Even though it is OTC, it would still be wise for Adult Foster Care providers to get a prescription for naloxone use from the primary care physician. I recommend having it as a standing PRN Doctor’s order, especially for Mental Health Homes and for all patients with a diagnosed substance use disorder.
- If you intend to keep an emergency supply for first aid purposes it would be wise to get your county officials’ guidelines for its use in your home. Get approval from the county in writing to have it in your first aid kit before you buy it.
- Internasal versions are easiest for AFC homes. Injectables require a nursing delegation and a sharps container.
- Have naloxone administration training for each care staff member and document training completion.
- Have a policy of always calling 911 when naloxone is used.
- You have my permission to copy any part of this course to use in your training material.
How to use Naloxone
 I cannot do better than the Oregon State Public Health Divisions: Naloxone Training Protocol so I am including it in this course. For an original copy go to https://www.oregon.gov/oha/PH/PROVIDERPARTNERRESOURCES/EMSTRAUMASYSTEMS/Documents/naloxone-training-protocol.pdf
I cannot do better than the Oregon State Public Health Divisions: Naloxone Training Protocol so I am including it in this course. For an original copy go to https://www.oregon.gov/oha/PH/PROVIDERPARTNERRESOURCES/EMSTRAUMASYSTEMS/Documents/naloxone-training-protocol.pdf
It comes complete with training completion documentation.
Quote
Opiate Overdose Treatment: Naloxone Training Protocol
1. Signs and symptoms of opiate overdose
The signs and symptoms of opiate overdose include:
-
- Unresponsiveness to yelling or stimulation, like rubbing your knuckles up and down the person’s sternum, or breastbone (also called a sternum rub) [This symptom effectively draws the line between overdosing and being really high but not overdosing.]
- Slow, shallow, or no breathing
- Pulse (heartbeat) is slow, erratic, or not there at all
- Turning pale, blue or gray (especially lips and fingernails)
- Snoring/gurgling/choking sounds
- Body very limp
- Vomiting
2. Opiate overdose treatment overview
-
- Check for a response.
- Call 911.
- Start chest compressions.
- Administer naloxone.
- Resume chest compressions with rescue breathing if the person has not yet started breathing.
- Conduct follow-up – administer a second dose of naloxone if no response after 3 minutes and resume chest compressions with rescue breathing.
- If naloxone is administered, provide details to emergency medical services
3. Responding to an opiate overdose
-
- Check for responsiveness.
 Yell.
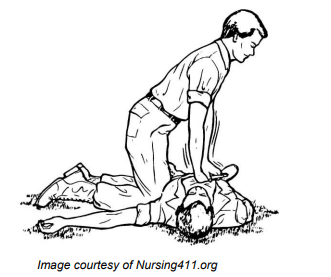
Yell.- Give a sternum rub. Make a fist and rake your knuckles hard up and down the front of the person’s sternum (breastbone). This is sometimes enough to wake the person up.
- Check for breathing. See if the person’s chest rises and falls and put your ear near the person’s face to listen and feel for breaths.
- If the person does not respond or is not breathing, proceed with the steps listed below.
- Call 911. If you have to leave the person, put the person in the recovery position.*
- State that someone is unconscious due to suspected overdose and indicate if the person is not breathing. (If you call police or 911 to get help for someone having a drug overdose, Oregon’s Good Samaritan Law protects you from being arrested or prosecuted for drug-related charges or probation or parole violations based on information provided to emergency responders.)
- Give the address and location.
- Be aware that complications may arise in overdose cases. Naloxone only works on opiates, and the person may have overdosed on something else, e.g., alcohol or benzodiazepines. Emergency medical services are critical.
- Check for responsiveness.
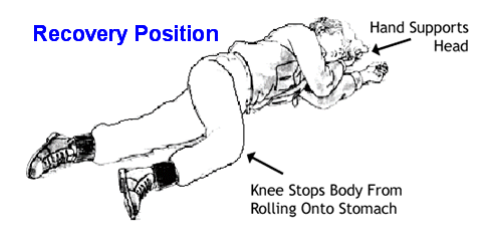
*Recovery position:
-
-
-
-
-
-
-
- Roll the person over slightly on the person’s side.
- Bend the top knee.
- Put the person’s top hand under the person’s head to support it.
- This position should keep the person from rolling onto his/her stomach or back, so the person does not choke if he/she vomits.
-
-
-
-
-
-
-
- (A) Start chest compressions with rescue breathing (CPR).
- Place heel of one hand over center of person’s chest.
- Place other hand on top of first hand, keeping elbows straight with shoulders directly above hands.
- Use body weight to push straight down, at least 2 inches, at rate of 100 compressions per minute.
- Give 2 breaths for every 30 compressions.
- CPR should be performed for 5 rounds (2 breaths for every 30 compressions), or for approximately 2 minutes, before reassessing.
- (A) Start chest compressions with rescue breathing (CPR).
OR
(B) If overdose is witnessed, i.e., you see the person stop breathing, or you are sure it is overdose due to personal knowledge of the person or situation, you have the option to start rescue breathing. Be aware when you call 911 that they may instruct you to perform CPR as well.
-
-
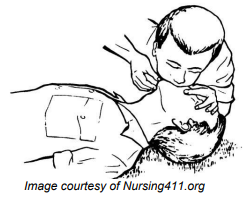
- Check the person’s airway for obstructions and remove any obstructions that can be seen
- Tilt the person’s forehead back and lift chin – see diagram below.
- Pinch the person’s nose and give normal breaths – not quick and not overly powerful breaths.
- Give one breath every five seconds.
- Continue rescue breathing for approximately 30 seconds.
-
4. Administer naloxone.
If the patient has been receiving opioids, giving them naloxone may result in temporary withdrawal symptoms. This response can include abrupt waking up, vomiting, diarrhea, sweating, and agitated behavior. While these symptoms can be dramatic and unpleasant, they are not life threatening and will only last until the naloxone has worn off. See details about specific naloxone products below.
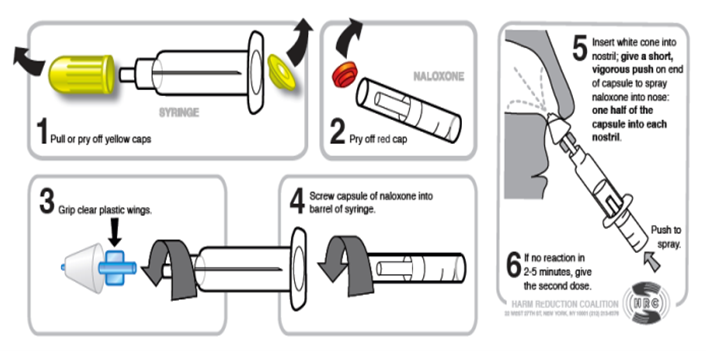
a) If your naloxone kit is a syringe set up to be given as a nasal (nose) spray:
-
-
-
- Pull or pry off both top and bottom covers on the syringe.
- Pry off the cap of the naloxone capsule.
- Grip the clear plastic wings.
- Screw the naloxone cartridge into the barrel of syringe.
- Insert white cone into nostril; give a short vigorous push on the end of the naloxone cartridge to spray naloxone into the nose: one half of the cartridge goes into each nostril.
- If minimal or no response in 3 minutes, then give a second dose.
-
-
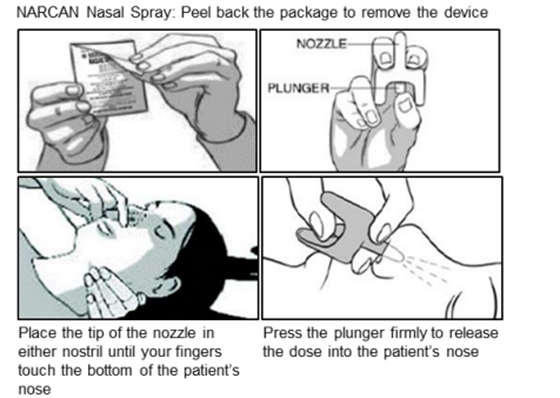
b) If your naloxone kit is NARCAN® Nasal Spray:
-
-
-
- Peel back the package to remove the device
- Hold the nozzle between two fingers as shown in image below.
- Place the tip of the nozzle in either nostril until your fingers touch the bottom of the patient’s nose.
- Press the plunger firmly with thumb to release the dose into the patient’s nose.
- If minimal or no response in 3 minutes, then give a second dose.
-
-
c) If your naloxone kit is a syringe set up to be given as an injection into a muscle (intramuscular):
-
-
-
- Remove cap of the naloxone vial.
- Draw up 1mL of naloxone into a syringe. (Ideally, the needle size for an injection into the muscle is 1 to 1.5-inches long and 25-gauge width)
- If available, clean the area with an alcohol wipe before you inject.
- Inject into muscle in the upper arm, thigh, or buttocks.
- Insert the needle at a 90-degree angle to the skin and push in plunger.
- If minimal or no response in 3 minutes, then give a second dose.
-
-
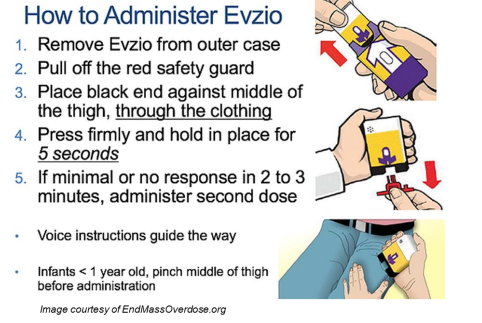
d) If your Naloxone kit is an Evzio® Injectable Device:
5. Resume chest compressions with rescue breathing (or chest compressions only) if the person has not yet started breathing. Brain damage can occur after 3-5 minutes without oxygen. The naloxone may not kick in that quickly. You may have to perform CPR for the person until the naloxone takes effect or until emergency medical services arrive.
6.Conduct follow-up.
-
-
- Naloxone takes several minutes to kick in and wears off in 30-45 minutes. The person may go back into overdose after the naloxone wears off.
- It is recommended that you watch the person for at least an hour or until emergency medical services arrive, in case the person goes back into overdose.
- You may need to give the person more naloxone. Give a second dose if the person does not respond after 3 minutes.
- If an overdose victim revives, keep the person calm. Tell the person that drugs are still in his/her system and that the naloxone wears off in 30-45 minutes. (Recommend that the person seek medical attention and assist him/her if necessary.)
- Do not let the person use more opiates. The naloxone will block them and the person could overdose again after the naloxone wears off.
-
End Quote
Again pretty good training …….But, (you knew I was going to write but again didn't yah)
Let me fill in some important details for AFC homes
- Because naloxone wears off before the drugs do, you have to monitor the patient for 6-12 hours after the first naloxone dose.
- If you have to repeat the nasal spray use alternating nostrils.
- How many doses of naloxone to be stored in your first aid kit depends how long it takes for 911 responders to get to you (more for very rural areas) and what illnesses your residents have. (more for substance use disorders).
- Tell 911 that you have given naloxone.
- Some nasal spray packages contain 2 doses.
- Store at room temperature with your other medications.
- Don’t forget to include the naloxone prescription on your MARS.
- If you use it, chart it on the PRN log and record the event in the resident’s file.
For visual learners here is a video on nasal spray naloxone administration.
Conclusion
Hopefully you will never have to use this information, and never have hear another “but” joke…. But…. If you do have to save a life from an opioid overdose, then you got the basics down. If you do forget the details, you know you can always come back to this lesson to get the why fors, the how to use, and what AFC providers have to do on top of everything else.
As always, good luck in your caregiving efforts.
Mark Parkinson BsPharm
References:
- Matthew R. Jordan; et al. Naloxone Stat Pearls. National Library of Medicine. May 5, 2024. https://www.ncbi.nlm.nih.gov/books/NBK441910/
- How Naloxone Saves Lives in Opioid Overdose. National Library of Medicine. Jan 15, 2019. https://www.youtube.com/watch?v=cssRZEI9ujY
- Tapering off opioids: When and how. Mayo Clinic.org. Nov. 23, 2023 https://www.mayoclinic.org/diseases-conditions/prescription-drug-abuse/in-depth/tapering-off-opioids-when-and-how/art-20386036#:~:text=Symptoms%20of%20opioid%20withdrawal%20may,such%20as%20sadness%20and%20depression.
- Opiate Overdose Treatment: Naloxone Training Protocol. Oregon State Public Health Division EMS & Trauma Systems. Oct 6, 2017 https://www.oregon.gov/oha/PH/PROVIDERPARTNERRESOURCES/EMSTRAUMASYSTEMS/Documents/naloxone-training-protocol.pdf
- NARCAN Nasal Spray - How to use. canaPHEM, Nov 9, 2018 https://www.youtube.com/watch?v=WnjgrRNMfKM
Exam Portal
click on [Take Exam]
Purchase membership here to unlock Exam Portal.
|
|
|
|
|
*Important*
Registration and login is required to place your name on your CE Certificates and access your certificate history.
Username MUST be how you want your name on your CE Certificate.
| Guest: Purchase Exam |