Concerned About Cancer?
Concerned About Cancer?
Author: Mark Parkinson BSPharm: President AFC-CE
Credit Hours 4- Approximate time required: 240 min.
Educational Goal:
To educate Adult Foster Care providers about cancer.
Educational Objectives:
Define the word cancer.
Describe how cancer is named, typed, graded, staged and classified.
List the known contributors to the development of cancer
Teach about the role of the caregiver in cancer
Define prognosis and survivorship in regard to cancer
Tell about the Grief and Coping Process
Define common cancer terms
Procedure:
Read the course materials. 2. Click on exam portal [Take Exam]. 3. If you have not done so yet fill in Register form (username must be the name you want on your CE certificate). 4. Log in 5. Take exam. 6. Click on [Show Results] when done and follow the instructions that appear. 7. A score of 70% or better is considered passing and a Certificate of Completion will be generated for your records.
Disclaimer
The information presented in this activity is not meant to serve as a guideline for patient management. All procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this article should not be used by care providers without evaluation of their patients’ Doctor. Some conditions and possible contraindications may be of concern. All applicable manufacturers’ product information should be reviewed before use. The author and publisher of this continuing education program have made all reasonable efforts to ensure that all information contained herein is accurate in accordance with the latest available scientific knowledge at the time of acceptance for publication. Nutritional products discussed are not intended for the diagnosis, treatment, cure, or prevention of any disease.
Concerned About Cancer?
There are very few words that evoke more fear than the word Cancer. According to the National Cancer Institute, “Cancer is among the leading causes of death worldwide. In 2012, there were 14.1 million new cases and 8.2 million cancer-related deaths worldwide. In 2018, an estimated 1,735,350 new cases of cancer will be diagnosed in the United States and 609,640 people will die from the disease. The number of new cases of cancer (cancer incidence) is 439.2 per 100,000 men and women per year. Approximately 38.4% of men and women will be diagnosed with cancer at some point during their lifetimes (based on 2011–2015 cases). It is estimated that the national expenditures for cancer care in the United States in 2017 was $147.3 billion dollars.” Source https://www.cancer.gov/about-cancer/understanding/statistics
Cancer in the mainstream media is always portrayed as a tragedy. Invariably the story that is told is that those with cancer will be victims. They will have a long, slow, painful struggle with the disease, followed eventually by death. The stories about cancer treatments are also full of suffering, where even the caregiver experiences bitter emotions. It is no wonder that we avoid even the thought of the word cancer. How much of that story is true and how much are just fiction? What is cancer? Is it one disease or a collection of diseases? Do you catch it or are you born with it? What are the signs and symptoms? How is it diagnosed? How is it treated? What is actually involved in taking care of those with cancer?
be victims. They will have a long, slow, painful struggle with the disease, followed eventually by death. The stories about cancer treatments are also full of suffering, where even the caregiver experiences bitter emotions. It is no wonder that we avoid even the thought of the word cancer. How much of that story is true and how much are just fiction? What is cancer? Is it one disease or a collection of diseases? Do you catch it or are you born with it? What are the signs and symptoms? How is it diagnosed? How is it treated? What is actually involved in taking care of those with cancer?
Definition
The National Cancer Institute at the National Institutes of Health defines cancer as:
“A term for diseases in which abnormal cells divide without control and can invade nearby tissues. Cancer cells can also spread to other parts of the body through the blood and lymph systems.”
Basically, cancer is a disease of abnormal cell growth and it can happen to any cell in the body. The transformation of a normal cell into a cancer cell is called carcinogenesis.
It all happens in the genes of the cell’s DNA. Genes are small subsections of the DNA. They are responsible for the different functioning of the cell. As the genes go about their business, errors can occur. Those errors are called mutations. The mutations can be caused by external events like toxic chemicals (we call them carcinogens), radiation, or naturally-occurring random events. Some forms of genes are more susceptible to changes than others. Those who inherit these forms of genes are predisposed to developing cancer.
As gene errors accumulate in the DNA, the cell starts to function abnormally. Ordinarily the body can sense and control the abnormalities by killing the cell or programming the cell to die on its own. Sometimes that doesn’t happen and the abnormal cell starts to grow and divide, forming a mass of irregular cells called a tumor. If the tumor stays together in a mass, we call it a benign tumor. If the tumor grows out of control and pieces of the tumor break off, travel to other sites, and start to grow, we call it a malignant tumor. The process of spreading through the body is called metastasis. When malignancies occur, we call that cancer, though not all cancer forms tumors.
Name, Type, Grade and Stage
Any cell of our body has the potential to become malignant. This leads to a confusing amount of diseases we could call cancer. According to the National Cancer Institute at the National Institutes of Health there are over 100 types of cancer. The Cancer Research Institute states that there are over 200 varieties. To help make sense of the mind-boggling number of variables in the disease, modern medicine classifies and categorizes each occurrence.
Name
Commonly the cancer is named from where the cancer first originated. For example: breast cancer, skin cancer, etc. We still call it breast cancer even if it spreads to the bones or other places in the body. That leads to a lot of confusion, so modern medicine classifies and categories cancer disease names more definitively.
Medical terminology builds up cancer names using different aspects of what they are trying to name, thus describing the condition as well as giving it a name. In cancer names the beginning of the word references where the disease originated. The ending of the term refers to the classification or type of cancer cell that has occurred.
Prefix examples:
|
Organ or tissue of origin
|
hepatocarcinoma (liver) lipocarcinoma (fat) |
|
Size and shape of the cells
|
giant cell carcinoma spindle cell carcinoma small-cell carcinoma |
|
Type of cell in an organ
|
ductal carcinoma of the breast Merkel cell carcinoma |
Suffix example:
|
Carcinoma |
Cancers derived from epithelial cells. This group includes many of the most common cancers and includes nearly all those in the breast, prostate, lung, pancreas, and colon. |
|
Sarcoma |
Cancers arising from connective tissue (e.g. bone, cartilage, fat, nerve), each of which develops from cells originating in mesenchymal cells outside the bone marrow. |
|
Lymphoma Leukemia |
These two classes arise from hematopoietic (blood-forming) cells that leave the marrow and tend to mature in the lymph nodes and blood, respectively. |
|
Germ cell tumor |
Cancers derived from pluripotent cells, most often presenting in the testicle or the ovary (seminoma and dysgerminoma, respectively). |
|
Blastoma |
Cancers derived from immature "precursor" cells or embryonic tissue. |
Source https://en.wikipedia.org/wiki/Cancer
I have always appreciated the way medical terminology puts so much information into a single term. It may lead to great big complicated words, but if you look up the various parts of the word you can tell what is going on just by the name.
Let’s break apart a scary, big cancer name.
Neuroblastoma: neuro – nerves, blastoma – cancer of precursor cells
Or a type of cancer that forms in immature nerve tissue.
A cautionary word about tumor names
The suffix -oma means tumor, but not all tumors are cancerous; some are benign. If you see -oma ending a word, do your research before jumping to any conclusions. The suffix -noma does mean cancer.
Type Classification
Cancers are broadly grouped as solid (tumor mass) or liquid (blood cell cancers. They are further classified by where the cancer started.
Cancer Classifications:
|
1. Carcinomas are cancers that occur in epithelial (surface) tissues in the body. 2. Sarcomas occur in connective tissue. For example: bone, cartilage, fat, blood vessels, and muscles. 3. Myelomas are cancers that occur in plasma cells in the bone marrow. 4. Leukemias are a group of different blood cancers of the bone marrow. 5. Lymphomas are cancers of the immune system cells. 6. Mixed cancers arise from more than one type of tissue. |
Source https://www.medicinenet.com/cancer_101_pictures_slideshow/article.htm
Grade
Tumor grade is the description of a tumor based on how abnormal the tumor cells and the tumor tissue look under a microscope. It gives important clues on the potential of a tumor to grow or turn cancerous and spread. It ranges from almost-normal-looking cells (well differentiated) to abnormal cells that lack normal cell structures (poorly differentiated or undifferentiated). There are several different grading systems. It all depends on the type of cancer being described. In general, it is a simple number.
Cancer Grades:
|
GX |
Grade cannot be assessed (undetermined grade) |
|
G1 |
Well differentiated (low grade) |
|
G2 |
Moderately differentiated (intermediate grade) |
|
G3 |
Poorly differentiated (high grade) |
|
G4 |
Undifferentiated (high grade) |
Source https://www.cancer.gov/about-cancer/diagnosis-staging/prognosis/tumor-grade-fact-sheet
Breast cancer and prostate cancer have a grading system that is a bit more complicated, but the general rule of thumb is the higher the grade, the greater potential for bad news.
Stage
The stage of a cancer is determined generally by how far the cancer has spread. The stage is often used by doctors in their diagnosis of the disease.
Cancer Stages:
|
Stage O |
This stage describes cancer in situ, which means “in place.” Stage 0 cancers are still located in the place they started and have not spread to nearby tissues. This stage of cancer is often highly curable, usually by removing the entire tumor with surgery. |
|
Stage I |
This stage is usually a small cancer or tumor that has not grown deeply into nearby tissues. It also has not spread to the lymph nodes or other parts of the body. It is often called early-stage cancer. |
|
Stage II Stage III |
In general, these two stages indicate larger cancers or tumors that have grown more deeply into nearby tissue. They may have also spread to lymph nodes but not to other parts of the body. |
|
Stage IV |
This stage means that the cancer has spread to other organs or parts of the body. It may also be called advanced or metastatic cancer. |
Source; https://www.cancer.net/navigating-cancer-care/diagnosing-cancer/stages-cancer
Causes of Cancer
Because of people’s strong reaction towards cancer, any story about it is big news. News outlets know that the word “cancer” 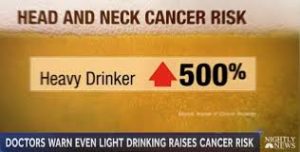 sells. In my opinion, the consequence of this sensational news coverage is that it seems like just about everything causes cancer. Of course, that is not true. A lot of things have to line up in order to make it past the body’s cancer defenses. In fact, it’s pretty hard to point to any one thing and say, “That is the thing that caused your cancer.” It would be more accurate to say that thing or those things contributed to the development of your cancer. Generally speaking, 90–95 percent of cancer cases are most likely caused by outside factors. That leaves the remaining 5–10 percent as being due to inherited genetic weakness in the DNA or in the anti-cancer defenses.
sells. In my opinion, the consequence of this sensational news coverage is that it seems like just about everything causes cancer. Of course, that is not true. A lot of things have to line up in order to make it past the body’s cancer defenses. In fact, it’s pretty hard to point to any one thing and say, “That is the thing that caused your cancer.” It would be more accurate to say that thing or those things contributed to the development of your cancer. Generally speaking, 90–95 percent of cancer cases are most likely caused by outside factors. That leaves the remaining 5–10 percent as being due to inherited genetic weakness in the DNA or in the anti-cancer defenses.
Known Contributors to the Development of Cancer
As you recall from earlier in this article, cancer is a result of abnormal genes that cause the DNA to not function normally. Plus, the abnormal cell is not killed off by the defenses but instead grows out of control. I would also like to point out that you cannot “catch” cancer from someone who has it, except in the very rare cases of pregnancy or cancer-containing tissue donation and blood transfusion. Here is a general list of known contributors to the development of cancer.
- Chemicals – Certain chemicals called carcinogens interfere with the molecular functioning of cells and their DNA. Tobacco smoke contains over 50 carcinogens and causes 90 percent of lung cancers. Other famous carcinogens are benzene and alcohol. Exposure to carcinogens does not guarantee a development of cancer, but greater exposure increases the chances significantly.
- Diet, inactivity, obesity – Up to 35 percent of cancers have a dietary component. Eating large amounts of certain foods, lack of physical exercise, and especially obesity leads to a general decline of health and a weakening of our immune and endocrine (hormone) systems. The chemicals in the foods we eat may also be factors in cancer. For example, a high-salt diet has been linked to cancer.
- Infection – Viruses, bacteria, and a few parasites interfere with a cell’s functioning, which may lead to cancer. Virus infections that lead to carcinomas are classified as oncoviruses.
- Radiation – High-dose or long-exposure-time radiation disrupts the atoms in our cells. Disorder enough of the wrong atoms and you get cancer. Radiation sources include radioactive material, ultraviolet light from the sun, and possibly high-voltage power lines.
- Cell-damaging agents – Physically damaging a cell over and over again can lead to errors in the repair process that can lead to cancer. Two examples of this are mesothelioma, caused by asbestos, and esophageal cancer, caused by stomach acid in the throat (GERD).
- Autoimmune disease – Diseases like celiac disease, Crohn’s disease and ulcerative colitis also make a cell repair itself over and over again. The extra repair and the repeated inflammatory process increase the chance of malignancies.
- Hormones – Hormones that play a role in cell proliferation do not cause cancer but can make it grow faster. Think of it like stepping on the gas of the cancer engine. Estrogen and breast cancer and testosterone and testicular cancer are two examples.
- Defects – Congenital (inherited) defects in any of the cell repair genes or the anti-cancer cell mechanisms can predispose an individual to developing cancer. Those whose parents died of breast cancer are at greater risk themselves.
The Role of the Caregiver in Cancer
I know that some of you are thinking, “This is all very interesting, but what has it got to do with me? I’m no doctor. What has all this cancer stuff got to do with my job? I don’t have anything to do with cancer.” In-home caregivers have a greater role in cancer than what you might think. In my opinion Adult Foster Care providers have the most prominent role in preventing cancer, are in the best position for early detection of cancer, and they play a major role in patient compliance with treatment. In addition, they are probably the most influential on the day-to-day perceptions and attitudes of the patient. All of the above are key components in the detection and treatment of cancer. It is my hope that this article helps prepare you for your important roles in this disease. Let’s take a look at some of the tools at your disposal.
Perspectives and Cancer
 The society that we live in has made cancer a very serious subject. The news we read and the stories we hear affects our perceptions and perspectives. Negative doom-and-gloom perspectives increase the impact of the disease on both caregiver and patient. Gaining a proper perspective, one that is defined by knowledge and not by fear, increases the effectiveness of care and treatment and results in more positive outcomes.
The society that we live in has made cancer a very serious subject. The news we read and the stories we hear affects our perceptions and perspectives. Negative doom-and-gloom perspectives increase the impact of the disease on both caregiver and patient. Gaining a proper perspective, one that is defined by knowledge and not by fear, increases the effectiveness of care and treatment and results in more positive outcomes.
The truth is, not all cancer cases involve long, drawn-out, difficult treatments and lead to death. The most common form of cancer, non-melanoma skin cancer, accounts for about one-third of cancer cases worldwide and rarely ends in death. There are many cancer cases treated by a simple surgery to remove the tumor. Even in cases that are more serious, advances in cancer care have greatly improved treatment results. Regardless of the seriousness of the cancer it is important to remember: 1. positive perspectives increase positive outcomes, 2. the earlier a cancer is diagnosed and treated, the better, and 3. there is always something that can be done for cancer victims, even if it is just making them feel more comfortable.
Prevention and Cancer
Of course, the most effective treatment for cancer is preventing it from happening in the first place. Since 70–90 percent of cancers are caused by environmental factors, the lifestyle choices we make are the most important factors in preventing cancer. Adult Foster Care providers are in a position to help maintain healthy lifestyle choices more so than any other medical provider. In my opinion, that gives In Home caregivers the most prominent role in the prevention of cancer. 
For the In-Home caregiver, it all comes down to managing the risk factors that lead to the potential of cancer. I am not recommending stressing about every little thing. With all the fake news and pseudo-science about cancer we are bombarded with every day, that would be an impossible effort. What is doable is concentrating on the major risk factors of tobacco, obesity, alcohol use, poor diet, ultraviolet radiation (sunshine), physical inactivity and pollutants. In general, what that means is establish good caregiver business practices. Run your home right and the cancer risks take care of themselves. Keeping your residents healthy is all that is required.
There are a couple of additional things that you could do to manage the risk of cancer.
- For mental health homes, caregivers must understand the role of nicotine and alcohol use in therapy. Their residents use these cancer-causing agents as a self-treatment. By replacing them with more effective therapy you reduce the need, making it easier to control their use.
- There are vaccinations that can control the infections that can cause cancer. They are the human papillomavirus vaccine to prevent cervical cancer in females, and the hepatitis B vaccine to prevent liver cancer. Not everyone needs to be vaccinated, just those at risk. For hepatitis B that would be children and adolescents younger than 19 years of age and adults who are at risk for hepatitis B virus infection. For human papillomavirus vaccine it is recommended for girls aged 11 or 12 and boys before the age of 26. Human papillomavirus is spread by sexual contact. If there is no chance of that occurring, there may not be a need for vaccination. Consult with a physician on a case-by-case basis.
- You can check your home for radiation sources. It has been reported that approximately one out of every 15 houses in the U.S. may have elevated levels of radon, a naturally occurring radioactive gas.
- Check on family history of cancer. This will help identify hereditary risk factors. You would think that the primary care physician would cover this. But as you already know, not everyone fills out the doctor’s paperwork completely. Also, there are those who go doctor-hopping. The more switching of doctors, the more likely things will get missed. You have time to be thorough while doctors do not.
- Ultra-violet radiation is usually not a problem for care homes. Your problem is just the opposite; it’s hard to get them out into the sunshine. If you are concerned, using a simple sunscreen and wearing a hat are sufficient enough precautions.
- If you’re worried about carcinogenic chemicals in the foods you serve, the rule of thumb is to cook from scratch. Also, avoid barbequed and pickled foods and foods with high salt content. It may be an effort to cook from raw ingredients, but there are other benefits that make it worth your while. It’s easier on the budget, it usually tastes better, and it’s good for marketing. (Potential customers love hearing about home-cooked meals made from scratch.)

Detecting Cancer
Detecting cancer when it starts is almost impossible. It starts too small, can happen anywhere in the body, and its signs and symptoms are non-existent. As it grows it is still very hard to spot because of all the variable ways the disease can present itself. Cancer has been called the great imitator because symptoms often look like another disease’s processes. Even doctors have a difficult time diagnosing cancer. They usually have to take a sample and send it off to a lab for verification. The process is called taking a biopsy. Detection usually is a matter of doctors recognizing the possibility of cancer by the patterns of abnormalities they see in the signs and symptoms. The sooner they recognize the possibility, the more promising the outcome. That is where the In-Home caregiver comes into play.
The Adult Foster Care provider can be the eyes and ears of the doctor. If you’re observant you will see the changes and abnormalities before any other medical professional. This early detection is key to successfully treating cancer. The earlier, the better is the rule of thumb.
Before you get all excited, you’re not diagnosing the patient, you’re just looking for the possibility that something is wrong with your resident. If you become aware of certain symptoms occurring, you can bring them to the attention of the doctor and follow up by asking the right questions.
The general signs and symptoms of cancer include:
- Unusual fatigue that is not helped by resting. Some blood changes like in leukemia or cancer-caused chronic bleeding can leave victims anemic and weak.
- Weight loss without trying. Almost half the people with cancer lose weight. This is often the first recognizable sign that shows up.
- Unexplained pain that is persistent and is hard to treat. That includes headaches that for lasts days.
- Skin changes that include new moles, lumps, and thickening or unusual marks. Look for unusual color changes like yellowing of the skin and red patches. Also look for itchiness and unexpected hair growth.
- Changes in bowel or bladder function, especially if there is bleeding involved. Blood in the stools makes them look tarry or like coffee grounds.
- Voice changes or a cough that is severe or lasts more than three weeks. Here again, if blood comes up that’s an automatic trip to the doctor.
- Fever is always a sign that the body is trying to fight something. If the fever doesn’t go away, then that’s a sign that the problem is not going away. Time to see the doctor.
- Sores that don’t heal, including sores in the mouth. Even a minor sore that doesn’t heal should be looked at.
- Continued indigestion, bloated feeling, or trouble swallowing.
- In men: changes in the testicles or penis. That includes pain, a lump, redness, or a change in size or shape. Watch for complaints about painful peeing.
- In women: breast changes. Look for lumps, sudden changes in size, discharge from the nipples, spots, or other changes in the skin around the nipples. Watch for bleeding between periods or bloating that isn’t linked to PMS.
If you take this list at face value you could think, “Most of those happen just about every week in my house. How will I ever be able to see cancer coming when those symptoms are so common?” It’s all about knowing your residents and seeing what’s not normal. You’re looking for the unexplained change from the regular routine. If you can say, “Well, that’s not right. I can’t figure out what’s causing that,” then you’d be justified in calling the doctor. Look for the unusual combination of symptoms or the  problem that will not go away or is difficult to fix. When deciding if you should bring up the “Is it cancer?” question with the doctor, remember what cancer is, how it is formed, and what it might look like. If all the signs fit the cancer profile, then you would be justified. If you have a few misidentifications, it’s no big deal. Learn from each time so you can add it to your experience at knowing what is normal and not normal. It’s always better to be safe than sorry, just don’t overdo it and wreck your reputation.
problem that will not go away or is difficult to fix. When deciding if you should bring up the “Is it cancer?” question with the doctor, remember what cancer is, how it is formed, and what it might look like. If all the signs fit the cancer profile, then you would be justified. If you have a few misidentifications, it’s no big deal. Learn from each time so you can add it to your experience at knowing what is normal and not normal. It’s always better to be safe than sorry, just don’t overdo it and wreck your reputation.
Screening for Cancer
Unfortunately, cancer can occur without symptoms. There are medical tests that can detect cancers even if there are no signs at all, but they can be expensive and time-consuming. Using these tests to screen for cancer becomes a balancing act between expense and benefit. The more risk factors there are, the more justified the screening tests become. Consult with the resident’s doctor about which tests should be given and when. If there are concerns, I recommend that you put a note in the resident’s file as a reminder to get the patient screened at the appropriate times.

In general, the United States Preventive Task Force (USPTF) and the Center for Disease Control recommends the following.
- Breast cancer: Women who are 50 to 74 years old and are at average risk for breast cancer get a mammogram every two years. A mammogram is an x-ray of the breast. A magnetic resonance image, (MRI) which uses radio waves and magnets, can also be used.
- Cervical cancer: Women between the ages of 21 and 65 should get a Pap test. The Pap test takes tissue samples and look for cancer cells. At age 30 it is recommended to take an HPV test. The HPV test looks for the virus human papillomavirus that can cause cancer. If these tests come up negative, it may be several years before another test is needed.
- Colorectal cancer: Everyone between the ages of 50–75 should get regular colorectal exams. Between the ages of 75–86 patients should consult with their doctor to see if there is a need for further exams. There are several tests that the doctor can perform, which include: stool tests every 1–3 years, flexible sigmoidoscopy every 5 or 10 years, colonoscopy every 10 years, and CT colonography (virtual colonoscopy) every 5 years.
- Lung cancer – For heavy smokers or former heavy smokers who have quit in the last 15 years it is recommended that a yearly screening with a low-dose computed tomography (LDCT) be taken.
- Screening for ovarian, pancreatic, prostate, testicular, and thyroid cancers has not been shown to reduce deaths from those cancers, so the USPTF recommends against screening tests. The American Cancer Society does state, “Starting at age 50, all men at average risk should talk with a healthcare provider about the uncertainties, risks, and potential benefits of testing so they can decide if they want to be tested.”

Prognosis for Those with Cancer
For those diagnosed with cancer, a thousand questions arise. How long do I have to live? How much am I going to suffer? What treatments should I get? They turn to the doctor for answers and the doctor gives them a prognosis. But a prognosis is not what you think it is.
According to Taber’s Cyclopedic Medical Dictionary, 16th edition, a prognosis is defined as a “Prediction of course and end of disease, and the estimate of the chance of recovery.” In other words, it’s the doctor’s best guess on how the disease will progress. But all things considered, it’s a pretty good guess because it is based on a mountain of statistics.
How a Prognosis Is Determined![]()
For years medical science has been collecting statistics on everything cancer-related including:
- The type of cancer and where it has occurred in the body.
- The stage of the cancer.
- The cancer’s grade. Grading provides important clues about the likelihood of how the cancer grows and spreads.
- Certain traits of the cancer cells.
- What the age and health of the cancer victims are and how it affects the progression of the disease.
- How patients respond to the various treatments.
The data has been sorted, labeled, categorized, and cataloged. Then, statisticians take over and try to boil all that data down to useable numbers. Doctors can use this information to make a pretty good prediction about how a particular type of cancer will progress. These predications can also help determine which treatment to choose. To help you get a better understanding of what a cancer prognosis is all about, let’s consider the following.
Estimating How Long a Cancer Victim Will Live. 
No one can tell how long a person who has cancer will live, but they can tell you the survival rate of others who have had that kind of cancer. It is usually expressed as a five-year survival rate. The five-year relative survival rate for women with cervical cancer is about 68 percent. This means that about 68 out of every 100 women with cervical cancer will be alive five years after diagnosis. Other examples are the five-year relative survival rate for early-stage cervical cancer, which is 92 percent. This means that 92 out of every 100 women with early-stage cervical cancer will be alive five years after diagnosis. For early-stage colorectal cancer, the five-year relative survival rate is 90 percent. For advanced-stage colorectal cancer that’s spread to distant parts of the body, the rate drops to about 13 percent.
Points for Caregivers to Remember About Cancer Prognosis
- A prognosis is a guess based on statistical averages of large groups of people. Individual reactions may vary from the norm.
- Survival rates are based on known variables. If the variables change, the original prediction will be wrong.
- A prognosis is actually very complex. If you or the resident is unsure what it means, ask the doctor for clarification.
- Five-year rates, by definition, are five years out of date. New therapies are being developed all the time.
The Concepts of Survival, Cure and Remission
Survival is an all-encompassing term that includes those who are cured, those in remission, those who have relapsed and those still in active treatment. It would be unwise to relate the term “survival” with being cured. When it comes to cancer, nothing is that simple. In cancer, “cure” means that there are no traces of your cancer after treatment. Remission means that the signs and symptoms of cancer are reduced. Remission can be partial or complete. Complete means no signs of the cancer remain. Relapse means the symptoms have returned.
With cancer there is always the chance that some cancerous cells are still there, undetected. There are also the underlying risk factors to consider. If nothing has changed, the chance for the cancer to return is still high. Even though the medical community considers many cancers “cured” if there are no symptoms after five years, it is still possible for the cancer to come back. In cancer it should always be remembered that survival means alive, not disease-free.
 The Final Words on Prognosis
The Final Words on Prognosis
Not everyone can handle bad news. A prognosis can just be too intimidating, frightening or impersonal for some of your residents. If the patient doesn’t want to know the prognosis, you have to respect that. But, as the patient’s advocate and frontline caregiver, you should know as much as you can. If there is an issue with the resident not wanting to know the prognosis, I recommend getting a copy of the prognosis for your files. The information is just too important and its impact on your caregiving too great for you to not have it. Use the prognosis with skill and tact to ease the patient into what must be done in the future.
Caregiving in Cancer
Cancer can happen anywhere in the body to any cell type. With that much variability, patient care in cancer becomes too broad a subject to cover in any one lesson in depth. There are, after all, entire books and college degrees dedicated to caring for cancer victims. If you are employed in a care home and have a resident with cancer, your caregiving duties will multiply in complexity and effort. In the beginning, almost nothing will change in your caregiving routine. But as the cancer progresses or the therapy gets more aggressive, no one caregiver can handle it all. You will become part of a team effort. The emphasis of your role will shift more towards being the patient’s advocate as well as the primary caregiver. Even with help, if the cancer progresses, there will be a point where cancer caregiving will be beyond what you can supply in an adult foster care home. So, my advice is, get a feel for the overall process, know where and how to get help, and know when to say, “That’s enough for me.” The rest of this article will be written with that in mind. If you want more detailed training on cancer care specifics, then get the book or take the course.

Cancer Treatments
The ultimate goal of all cancer treatments is either killing off the cancerous cells or physically removing them from the body. There are several options open to the doctor, which include surgery, medical lasers, radiation, chemotherapy, immunotherapy and alternative therapy. Often the therapies chosen will change over the course of treatment and end up being a combination of several of the following options.
- Surgery – Cutting out the cancer is the treatment of choice if the cancer is solid and isolated. In cancer’s early stages the doctor will try to remove the entire tumor during the diagnosis/biopsy procedure. If the cancer is too advanced or it’s impractical to remove it all, surgery still might be done to reduce the cancer’s mass, thus reducing the symptoms burden and increasing the comfort of the patient.
- Medical lasers – High-intensity light devices known as lasers are used to shrink or destroy cancerous and precancerous tumors. They are most effective on surface cancers even if that surface is on an internal organ within the body. Lasers are more precise than surgery and have fewer side effects, but it takes special training and equipment. Of course, this makes laser therapy harder to find and more expensive.
- Radiation – Ionizing radiation is used to reach into a cancer cell and disrupt the very atoms holding it together. If you disrupt enough of the atoms, especially its DNA, the cell will die. Unfortunately, what kills cancer cells will also harm healthy cells, including starting a secondary cancer. Radiation therapy must be very precise and specific.
- Chemotherapy – Known as chemo for short, this is a collection of powerful chemicals that are used to make cells die. Traditionally this was a nonspecific therapy used to target cells that divide rapidly. It was hoped that it would kill all of the rapidly multiplying cancer cells before significantly harming the rest of the body. Recently there has been the development of more directed therapy that targets unique cancer-related functions. For example, chemicals that just block the estrogen receptors in breast cells.
- Immunotherapy – The body has the ability to kill off cancer cells by itself. Immunotherapy is designed to support and enhance this ability. It is a relatively new science with new therapies in development, including stimulating the immune system and supplementing the immune system from outside sources.
- Alternative therapy – There is more than one system of treating patients. Alternative therapy includes therapies traditionally not used in Western-style medicine. Since these therapies typically are not extensively studied, their use is dependent on the experience of the practitioner. Alternative therapy means therapies that are used instead of conventional methods and this route is quite controversial. What is gaining in popularity is the use of these therapies as add-on treatments. This has been referred to as complementary therapy.
Cancer Management
The underlying goal of cancer management is managing the patient, not the disease. It involves how the cancer reacts to the treatments and how the patient reacts to the treatments and the cancer. It’s a blend of medical treatment, symptom relief, side-effect management, emotional support, financial considerations, caregiving, and the choices the patient and their family have to make along the way. Cancer management is a team effort. As the primary caregiver and patient advocate, the process of cancer management is something the adult foster care provider should be deeply involved in. It’s going to take the caregiver being assertive enough to be included on the team.
Patient’s Reaction
It all starts with the patient’s reaction to the cancer diagnosis. There is going to be an emotional roller coaster as the patient tries to cope with the consequences of cancer. The resident and their family have much to contemplate and many decisions to make. There will be many questions. Help the resident find the answers. Be patient, positive, and professional. Help find the resources that they will need, including the will to keep going when times get tough. Speaking of getting tough, there might be times when therapy side effects are difficult to handle. Every caregiving fiber of your body will want to back off the therapy. You think you are being kind but in cancer you are literally killing them with your kindness. Stick to the therapies and help the resident to cope.

Grief and Coping
Grief will be a major component in their initial reaction. To help with the grief I suggest the work of David Kessler and Elisabeth -Ross and Grief.com. They describe the five stages of grieving. I quote Mr. Kessler’s website.
- DENIAL – Denial is the first of the five stages of grief. It helps us to survive the loss. In this stage, the world becomes meaningless and overwhelming. Life makes no sense. We are in a state of shock and denial. We go numb. We wonder how we can go on, if we can go on, why we should go on. We try to find a way to simply get through each day. Denial and shock help us to cope and make survival possible. Denial helps us to pace our feelings of grief. There is a grace in denial. It is nature’s way of letting in only as much as we can handle. As you accept the reality of the loss and start to ask yourself questions, you are unknowingly beginning the healing process. You are becoming stronger, and the denial is beginning to fade. But as you proceed, all the feelings you were denying begin to surface.
- ANGER – Anger is a necessary stage of the healing process. Be willing to feel your anger, even though it may seem endless. The more you truly feel it, the more it will begin to dissipate and the more you will heal. There are many other emotions under the anger and you will get to them in time, but anger is the emotion we are most used to managing. The truth is that anger has no limits. It can extend not only to your friends, the doctors, your family, yourself and your loved one who died, but also to God. You may ask, “Where is God in this? Underneath anger is pain, your pain. It is natural to feel deserted and abandoned, but we live in a society that fears anger. Anger is strength and it can be an anchor, giving temporary structure to the nothingness of loss. At first grief feels like being lost at sea: no connection to anything. Then you get angry at someone, maybe a person who didn’t attend the funeral, maybe a person who isn’t around, maybe a person who is different now that your loved one has died. Suddenly you have a structure—your anger toward them. The anger becomes a bridge over the open sea, a connection from you to them. It is something to hold onto; and a connection made from the strength of anger feels better than nothing. We usually know more about suppressing anger than feeling it. The anger is just another indication of the intensity of your love.
- BARGAINING – Before a loss, it seems like you will do anything if only your loved one would be spared. “Please God,” you bargain, “I will never be angry at my wife again if you’ll just let her live.” After a loss, bargaining may take the form of a temporary truce. “What if I devote the rest of my life to helping others. Then can I wake up and realize this has all been a bad dream?” We become lost in a maze of “If only…” or “What if…” statements. We want life returned to what is was; we want our loved one restored. We want to go back in time: find the tumor sooner, recognize the illness more quickly, stop the accident from happening…if only, if only, if only. Guilt is often bargaining’s companion. The “if onlys” cause us to find fault in ourselves and what we “think” we could have done differently. We may even bargain with the pain. We will do anything not to feel the pain of this loss. We remain in the past, trying to negotiate our way out of the hurt. People often think of the stages as lasting weeks or months. They forget that the stages are responses to feelings that can last for minutes or hours as we flip in and out of one and then another. We do not enter and leave each individual stage in a linear fashion. We may feel one, then another and back again to the first one.
- DEPRESSION – After bargaining, our attention moves squarely into the present. Empty feelings present themselves, and grief enters our lives on a deeper level, deeper than we ever imagined. This depressive stage feels as though it will last forever. It’s important to understand that this depression is not a sign of mental illness. It is the appropriate response to a great loss. We withdraw from life, left in a fog of intense sadness, wondering, perhaps, if there is any point in going on alone? Why go on at all? Depression after a loss is too often seen as unnatural: a state to be fixed, something to snap out of. The first question to ask yourself is whether or not the situation you’re in is actually depressing. The loss of a loved one is a very depressing situation, and depression is a normal and appropriate response. To not experience depression after a loved one dies would be unusual. When a loss fully settles in your soul, the realization that your loved one didn’t get better this time and is not coming back is understandably depressing. If grief is a process of healing, then depression is one of the many necessary steps along the way.
- ACCEPTANCE – Acceptance is often confused with the notion of being “all right” or “OK” with what has happened. This is not the case. Most people don’t ever feel OK or all right about the loss of a loved one. This stage is about accepting the reality that our loved one is physically gone and recognizing that this new reality is the permanent reality. We will never like this reality or make it OK, but eventually we accept it. We learn to live with it. It is the new norm with which we must learn to live. We must try to live now in a world where our loved one is missing. In resisting this new norm, at first many people want to maintain life as it was before a loved one died. In time, through bits and pieces of acceptance, however, we see that we cannot maintain the past intact. It has been forever changed and we must readjust. We must learn to reorganize roles, re-assign them to others or take them on ourselves. Finding acceptance may be just having more good days than bad ones. As we begin to live again and enjoy our life, we often feel that in doing so, we are betraying our loved one. We can never replace what has been lost, but we can make new connections, new meaningful relationships, new inter-dependencies. Instead of denying our feelings, we listen to our needs; we move, we change, we grow, we evolve. We may start to reach out to others and become involved in their lives. We invest in our friendships and in our relationship with ourselves. We begin to live again, but we cannot do so until we have given grief its time.
Source https://grief.com/the-five-stages-of-grief/

Cancer Patient Care
Caring for the cancer patient consists of two general categories: Curing the cancer and supporting the patient. Curing the cancer could involve one or more of the previously discussed therapies. Caregivers should obtain a copy of the doctor’s care plan, or at least detailed instructions of what is expected of the caregiver. Be prepared to push for skilled nursing help to manage what will be required or a nurse to train and delegate tasks that must be done. It may seem overwhelming to the primary caregiver. Fortunately, you are not alone. There will be plenty of help from a whole team of medical professionals. I suggest keeping records of medical appointments, test results, medications and dosages, symptoms and side effects, and the names and telephone numbers for resources. Keep it in the resident’s file and show it to those who need to see the details. That includes the resident and their family, when appropriate.
Supporting the patient is called palliative care. It primarily involves monitoring the patient and managing their comfort levels. Basically, it’s all about maintaining normalcy or as close to normal as conditions permit. Fortunately for the resident with cancer it’s what adult foster care providers do best. We are specialists when it comes to maintaining a homelike environment for our residents. I am confident that your regular care routines will be adequate if you are prepared to handle the complications that may arise from both from the cancer and its therapy. A complete list of side effects and complications is impractical but here is a list of common ones:
- Fatigue
- Anemia
- Loss of appetite
- Insomnia
- Hair loss (mainly caused by treatments)
- Nausea (which can be very severe)
- Lymphedema
- Pain
- Immune system depression
- Weight loss
The methods involved in providing supportive care will dependent on the resources and skilled help that is available to you. Remember the adult foster care standard of monitoring for unusual behaviors and complaints, then communicating them to the doctor, pharmacist, or home health nurse. Watch for changes in your PRN logs to help catch subtle changes over time. Here are a few other caregiver tools that might help:
- The American Cancer Society publishes some very comprehensive reports under the title “Track Your Side Effects During Cancer Treatment” at: https://www.cancer.org/treatment/treatments-and-side-effects/tools-to-monitor-treatment.html
- The American Cancer Society also publishes a Pain Diary, which could be very useful in pain management. It is found on the same page as above.
- I have a three-lesson course on pain management. I call it “Pain School.”
- There are advocacy groups for just about every type of cancer that there is. You can connect with them with a few easy Internet searches. Just type in the search field the name of the cancer and the term “support group” or “advocacy group.” For example, “bladder cancer support group.”
- Remember to utilize the support you get from the pharmacy. They are usually easier to get ahold of than the doctor. Some pharmacists specialize in cancer care.
- There are research groups that conduct clinical trials on new medications and therapies. Contact your doctor to get involved in one or conduct your own Internet search. Cancer.net has a list of them here: https://www.cancer.net/research-and-advocacy/clinical-trials/finding-clinical-trial
Long-Term Side Effects
If a case of cancer has been severe or the treatment particularly powerful, complications may arise months or even years after therapy has been discontinued. There is also the chance of secondary cancer developing. The caregiver should remain vigilant to unusual occurrences and report them to the doctor. After treatment ends you might ask the doctor if additional screening tests will be required. Those tests could include thyroid tests, lung functions tests, blood counts, electrocardiograms (EKGs), mammograms, x-rays and computed tomography (CT) scans.
Survivorship
A patient who has had cancer is often called a cancer survivor. Those who go through this trial are changed by it. Emotions, relationships, perspectives, and attitudes can be altered. Some may even experience survival guilt. As the therapies are discontinued, the patient is faced with trying to get their life back to normal. Relief and/or anxiety may increase as attention from the care team is reduced. Cares, concerns, and fears may linger for years to come. The caregiver should be prepared to help the cancer survivor resident cope with the changes and emotions that cancer survivorship may produce.
Survival statistics:
The number of people who have had cancer has gone up greatly over the last 45 years in the United States. In 1971, there were 3 million people with cancer. Today there are more than 15.5 million.
- About 67 percent of today’s cancer survivors were diagnosed five or more years ago.
- About 17 percent of all cancer survivors were diagnosed 20 or more years ago.
- Nearly half (47 percent) of survivors are age 70 or older.
Source: https://www.cancer.net/survivorship/what-survivorship
When Efforts Fail
Every patient has the right to choose not to be treated for cancer. It’s hard on the caregiver but the resident has the right to refuse treatment. In my opinion it’s okay for the caregiver to question that decision. Emotions and fears can run high and cloud the resident’s judgement. The caregiver can offer education to relieve fears and offer counsel to provide proper perspective. I think it’s okay to raise objections, just as long as the resident has the final say in the matter. Respecting the resident’s right to die is part of the job. There is also the case of treatment failure. The patient may want to live but the cancer may be beyond therapy. So, what do you do when lifesaving efforts fail? The answer is that treatments may fail, or patients may refuse them, but caregiving never stops. It just switches to different goals.
When death becomes inevitable, whether by choice or treatment failure, there will be added duties to perform. Caregiving may continue but provisions must be made for making the patient comfortable and saying their farewells. The Adult Foster Care provider is in a powerful position to provide meaningful support at this end-of-life time. Not only will you find yourself giving aid and comfort, but you will also be a friend, counselor, and facilitator to both resident and family. This time of greatest need can also be a time of your greatest fulfillment as a caregiver. This being said, it is also a time of decision for the adult foster care home. Should the resident stay or move on? There are perfectly good business decisions to move a heavy care resident out. Before that choice is made, you must know that there is plenty of help available to the caregiver.
Hospice
Hospice is a philosophy and type of care that no longer tries to cure but focuses on the comfort of the patient. In the United States, Medicare and other insurers pay for end-of-life care when there is a prognosis of less than six months to live. That time frame can be extended as long as the doctor can certify a terminal diagnosis. Hospice care comprises a team of specialists that includes a hospice doctor who leads the team, nurses, respite caregivers, pharmacist, counselors, therapists, and volunteers. Usually the hospice team is employed by a hospice provider company. The patient has the right to change that company every review period.
The impact that hospice has on adult foster care is that there is always free help available 24 hours a day, seven days a week, but goals of therapy will be changed. Medical decisions will be made by the hospice doctor. He or she will concentrate on the patient’s comfort. There will no longer be any effort to cure the patient. Other therapies unrelated to the cancer may also be discontinued. The transition may be frustrating for the caregiver and challenging for the patient. No one likes change, especially the elderly and cognitively impaired. It will help to keep the channels of communication open.
When death is near, certain physiological changes will occur. Appetite and thirst will drastically reduce. Mucus may build up. Profound weakness may occur. Confusion may appear and the ability to mentally function may be reduced. Bodily functions may start to shut down. Keep calm and peaceful during this time. Move the resident’s position every few hours. Keep in mind the needs of the family during this time. It’s okay to rely heavily on the hospice care team.
- Oncology – study of tumors
- Oncologist – cancer specialist
- Malignant – a tumor that invades and spreads (metastasize)
- Benign – tumors that don’t spread or cause harmful effects
- Tumor – mass of cells that abnormally multiply
- Carcinoma – the most common form of cancer
- Sarcoma – a rare form of cancer in the supportive and connective tissue
- Tumor biopsy – tumor tissue sample
- Well differentiated – tumors that still look like the original source tissue. They generally have a good clinical outcome
- Poorly differentiated – tumors that have a more primitive structure and may not resemble its original tissue. They generally have a poorer outcome
- Tumor markers – substances produced by tumors or the body's response to the presence of a tumor
- Prostate specific antigen (PSA) – tumor marker for prostate cancer
- Ablate (ablation) – to remove or destroy the function of an organ or body tissue
- Myelosuppression – side effect of chemo where rapidly dividing bone marrow cells is killed off
- Remission – period of holding the cancer in check
- Relapse – reoccurrence of cancer
- Resect – to cut and remove a segment of an organ containing a tumor
- Alopecia – hair loss
- Apoptosis – programmed cell death
- Debulk – surgically reducing the volume or amount of cancer
- Mastectomy – surgery to remove all or part of the breast and sometimes other tissue
- Refractory – no longer responsive to treatment

Conclusion
Cancer will always be an emotionally charged, sensationally driven topic. Tragedy sells and there are few bigger attention-grabbers than cancer. Hopefully the basic info given in this course has enlightened you and cut through all that clutter. Yes, people die from cancer. It is equally true that more people are becoming cancer survivors. With ongoing research, informed caregivers, and educated patients, survivorship continues to grow year after year. Knowledge will always trump fear.
As always, good luck in your caregiving efforts
Mark Parkinson BSPharm
References:
What Is Cancer? National Cancer Institute. NIH https://www.cancer.gov/about-ancer/understanding/what-is-cancer
Cancer. Wikipedia. https://en.wikipedia.org/wiki/Cancer
Charles Patrick Davis, MD, PhD, Cancer. MedicineNet. WedMD. 8/9/2016. https://www.medicinenet.com/cancer/article.htm#what_is_cancer
Cancer Basics, What Is Cancer? American Cancer Society. 2018. https://www.cancer.org/cancer/cancer-basics/what-is-cancer.html
Understanding Cancer: Metastasis, Stages of Cancer, and More. MedicineNet. WedMD. https://www.medicinenet.com/cancer_101_pictures_slideshow/article.htm
Carcinogenesis. Wikipedia. https://en.wikipedia.org/wiki/Carcinogenesis
Epigenetics. Wikipedia. https://en.wikipedia.org/wiki/Epigenetics
One Cause to Cure. Cancer Research Institute. https://www.cancerresearch.org
Medical Terminology: Cancer. Quizlet. https://quizlet.com/64594534/medical-terminology-cancer-flash-cards/
List of Cancer Types. Wikipedia. https://en.wikipedia.org/wiki/List_of_cancer_types
Stages of Cancer. Cancer.net. American Society of Clinical Oncology. . https://www.cancer.net/navigating-cancer-care/diagnosing-cancer/stages-cancer
Keith Mulvihill. 9 Surprising Sources of Radiation in Your Home. ThisOldHouse.com https://www.thisoldhouse.com/ideas/9-surprising-sources-radiation-your-home
What Is Breast Cancer Screening? Centers for Disease Control and Prevention. 2018. https://www.cdc.gov/cancer/breast/basic_info/screening.htm
What Should I Know About Screening? Centers for Disease Control and Prevention. 2018. https://www.cdc.gov/cancer/cervical/basic_info/screening.htm
Understanding Cancer Prognosis. National Cancer Institute, NIH. 2018. https://www.cancer.gov/about-cancer/diagnosis-staging/prognosis
Prognosis and Cancer Statistics: Questions and Answers. Everydayhealth.com. 2008. https://www.everydayhealth.com/cancer/understanding/prognosis-and-cancer-statistics.aspx
Understanding Statistics Used to Guide Prognosis and Evaluate Treatment. Cancer.net. American Society of Clinical Oncology. https://www.cancer.net/navigating-cancer-care/cancer-basics/understanding-statistics-used-guide-prognosis-and-evaluate-treatment
Tumor Grade. National Cancer Institute, NIH. 2018 https://www.cancer.gov/about-cancer/diagnosis-staging/prognosis/tumor-grade-fact-sheet
Exam Portal
click on [Take Exam]
Purchase membership here to unlock Exam Portal.
|
|
|
|
|
*Important*
Registration and login is required to place your name on your CE Certificates and access your certificate history.
Username MUST be how you want your name on your CE Certificate.
| Guest: Purchase Exam |






