Let’s Have a Conversation About Diabetes
Let’s Have a Conversation About Diabetes
Author: Mark Parkinson BSPharm: President AFC-CE
Credit Hours 2- Approximate time required: 120 min.
Educational Goal:
To answer question about diabetes.
Educational Objectives:
Answer the questions, what is diabetes and what causes it.
Give a description of Type I, Type II and Gestational Diabetes.
Provide a list of risk factors for developing diabetes.
List the sign to monitor for that indicates diabetes.
Explain what the consequences of uncontrolled diabetes.
Procedure:
Read the course materials. 2. Click on exam portal [Take Exam]. 3. If you have not done so yet fill in Register form (username must be the name you want on your CE certificate). 4. Log in 5. Take exam. 6. Click on [Show Results] when done and follow the instructions that appear. 7. A score of 70% or better is considered passing and a Certificate of Completion will be generated for your records.
Disclaimer
The information presented in this activity is not meant to serve as a guideline for patient management. All procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this article should not be used by care providers without evaluation of their patients’ Doctor. Some conditions and possible contraindications may be of concern. All applicable manufacturers’ product information should be reviewed before use. The author and publisher of this continuing education program have made all reasonable efforts to ensure that all information contained herein is accurate in accordance with the latest available scientific knowledge at the time of acceptance for publication. Nutritional products discussed are not intended for the diagnosis, treatment, cure, or prevention of any disease.
Let’s Have a Conversation About Diabetes
In 2015 the Center for Disease Control reported that over 30 million people in the U.S., or 9.4 percent of the population, had diabetes. They estimated that 12.2 percent of all adults over 18 years of age were affected by the disease and 7.2 million didn’t know they had it. They also observed that the prevalence of diabetes cases increases with age, reaching a high of 25.2 percent for those 65 years of age and older. There are many indications that the prevalence of diabetes is increasing.
What does that mean for adult foster care? Up to one out every four of your current or future residents could have diabetes. Of those who do have the disease, one-quarter of them will not know they are afflicted. The implications are, caregivers need to understand the disease, recognize the symptoms, and know how to care for those with diabetes, even if no one is currently diagnosed. Let’s have a conversation about diabetes that I think will help you be prepared. You’ll ask the questions, and I will provide the answers. I will even discuss the background information so that you will understand my answers.

What Is Diabetes, You Ask?
Answer: Diabetes mellitus is a collection of conditions that create too much glucose in the blood. Simply enough said but much more complex in its understanding. For those with the disease, something has gone wrong in how glucose is processed by the body.
Background: Let’s start with how glucose is normally processed.
Before we proceed with our discussion, we must clarify a point. There are two different diseases that have the word “diabetes” attached to them: diabetes mellitus and diabetes insipidus. Diabetes insipidus is a disorder that affects the way water flows through the body. It causes excessive urination and excessive thirst. Sometimes it’s nicknamed the bed-wetter disease. They have the same first name because both of their discoveries involved observing excessive urination and excess thirst. Diabetes insipidus is a rarer condition and is unrelated to blood glucose so we will not be covering it in this course.
Glucose
Glucose is a carbohydrate molecule known as a simple sugar. It is packed full of easily accessible energy. It is our preferred source of fuel. It is very important to every cell in our body, especially the brain. Our digestive system is set up to get it from the foods we eat. Our gut either absorbs it straight from the food we eat, breaks apart other more complex sugars like starches to get it, or coverts other molecules like proteins and fats into something similar to glucose.
Having a constant fuel source is very important to our bodies. It is so important that our bodies convert excess glucose into fat and stores it away in our adipose tissues. When we can’t get enough glucose from our diet, we pull out our fat fuel stores and use them for energy. When even that is not enough fuel, our bodies break apart the proteins in our muscles and tissues and use them for energy.
Glucose as a chemical is a highly reactive molecule. It can interact in many different ways with the various molecules in our cells.
Glucose is also hydrophilic, which means it is highly attracted to and mixes easily with water. Our body utilizes that property to move the glucose around the body in the water of our blood, lymph, and urine systems. 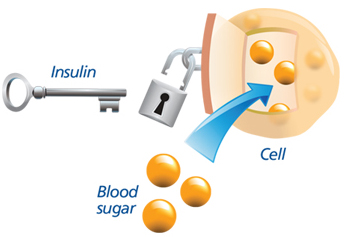
Insulin
When our cells need more fuel, they take in glucose via special molecular channels in the cell walls. These channels are usually closed to prevent leakage from the cell. It takes a special hormone called insulin to open them up. Insulin is also involved in storing away glucose as fat. The more insulin in the bloodstream, the more fat is stored away. Insulin is produced in the pancreas by specialized cells called beta cells.
That is the broad overview of how glucose metabolism normally functions. I left out a lot of details, but we have enough background to continue our talk.
I have heard there are different kinds of diabetes?
Answer: Yes, there are different types of diabetes mellitus (from now on I will just refer to them as diabetes). Their names have evolved over time as our understanding has grown.
Background: At first, doctors called everything with excessive urination and thirst diabetes. As we gained more knowledge, researchers realized that there were several different causes of those symptoms. Naturally, more descriptive names were added to help differentiate between the forms of the disease. In the past they have been referred to as juvenile and adult diabetes, early onset and late onset diabetes. Those names never quite described accurately enough what was going on. Currently the most common forms of the condition are simply referred to as Type I, Type II and Gestational diabetes. There are other forms of the disease, but they are rare, so we will not be covering them. Let’s talk further about the common varieties.
Type I
 In Type I Diabetes the body has lost the ability to make enough insulin to meet its needs. Without insulin, glucose can’t get into the cells. This triggers a series of metabolic events in the body. The cells send signals to the brain that they need more fuel. The brain automatically triggers an increase in appetite. The person eats more food, which results in more glucose in the bloodstream, but there’s no place for it to go. Normally excess glucose is stored away as fat, but insulin is also required in the fat storage system of our body so there is still no place for the glucose to go. Eventually the excess glucose spills out through the urine. Water follows the sugar out, so urination volume increases. Soon the body becomes dehydrated due to the increased urine volume. Soon the thirst drive increases to compensate for the loss of water. In the meantime, the cells still lack fuel so they can’t function well. The body starts to pump out its fats stores to try to make up the difference, but without insulin it’s to no avail. The body has run out of fuel, so its systems start to shut down.
In Type I Diabetes the body has lost the ability to make enough insulin to meet its needs. Without insulin, glucose can’t get into the cells. This triggers a series of metabolic events in the body. The cells send signals to the brain that they need more fuel. The brain automatically triggers an increase in appetite. The person eats more food, which results in more glucose in the bloodstream, but there’s no place for it to go. Normally excess glucose is stored away as fat, but insulin is also required in the fat storage system of our body so there is still no place for the glucose to go. Eventually the excess glucose spills out through the urine. Water follows the sugar out, so urination volume increases. Soon the body becomes dehydrated due to the increased urine volume. Soon the thirst drive increases to compensate for the loss of water. In the meantime, the cells still lack fuel so they can’t function well. The body starts to pump out its fats stores to try to make up the difference, but without insulin it’s to no avail. The body has run out of fuel, so its systems start to shut down.
Symptoms that caregivers should watch for in Type I diabetics are they always hungry, thirsty, and have to urinate a lot. They are weak and tired all the time and have a hard time thinking. Their fats stores get used up, which results in unexplained weight loss. The onset of this type of diabetes tends to happen very quickly.
What happened to the insulin?
Answer: The body accidently killed off the beta cells in the pancreas in an autoimmune response.
Background: Our immune system fights off invading microorganisms by having watchdogs, so to speak, patrolling the blood system. They’re called antibodies. When they detect a foreign material (scientifically called an antigen) they latch onto it. Then several things happen. Two important things in regard to Type I diabetes are: 1. The antibody connects to killer T cells and they destroy the antigen. 2. The T cells and the antibodies start to replicate and so are primed to kill off anything that looks like that original antigen. Unfortunately, there are antigens that are very similar to certain parts on the cell wall of Beta cells. In victims of Type I diabetes the immune system fights off the infection and goes after the beta cells too and wipes them out. Type I diabetes mostly affects children, but older adults can be affected too. Caregivers should watch for the signs of thirst, hunger, and fatigue in their residents who just got over a cold or flu.
Type II
Type II diabetes is a condition of insulin resistance. The pancreas’s beta cells are still there, but insulin is not having its full effect. Something is going wrong that is preventing the glucose from entering the cell as readily as it should. To compensate, the body starts to work harder in other areas. It keeps things going normally for a while, but it comes with extra costs. Eventually the costs become too high and the overworked systems start to fail. Gradually the classic diabetic symptoms start to appear. If steps aren’t taken to treat the disease, the symptoms get progressively worse.
What would it look like if one of my residents started to develop Type II Diabetes?
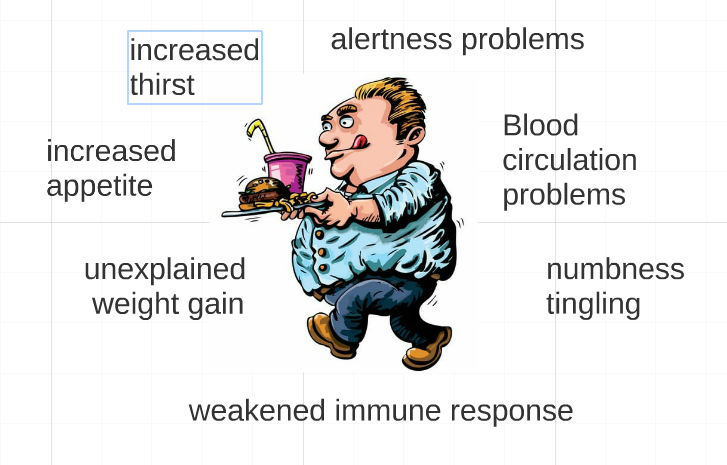
Response: At first, they would start having minor annoying symptoms that are easily ignored. But, you would start to notice that the problems are not going away by themselves. As the condition progresses, the annoyances would go from mild to moderate. The resident would start to complain more, and the symptoms would become more pronounced. Caregivers would start to see some of the following signs:
- Increased appetite – The glucose-starved cells continue to send out “feed me” signals. The brain receives those signals and increases hunger.
- Numbness and tingling – The extra “highly reactive” glucose attaches to nerve endings and disrupts their functions. Diabetics start to feel tingling or numbness in their fingers and toes.
- Weakened immune response – Glucose can fasten itself to parts of the immune system and reduce its ability to fight off infections. Wounds, scrapes, and sores take forever to heal.
- Blood circulation problems – Glucose can also attach to the walls of blood vessels, causing a host of other issues. At first it affects the smaller blood vessels and is seen as blood circulation problems (cold fingers and toes), and vision problems.
- Unexplained weight gain – The beta cells are stimulated to pump out even more insulin to meet the extra need. The extra insulin stimulates more glucose to be stored away as fat. In type II diabetics this usually shows as unexplained weight gain, especially around the waist.
- Increase in thirst – The body starts to lose too much water through urination. It will start to show as itchy, flaky skin; dry, cottony mouth; and of course, extra thirst.
- Alertness and drive problems – Individual cells have problem functioning due to a lack of fuel. Collectively this shows as lack of drive and energy, mental fuzziness, and increased irritability.
I’ve heard of prediabetes, is that what we are talking about?
Answer: Yes, officially prediabetes means that the blood glucose is higher than normal but not enough to be diagnosed with diabetes. Unofficially some clinicians include the outward signs of Type II Diabetes, like being overweight. Practically speaking, all that prediabetes really means is something might be going wrong, so pay attention and help the resident start to live a healthier lifestyle.

Gestational Diabetes
Gestational diabetes happens only in pregnancies and we have not nailed down exactly why yet. We do know that hormones produced by the placenta play a role. For some women, they seem to make it difficult to produce enough insulin. The extra weight and genetic makeup may also be a factor. Fortunately, the condition goes away after the pregnancy is done, but not for everyone. Those who do get gestational diabetes are now at greater risk for Type II diabetes. Like Type I diabetes, insulin shots may be needed right from the start to keep blood glucose down to healthy levels. Since pregnant residents in care homes are as rare as vegetarians at a hot-dog- eating contest, that is all we are going to talk about the subject.
What causes Type II diabetes?
Answer: We don’t know. Research has not figured out all the different causes yet.
Background: The insulin-glucose system is actually a very complex series of metabolic steps. Think of it as a long trail of dominos. If one domino falls, it triggers a chain reaction that eventually gets the glucose where it needs to be in the cell. Just like with a chain of dominos, if there is a problem anywhere in the series of actions, the final reaction does not take place and glucose can’t get into the cell. So far medical science has not been able to point at the one domino that’s the root of the problem. There even may be several factors involved.

Even though we have not figured out all the specifics yet, we do have a handle on the bigger picture. We can point to a list of characteristics that put people at greater risk for developing the disease. If caregivers knew which of their residents were at greater risk, they could start to monitor them more closely for the telltale signs.
What are the risk factors that I should be looking for?
Response: The risk of developing type 2 diabetes depends on a combination of factors. The more risk factors involved, the more closely you should monitor the resident. Here is what you should be looking for.
- Genetics – It all depends on how you are built in the first place. The resident may have inherited a broken “domino,” or a weak one which will break if overworked. Caregivers need to get and pay attention to family histories containing cases of diabetes.
- Race – This is inherited genetics again, but on a larger scale. African Americans, Mexican Americans, American Indians, Native Hawaiians, Pacific Islanders and Asian Americans are at higher risk. These groups may be at higher risk because of their genes and/or the lifestyles they are known to have. For example, this could include being overweight because of the kinds of foods their family traditionally eats.
- Lifestyle – Eating a diet that results in being overweight or obese, coupled with inactivity, puts a lot of stress on the insulin glucose system and is unhealthy for the whole body.
- Age – In general, the longer you use anything, the easier it is to break it. Those who are 45 years or older are at greater risk of developing symptoms.
- Drugs – Sometimes medications can harm beta cells or put stress on the insulin-glucose pathways.
A list of drugs that may have the risk of diabetic side effects are:
|
- Health problems – Other health problems that affect the entire body or the pancreas can put stress on or break the insulin-glucose pathway.
List of health problems that are risk factors for diabetes:
|
Isn’t there some kind of outward sign that tells me that diabetes is starting to occur?
Answer: Type I diabetes occurs very fast. The classic diabetes signs of thirst, urination, hunger, fatigue, and mental confusion could happen in a matter of weeks, if not days. Type II diabetes happens so gradually, though, that it’s hard to recognize the classic signs. There are a couple of red flags you could watch for. One is having frequent urinary tract infections (UTI) and the other is called acanthosis nigricans.
Background – UTI
Normally the bacteria and fungi living in the urinary tract system are easily controlled by our body’s defenses. In diabetes, two things happen that throw off that balance. 1. The extra glucose in the urine becomes a food source for all the bacteria and fungi and they multiply at a greater rate. 2. The immune system has been compromised by the extra glucose hanging around. The result is that UTIs are more likely to happen. If your resident has more than three UTIs in a year, or has a kidney infection, it’s time to test for diabetes.

Background – acanthosis nigricans
Acanthosis nigricans is a skin condition that affects diabetic patients. It appears as dark, thick, and velvety skin around the neck or armpits. Look specifically at where the skin creases and folds. It kind of looks like dirt and sweat buildup, but it won’t wash off.
I have an interesting personal story about acanthosis nigricans. Back when I was a pharmacy student, I was taught in-depth about diabetes. I was in class a long time memorizing and studying all the details. Somewhere in all those hours of study I started to notice the prediabetes signs and risk factors appearing in my wife. She had a sister with Type II diabetes, she kept getting yeast infections, and she was tired all the time, gaining weight and being miserable. I told her that she might have diabetes. You know what she said? “Are you sure?” Of course, I wasn’t sure, I was just a student. All those signs could be explained away by other conditions. Then I learned about acanthosis nigricans. I looked at her neck. Sure enough, a dark line had formed in the crease at the back of her neck. We had her blood glucose tested to confirm she had Type II diabetes. We had caught the condition early enough. To this day she has been able to avoid all the bad consequences of being a diabetic, and it’s all thanks to a student who was paying attention and a dirty-looking grey line at the back of her neck. I hope my story will be an inspiration to you to monitor your residents.
Wait a minute!
If no one is sure what causes diabetes, how can the doctor be sure my resident has diabetes?
Answer: There are definitive blood tests that the doctor can give the resident. They are Fasting Plasma Glucose Test (FPG), Random Plasma Glucose Test (RPG), and Glycated Hemoglobin Test (A1C).
Background: Glucose is highly regulated in our bodies. We are built to keep the concentration of blood glucose (blood sugar) at a certain level. Higher-than-normal concentrations just don’t happen normally. If the glucose concentration is higher as shown in these tests, the doctor knows for sure that something is wrong.
Random Plasma Glucose Test: A blood sample is taken and placed in a blood glucose meter. If the reading is higher than 200 milligrams per deciliter (mg/dL) then diabetes is suspected. RPG is the least accurate of all the tests but easiest to administer. It’s usually used as a screener test.
Fasting Plasma Glucose Test: FPG is more accurate and involves not eating anything for eight hours. Then a blood sample is placed in the blood glucose meter. A reading of 100 to 125 mg/dL is considered prediabetes. If it's 126 mg/dL or higher on two separate tests, you have diabetes.
Glycated Hemoglobin Test: A1C is more accurate than RPG and does not involve fasting. If glucose hangs around too long it can become attached to a hemoglobin cell or it becomes “glycated.” Normally it doesn’t happen very often. An A1C test measures the concentration of the glycated hemoglobin in a blood sample. Any results 6.5 percent or higher on two separate tests indicates that the resident has diabetes. An A1C between 5.7 and 6.4 percent indicates prediabetes. Below 5.7 is considered normal.
There is another even more accurate test. It’s called an oral glucose tolerance test. After fasting you drink a glucose solution. Then, at certain times over the next two hours a blood sample is taken, and the glucose concentration is measured. It is usually reserved for tough cases because who wants to sit around for two hours and get poked all the time?
I had one of these tests in college. The professor wanted us to understand the concept. The syrup was labeled root beer flavored, but you almost couldn’t tell. It was the most potent sweetness I have ever experienced. It almost made me gag. Giving the blood samples wasn’t fun either. The professor made us poke ourselves. It turned out I didn’t have diabetes.
It seems to me that this is a lot of hassle. Why don’t I just let the doctor handle all this diabetes stuff?
 Response: Yes, you could. Many fine caregivers have that same attitude. Here are a few things to consider, though. How often does a resident see the doctor? How long will that resident be in the same room as the doctor? Will that doctor be looking for diabetes symptoms? Doctors don’t normally screen for diabetes unless there are signs and symptoms. Will the resident tell the doctor about the small stuff that may be a sign of diabetes like, “I’m hungry and thirsty and need to pee a lot”? I think you are starting to see why there are so many undiagnosed diabetes patients. You certainly don’t have to be proactive about diabetes, but there may be consequences to that decision. I hate to think of what would have happened to my wife if I had not made those observations.
Response: Yes, you could. Many fine caregivers have that same attitude. Here are a few things to consider, though. How often does a resident see the doctor? How long will that resident be in the same room as the doctor? Will that doctor be looking for diabetes symptoms? Doctors don’t normally screen for diabetes unless there are signs and symptoms. Will the resident tell the doctor about the small stuff that may be a sign of diabetes like, “I’m hungry and thirsty and need to pee a lot”? I think you are starting to see why there are so many undiagnosed diabetes patients. You certainly don’t have to be proactive about diabetes, but there may be consequences to that decision. I hate to think of what would have happened to my wife if I had not made those observations.
What are the consequences of uncontrolled diabetes?
Response: Uncontrolled Type I diabetes is deadly. If nothing is done, the patient will quickly end up in the hospital. Uncontrolled Type II diabetes is also very harmful. Eventually it will lead to multiple health problems, hospitalization, or death.
Background: Type I – When there is not enough insulin, cells starve. The brain is particularly sensitive to a drop in glucose. The brain will send signals to start breaking down our fat stores. When fat is broken down for fuel, a byproduct chemical called a ketone, which is acidic, is produced. During Type I diabetes there is so much fat being broken down that it leads to a high concentration of ketones in the blood. This leads to Ketoacidosis. In ketoacidosis the blood has become too acidic, which can lead to a coma and death. Those who are beginning to experience ketoacidosis become confused, agitated, have a red face, breathe rapidly, and have a fruity breath.
If you see this in your residents, call 911.
Background: Type II – When there is too much glucose in the bloodstream for a long period of time, it starts to combine with tissues and causes harm in multiple ways. Diabetes Type II is also a condition of having too much lipids (fatty molecules in the bloodstream). It also adds to the patient’s long-term health problems.
The long-term consequences are:
- Small blood vessels and capillaries. Glucose will stick to the walls of small blood vessels interfering in the proper function. Blood flow is affected, leading to circulation, eye, and kidney problems.
- Major blood vessels. Eventually the larger blood vessels are also damaged by the glucose and lipids (fats). This leads to bladder problems, kidney failure, strokes, and heart attacks.
- Nerve system. Long-term exposure to glucose can kill nerve cells, leading to numbness, tingling, and constant nerve pain. Injuries cannot be felt and are left untreated.
- Immune system. Glucose can prevent parts of our immune system from working. Infections happen more often, and our body has a harder time removing damaged or malfunctioning cells. Infections occur but the diabetic can’t feel them. The infection grows to dangerous levels before they are treated. This leads to gangrene and amputations. Infections also lead to dental and gum disease. Malignant cells are not detected and destroyed by the immune system, leading to an increased chance for cancer developing.
- Eventually the overworked beta cells wear out, resulting in a lower insulin production. Lower insulin levels hasten the occurrence of diabetes symptoms.
Conclusion
If you are having a hard time wrapping your brain around all of this diabetic stuff, picture in your mind’s eye a vision of what is commonly called a “brittle diabetic” case. They will be morbidly obese, sitting in a wheelchair due to a foot amputation, blind from eye disease, and constantly complaining of nerve pain and being cold from lack of circulation. They will never smile or interact with others because they have bad teeth, bad breath, and a smell of incontinency. Finally, they will die of a heart attack—but not before suffering from one or more strokes first. I know I have laid it on pretty thick trying to make my point. I hope you can see, though, that proactive diabetes monitoring and care is worth the effort.
As always Good Luck in your caregiving.
Mark Parkinson BS Pharm
References:
What is Diabetes? National Institute of Diabetes and Digestive and Kidney Diseases, NIH. 2018. https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes
National Diabetes Statistics Report, 2017. Centers for Disease Control and Prevention. 2017 https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf
Diabetes Mellitus. Wikipedia. https://en.wikipedia.org/wiki/Diabetes_mellitus
Diabetes insipidus. Mayoclinic.org. 2018 https://www.mayoclinic.org/diseases-conditions/diabetes-insipidus/symptoms-causes/syc-20351269
Age, Race, Gender & Family History. American Diabetes Association. 2017. http://www.diabetes.org/are-you-at-risk/lower-your-risk/nonmodifiables.html#Race
Prediabetes. Mayoclinic.org 2018. https://www.mayoclinic.org/diseases-conditions/prediabetes/symptoms-causes/syc-20355278
Gestational Diabetes. National Institute of Diabetes and Digestive and Kidney Diseases, NIH. 2018. https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/gestational
Diabetes. Mayoclinic.org. 2018. https://www.mayoclinic.org/diseases-conditions/diabetes/diagnosis-treatment/drc-20371451
Carmella Wint and Marijane Leonard. What You Should Know About Diabetic Ketoacidosis. Healthline.com. Dec.4 2018. https://www.healthline.com/health/type-2-diabetes/ketoacidosis#causes
Exam Portal
click on [Take Exam]
Purchase membership here to unlock Exam Portal.
|
|
|
|
|
*Important*
Registration and login is required to place your name on your CE Certificates and access your certificate history.
Username MUST be how you want your name on your CE Certificate.
| Guest: Purchase Exam |