Mental Health First Aid- A Caregiver’s Plan to Deal Mental Health Occurrences 2
A Caregiver’s Plan to Deal
Mental Health Occurrences
Author: Mark Parkinson BsPharm: President AFC-CE
Credit Hours 3 - Approximate time required: 180 min.
Educational Goal
Provide a way for Adult Foster Care Providers to better manage problems due to mental health issues by using Mental Health First Aid.
Educational Objectives
- Introduce the concept of Mental Health First Aid
- Tell Mental Health caregiving insights
- Present Mental Health Statics
- Provide the details of the Mental Health First Aid caregiving technique.
- Expound on the ALGEE action plan.
Procedure:
Read the course materials. 2. Click on exam portal [Take Exam]. 3. If you have not done so yet fill in Register form (username must be the name you want on your CE certificate). 4. Log in 5. Take exam. 6. Click on [Show Results] when done and follow the instructions that appear. 7. A score of 70% or better is considered passing and a Certificate of Completion will be generated for your records.
Disclaimer
The information presented in this activity is not meant to serve as a guideline for patient management. All procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this article should not be used by care providers without evaluation of their patients’ Doctor. Some conditions and possible contraindications may be of concern. All applicable manufacturers’ product information should be reviewed before use. The author and publisher of this continuing education program have made all reasonable efforts to ensure that all information contained herein is accurate in accordance with the latest available scientific knowledge at the time of acceptance for publication. Nutritional products discussed are not intended for the diagnosis, treatment, cure, or prevention of any disease.
A Caregiver’s Plan to Deal Mental Health Occurrences
Reference
I recently came across a new concept in health care developed in Australia in the year 2000: Mental Health First Aid. I was intrigued by the topic, so I took a course called “Introduction to Mental Health First Aid: Pharmacy Activity.” The lesson was “created in partnership with the National Council for Mental Wellbeing and the American Pharmacist Association.” I took the information I gained there and adapted it for use in Foster Care Homes.
Authors
Kelly Gable, PharmD, BCPP, Professor, Department of Pharmacy Practice, Southern Illinois University at Edwardsville; Jerry McKee, PharmD, MS, BCPP, Director of Pharmacy Community Care of North Carolina
To save time and make the course more readable, quotes from the authors will look like “Early Intervention Tool” without using their names.
Please consider the original program as this course's primary source of reference. I know it’s different to put the reference section at the front instead of the back of the article. That’s just the “slightly off-kilter” kind of guy I am. I hope you find some use in this material.
Mental Health First Aid
Mental Health First Aid is the appropriate steps you take when you first encounter someone experiencing a mental health crisis. In general, you make sure the situation is safe to act in, stabilize the patient’s condition, and connect the patient to medical professionals. First Aid responders are not trying to be Doctors or cure the patient. They are just trying to get the patient safely to the doctor.
If that concept has a familiar ring to it, you are right. That is basically what foster care professionals do all the time for any medical condition experienced by their residents. As a profession, we have gotten pretty good at it too. But you have to admit, some of the toughest situations always seem to involve behavioral issues. How many of you readers have flopped around in a difficult situation involving unusual mental behaviors? I myself remember thinking on several occasions, “Well, that certainly could have gone better. That felt like I just shot myself in the foot trying to help. There has got to be a better way to handle that kind of situation.” Well, according to the National Council for Mental Wellbeing, there is a better way.
But first I would like to add my two cents to the pot.
My two cents worth
As we go through life, we learn a certain way to interact with those around us and we call that “normal behavior”. If someone behaves “abnormally” we all try to influence that person to act “normally” again. That works for the most part if that abnormally behaving person has the capacity to think normally. It does not work so well in situations where something is broken mentally, and they can’t think normally.
Let me expound on the point by using an example of a different physical problem. If someone breaks a leg, we naturally allow that person to behave differently. We know that an injured person can’t get up and run to the hospital, so we don’t expect them to. Those who are trying to help naturally put in a lot of additional effort to assist the injured person in getting to the hospital.
The difference between the two patients is we can easily see the broken leg and make the necessary allowances. But we can’t readily see the broken thinking happening inside the patient's mind. So we are reluctant to make allowances for their abnormal behaviors. We resent having to put in additional effort. The predictable results are, we end up flopping around a lot and making a general mess of things.
My advice to avoid the flopping around mess comes in three steps.
- Be flexible in what you call normal behavior. All your residents by definition are not normal. If they were normal, they would not be living with you
- Have extra patience in abnormal behavior situations. Don’t be in a rush to try to influence normal behavior. Take a couple of breaths before acting.
- Be aware of what is normal behavior for that resident. Then when abnormal behavior happens for them ask yourself, “Why is this occurring” before acting.
My second piece of advice for you is, Adjust your behavior to fit their perception of reality. But only do so if you have determined that something is broken mentally. As long as you keep everyone safe and cared for, your caregiving labors will be much easier by doing so. An example of that would be -If a dementia patient says the sky is pink, then say what a lovely shade of pink it is. No one is being hurt and it would take way too much effort to try to convince the dementia patient to think otherwise. Ask yourself these questions. Is it worth the effort to try to change their perception of things? Can you get the job done by just going around the abnormal behavior?
In the following material for mental health first aid responders, they refer to the above as “thinking non-judgmentally”. As a caregiver who lives with the patient, you have the opportunity to take that way of thinking to the next level. Okay, I’ve said my two cents - let’s begin.
Mental Illness
Temporarily acting differently and an actual mental illness are two different things. The first is choosing to act in a certain way. The second occurs because of involuntary events that are happening within a mental illness sufferer that lead to outward signs and symptoms of a mental disorder. According to the authors, “A mental disorder or mental illness is a diagnosable illness that disrupts a person’s ability to:
- Carry out daily activities living
- Engage in satisfying relationships
- Participate in regular social interactions like work
The key phrase here is diagnosable. Or in everyday terminology- tying a set of symptoms to a particular mental disease. Diagnosing a mental illness is really quite difficult. Fortunately, that is the doctor's job. You do not have to place a label on any set of abnormal behaviors. (Even though we are tempted to do so every single time). In-Home caregivers only have to suspect something is going wrong and get the resident to the appropriate medical provider.
Prevalence of Mental Illness
Mental illnesses are common in the United States and around the world. It is estimated that more than one in five U.S. adults live with a mental illness (59.3 million in 2022; 23.1% of the U.S. adult population). Source: https://www.nimh.nih.gov/health/statistics/mental-illness
To you, 1 in 5 may not be a believable static. It seems to report that the world is overflowing in crowded with crazy people. The explanation is, that mental illness symptoms come in a spectrum of severities. From no symptoms to severe. Also, those symptoms wax and wane over time. Because of the variability in symptom manifestation, statistical information is beginning to be reported in two broad categories, AMI and SMI. AMI is Any Mental Illness and SMI is Severe Mental Illness.
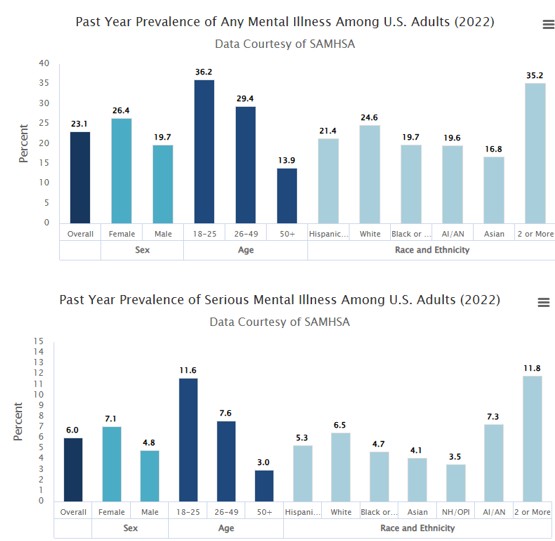 Source: https://www.nimh.nih.gov/health/statistics/mental-illness
Source: https://www.nimh.nih.gov/health/statistics/mental-illness
The authors reported “About 6 percent of adults, (1 in 17) suffer from a serious mental illness. Reporting an average of 88 days, approximately 3 months, during the past year when they were too ill take carrying out their normal daily activities. Across a person’s lifetime, people have a nearly 50/50 chance of having a mental illness at some time.”
Two more prevalence stats that I need to bring to your attention before making any conclusions. The first is “People often delay getting treatment for almost all mental disorders. The median delay for seeking treatment was 10 years. Worldwide median delays can range from 3 to 30 years for anxiety disorders. 1 to 14 years for mood disorders and 6 to 18 years for substance use disorders. The second is that “Many people suffer from more than one mental disorder at a given time. Nearly half, (45%) meet the criteria for two or more disorders.
So why did I just torture you with all these numbers and graphs? The facts are that the prevalence of mental disorders is greater than what you might have first thought. We don’t notice them often, because they are hidden from the public eye. It may even be hidden or disregarded by the patients themselves. Surfacing mental health issues in your residents may have started years before they came into your care. Even if they have come to you with a diagnosed mental illness there might be a second undiagnosed illness that is starting to manifest itself in your home. Now you, as the main caregiver, have to recognize the warning signs and know what to do. Hopefully, this course will help you be prepared with the tools of Mental health First Aid.
How to Think About Therapy Interventions
One last thing we need to touch on before we get into the mental health first aid techniques. You may be used to thinking of illness as a change in the biology of the body of the patient. For example, a broken leg, an infection, or a malfunction of the heart. To treat an illness, you work on altering the body to get back to normal functioning. Set the broken bone, kill off the infection with an antibiotic, and take medication that helps the heart to function normally. The goal of therapy is to regain normal bodily functions.
 In mental health therapy, the focus is more on the behaviors of the patient. The impact of the illness is measured as a loss of the patient’s ability to act normally. So also, the goal of therapy is the recovery of normal levels of behavioral activity in society despite their mental illness. The authors quoted the President’s New Freedom Commission on Mental Health “Recovery is the process in which people are able to live, work, learn and participate fully in their communities.,,.For some , this is the ability to live a fulfilling and productive life despite a disability….For others, recovery implies the reduction or complete remission of symptoms.”
In mental health therapy, the focus is more on the behaviors of the patient. The impact of the illness is measured as a loss of the patient’s ability to act normally. So also, the goal of therapy is the recovery of normal levels of behavioral activity in society despite their mental illness. The authors quoted the President’s New Freedom Commission on Mental Health “Recovery is the process in which people are able to live, work, learn and participate fully in their communities.,,.For some , this is the ability to live a fulfilling and productive life despite a disability….For others, recovery implies the reduction or complete remission of symptoms.”
I find a surprising amount of correlation between the recovery process of mental illness and the operations of an Adult Foster Care home. Both focus on the patient being able to live a fulfilling life regardless of any disability the resident/patient might be experiencing. Quite a natural fit if I do say so myself. The important takeaway of the above is that In-Home care providers have to start thinking of behaviors as part of the illness and recovery process. Having a good day behaviorally would be on the same level as reducing a fever in an infection. Having a bad day behaviorally would be on the same level as an infection relapse. That changes the way we look at disruptive behaviors, doesn’t it?
Disruptive behaviors are a perfect lead into mental health first aid techniques.
 First Aid for Mental Illness Occurrences
First Aid for Mental Illness Occurrences
Just like in regular first aid, there are general steps to take when appropriately responding to a mental illness emergency. They are:
- Recognize that an acute mental health issue is occurring.
- Ensure that it is safe to respond.
- Stabilize the patient’s condition
- Connect the Patient to the appropriate medical personnel.
For Adult Foster Care providers, there is a fifth step that needs to be taken later on. Obtain instruction on therapy and provide the necessary follow-up.
Recognizing
Every mental illness has its own set of behavioral symptoms. Don’t worry about correctly labeling each occurrence. Your job is to just suspect something is happening that is different than your resident’s normal behavior. Remember, when something annoying or weird happens, pause before responding and ask yourself “Why is that happening?”.
Ensuring Safety
Be aware of the surroundings and the mental state of the residents. Be in control of dangerous objects. Always have an escape route for yourself and others planned. Assess if the resident is in a mental state where they could harm themselves or others. If you determine that harm will likely happen, it might be wiser to call for reinforcements or emergency responders. There are specially trained first responders who can handle dangerous mental health issues.
Stabilizing
In mental health issues, stabilization involves calming the resident and reducing the stress of the situation. Often that can be achieved by just non-judgmentally listening. Listening also includes not trying to “fix the problem”. Remember you are not the doctor. You are not allowed to try to cure the patient. The goal of stabilization is to get the patient in a frame of mind where further therapeutic actions can be taken- later on. Having said all that there may be times when the situation escalated too quickly. Always be on the lookout for the possibility of suicide attempts or acts of violence and be ready to act accordingly.
Connecting with Medical Professionals
For mental health issues, this might be a little bit more complicated for In-Home caregivers than what you might think. You are in charge of transportation, not the patient. It’s your job to ensure your resident gets to the right medical professional. Do you contact the Primary Care Physician? Does a mental health specialist need to be involved? If so, do you need a referral from the PCP to see one? What does the insurance say needs to be done to ensure payment? Is it easier to send the resident to the Psych ward of the local hospital and sort out the doctor stuff later? Do you use your car or is 911 dispatching an ambulance better? What about just talking to a crisis helpline over the phone?
I have no ready answer for you. No algorithm to follow. Just the general statement, It depends on the seriousness of the situation and how cooperative the resident is. You and the resident will have to live with the consequences of your decisions. Err on safety and go with what you know. If you don’t know anything and you have a previously diagnosed mental health issue in one or more of your residents, you better get in the know before an emergency happens. After you take this course, I recommend you sit down and come up with a plan of action. If you’re the owner of the AFC home, you must instruct your support staff on what to do in cases like these.
- Here are some techniques I used to de-escalate a situation and gain more cooperation from an uncooperative resident.
- Reduce the amounts of decisions the resident has to make to the bare minimum. Make all the decisions for them and only let them choose if they refuse your
- Always blame or reference someone who is not there to argue with. “The doctor gave the instructions. The State requires me to do it this way. The insurance won’t pay unless we… etc. Once they realize you are not the source of the pressure on them, you can look like you are on their side. You are just trying to help them get what they need and want. You go from zero to hero in a few moments of thought.
- Refer to your actions and not theirs, so they can’t argue with you about it. “I think this is beyond my ability to help”, and “Let’s get you some better help”. “I don’t quite understand all the implications of what you’re going through so let’s get you to somebody who can understand”. “The state does not allow me to do that, let get you to someone who does have that authority”.
- Make it look like you’re on their side of the issue. “I sympathize with what you say, But- See number 2.” Also you might say “I see your point but what about- name a bad consequence that might happen. I don’t want it to happen to you”.
- Give them off-handed compliments about how smart they are if they agree with you. “You're smart enough to know that it’s the (name the mental illness) that’s talking not you.” “I know what you’re saying but I think you are much too smart to-fill in response (….fall for that, ….look foolish for continuing to shout, …give into thoughts of suicide)”.
B- For In-Home caregivers connecting the paper trail is just as important as connecting the patient. Always send a copy of your patient files with the resident. Add a section that requires medical staff to complete, containing instructions and follow-up details from the doctor.
I hope these hints are helpful to you. Let’s continue.
Mental Health First Aid: The Action Plan
Once you recognize your resident is just not acting up but is in the middle of an acute mental health crisis, it’s time to change from an In-Home care worker to a mental health first aid responder. This is where the Mental Health First Aid Action Plan comes into play. The action steps come in an easily remembered anagram called- A.L.G.E.E
Some more helpful hints
Remember at no point along this path are you trying to resolve the issue. Unless you have standing orders from the doctor. Do not try to initiate therapy on your own. You’ll just get in trouble with the State. It’s much easier to just shove this burden onto the shoulders of trained mental health professionals.
If there is a good chance of this becoming a regular event, I recommend that you become good friends with the professionals that you will be calling upon. Visit their offices and introduce yourself. Bring a treat with you so that you will be remembered favorably. Explain to them what an Adult Foster Care home is and how you will be interacting with them. Show them an example of the files you will be giving them and ask them if they need anything else. For Mental Health foster care homes, I would say this is almost a requirement in operating your home.
Get it, Got it, Good. Moving on.
The following explanation of ALGEE comes straight from the Mental Health First Aid website located here.
And I quote:
A – Approach, assess for risk of suicide or harm. Try to find a suitable time or place to start the conversation with the person, keeping their privacy and confidentiality in mind. If the person does not want to confide in you, encourage them to talk to someone they trust.
L – Listen nonjudgmentally. Many people experiencing a challenge or distress want to be heard first, so let the person share without interrupting them. Try to have empathy for their situation. You can get the conversation started by saying something like, “I noticed that …” Try to be accepting, even if you don’t agree with what they are saying.
G – Give reassurance and information. After someone has shared their experiences and emotions with you, be ready to provide hope and useful facts.
E – Encourage appropriate professional help. The earlier someone gets help, the better their chances of recovery. So, it’s important to offer to help this person learn more about the options available to them.
E – Encourage self-help and other support strategies. This includes helping them identify their support network, programs within the community, and creating a personalized emotional and physical self-care plan.
It is important to remember that there is no one-size-fits-all approach to executing the Mental Health First Aid (MHFA) Action Plan — you don’t even have to use every single step to provide support — and every situation will be different. If you are ever in a crisis situation where the person you are supporting is thinking about harming themself or others, or is acting erratically, call 911 immediately, and tell the dispatcher that responders with specific training in mental health or crisis de-escalation are needed. In non-crisis situations, you can go through the MHFA Action Plan and offer support to the person in need.
Regardless of the nature of the situation, staying calm is crucial as you offer support. Remember that your role is not to diagnose someone or solve the problem, but instead to provide support and information. By using the MHFA Action Plan, you can Be The Difference* and truly help someone who may need it.
End quote. *(emphasis added)
Adjustment for In-Home Caregivers
 ALGEE is written from the view of an outsider looking in at the situation. It asks the first aider to encourage the patient to take certain actions. For a patient living in an Adult Foster Care home, it is the responsibility of the In-Home care provider to do certain steps, like making an appointment with the doctor. The emphasis changes for the E steps from Encourager to Facilitator. The outcome changes from hoping the patient responds to ensuring the patient takes action. I hope that you can see that if an Adult Foster Care provider is the mental health first aid responder the ALGEE action plan becomes even more powerful. By following the plan, the Adult Foster Care provider goes from flopping around and making a mess to a bringer of hope and recovery.
ALGEE is written from the view of an outsider looking in at the situation. It asks the first aider to encourage the patient to take certain actions. For a patient living in an Adult Foster Care home, it is the responsibility of the In-Home care provider to do certain steps, like making an appointment with the doctor. The emphasis changes for the E steps from Encourager to Facilitator. The outcome changes from hoping the patient responds to ensuring the patient takes action. I hope that you can see that if an Adult Foster Care provider is the mental health first aid responder the ALGEE action plan becomes even more powerful. By following the plan, the Adult Foster Care provider goes from flopping around and making a mess to a bringer of hope and recovery.
This is Just a Start
This CE course is just an introduction to the principle of Mental Health First Aid. More in-depth training is available from the National Council for Mental Wellbeing. For more information visit their website at https://www.mentalhealthfirstaid.org/take-a-course/ Or you can go to https://www.mentalhealthfirstaid.org/take-a-course/ to see course availability in your area. If you ask in advance the county AFC licenser would probably give you CE credit for it.
Here is a sampling of the training, And I quote:
It’s hard to be nonjudgmental all the time. We automatically make judgments about people from the minute we first see or meet them based on appearance, behavior, and what they say. And that’s okay. Nonjudgmental listening isn’t about avoiding those judgments – it’s about making sure that you don’t express those negative judgments because that can get in the way of helping someone in need.
When you’re trying to be there for your friend, neighbor, or colleague, it’s important to maintain a positive attitude and open mind to truly be supportive. Use these Mental Health First Aid tips to be an effective nonjudgmental listener for those around you.
- Reflect on your own state of mind.
Before approaching someone with your concerns, it’s important to make sure you are in the right frame of mind to talk and listen without being judgmental. Reflect on your own state of mind to make sure you are feeling calm, open, and ready to help your peer in need.
- Adopt an attitude of acceptance, genuineness, and empathy.
Adopting an attitude of acceptance means respecting the person’s feelings, personal values, and experiences as valid, even if they are different from your own or you disagree with them. Taking time to imagine yourself in the other person’s place can help you be more genuine and empathic.
- Use verbal skills to show that you’re listening.
Simple verbal skills can help you show the person that you’re actively listening. This includes asking questions, listening to tone of voice and nonverbal cues being used, using minimal prompts like “I see” and “ah” and not interrupting the person to give them time to express their thoughts and feelings.
- Maintain positive body language.
Positive body language can show the person that you’re listening and truly care. This includes maintaining comfortable eye contact, sitting down instead of standing, sitting alongside and angled toward the person rather than directly opposite him or her, and maintaining an open body position.
- Recognize cultural differences.
If you are helping someone from a cultural background different from your own, you might need to adjust some verbal and nonverbal behaviors, such as the level of eye contact or amount of personal space. Be prepared to discuss what is culturally appropriate and realistic for the person or seek advice from someone from the same cultural background before engaging with him or her.
End Quote
Looks like good stuff, right? I think it’s worth the effort to check the site out. Before you do that, let’s go through an example of the ALGEE action plan at work.
ALGEE for a Major Depressive Episode
A- Assess and Approach
Major Depression Signs and Symptoms
According to the Mayo Clinic Website
Quote
Although depression may occur only once during your life, people typically have multiple episodes. During these episodes, symptoms occur most of the day, nearly every day, and may include:
- Feelings of sadness, tearfulness, emptiness or hopelessness
- Angry outbursts, irritability, or frustration, even over small matters
- Loss of interest or pleasure in most or all normal activities, such as sex, hobbies, or sports
- Sleep disturbances, including insomnia or sleeping too much
- Tiredness and lack of energy, so even small tasks take extra effort
- Reduced appetite and weight loss or increased cravings for food and weight gain
- Anxiety, agitation or restlessness
- Slowed thinking, speaking, or body movements
- Feelings of worthlessness or guilt, fixating on past failures or self-blame
- Trouble thinking, concentrating, making decisions, and remembering things
- Frequent or recurrent thoughts of death, suicidal thoughts, suicide attempts, or suicide
- Unexplained physical problems, such as back pain or headaches
For many people with depression, symptoms usually are severe enough to cause noticeable problems in day-to-day activities, such as work, school, social activities, or relationships with others. Some people may feel generally miserable or unhappy without really knowing why.
Depression symptoms in children and teens
 Common signs and symptoms of depression in children and teenagers are similar to those of adults, but there can be some differences.
Common signs and symptoms of depression in children and teenagers are similar to those of adults, but there can be some differences.
In younger children, symptoms of depression may include sadness, irritability, clinginess, worry, aches and pains, refusing to go to school, or being underweight.
In teens, symptoms may include sadness, irritability, feeling negative and worthless, anger, poor performance or poor attendance at school, feeling misunderstood and extremely sensitive, using recreational drugs or alcohol, eating or sleeping too much, self-harm, loss of interest in normal activities, and avoidance of social interaction.
Depression symptoms in older adults
 Depression is not a normal part of growing older, and it should never be taken lightly. Unfortunately, depression often goes undiagnosed and untreated in older adults, and they may feel reluctant to seek help. Symptoms of depression may be different or less obvious in older adults, such as:
Depression is not a normal part of growing older, and it should never be taken lightly. Unfortunately, depression often goes undiagnosed and untreated in older adults, and they may feel reluctant to seek help. Symptoms of depression may be different or less obvious in older adults, such as:
Memory difficulties or personality changes
Physical aches or pain
Fatigue, loss of appetite, sleep problems, or loss of interest in sex — not caused by a medical condition or medication
Often wanting to stay at home, rather than go out to socialize or do new things
Suicidal thinking or feelings, especially in older men
End Quote Source: https://www.mayoclinic.org/diseases-conditions/depression/symptoms-causes/syc-20356007
Caregiver action
Look for changes in your resident that just don’t seem to go away by themselves or keeps popping up on a regular basis. Remember you are not trying to diagnose, just suspect that something is happening. Once an In-Home caregiver becomes aware of the symptoms, it is time to increase your protective vigilance. The resident is not in their right mind and is more susceptible to thoughts of self-harm or suicide ideation as a coping mechanism. Look for unexplained bruises or cuts, trying to obtain instruments of self-harm, or developing a plan to commit suicide.
Suicide Assessment
People with major depression are at greater risk of suicide. Females attempt suicide at three times the rate of men, but men are more likely to succeed. Those who have chronic illness or are older white males are at greater risk statically.
Caregiver action
Listen for phrases like “I can’t see things getting any better”, or “I feel trapped, hopeless and all alone”. If a person has been really depressed, then suddenly feels calm and relieved, they may have resolved to go ahead and attempt suicide. If you have any suspensions, then privately have a talk with the resident. There are caregivers who may fear that talking about suicide may instill the idea in the mind of the resident. Extensive clinical studies have proven that this is not the case. The opposite actually happens. Having someone listen nonjudgmentally provides a space to work through their suicide crisis. Being able to talk about it is a much better coping mechanism. Calling a suicide prevention hotline or calling 911 and asking for help with a potential suicide victim is always an option.
L- Listen nonjudgmentally
Caregiver action
Even if there is no danger of suicide, this is the time to take the depressed resident to a quiet place and have a good talk. And for the In-Home caregiver, I really mean to have a good listen. Use all the techniques previously mentioned in this course, and for heaven’s sake, don’t try to be the therapist/doctor if you suspect a case of major depression. Get the ball rolling by asking questions like:
- I have noticed lately that (List observed symptom(s) ). How long have you been feeling this way?
- I noticed that you haven’t been feeling like yourself lately, want to talk about it?
- Tell me about how you’ve been feeling lately.
- Is there anything wrong?
- Do you need to get something off your chest?
Can you see that this is a much better approach than trying to solve problems from the get-go? It allows the resident to blow off steam and you get to be the caring caregiver hero.
G- Give guidance and reassurance
Someone suffering through a major depression episode has their perceptions of their situation distorted by their condition. It is really hard for them to see things as they really are. They have withdrawn within themselves and are left alone with their negative thoughts. They are caught in a spiraling downward cycle, where their negative thoughts tend to reinforce their distorted perceptions. Also having removed themselves from others, there is no one there to push back against the downward trend. But now, they have you. You have just let them vent their build-up negative emotions. You haven’t shamed them or told them to snap out of it (that would only reinforce their negative thoughts.) Now is a good time to push back against their negative perceptions with a good healthy dose of positive facts. Tell them the things that will bring them hope.
Caregiver action
Every conversation will be different so there are no perfect responses. You will have to rely upon your own people skills to successfully get through this step. But having said that, here are a few suggestions that I would make if I were in your shoes.
- It’s the condition, not you, that is causing the issue.
“I totally get why you are feeling this way. But consider that feeling blue clouds your view of how things really are. It is like your mind has placed blue-colored sunglasses over your eyes. It’s hard to see the rainbow of colors all around you. Let’s work on removing those blue blinders.
- You are not alone.
It must be lonely where you are right now. It’s hard to face all this by yourself. But now you don’t have to. I’m here to help. You don’t have to face this by yourself anymore. I’ve got your back, Jack. Let’s see now, what do WE do first?
- Copying Chemicals
Everyone’s mind puts out copy chemicals that help them deal with the pressures and stresses of life. I see that you are running on empty right now. Either your mind is not producing enough copying chemicals, or you are using them up too fast. Let’s see if the doctor has something that will help you catch up on your supply.
- The situation has changed
I see that events have conspired against you lately. But all that has changed now. I am aware of your situation now and together we can change things. It’s time to call in the calvary. I know some people who can help.
- It’s not you that is talking, it’s the depression.
I know that you are a good person. I can sense that about you. It must be the depression that is talking, not you. We need to work on putting a muzzle on the beast that is chewing on you right now. Once we get it under control, we’ll get you back to your real self.
You will notice I used empathy, lots of empathy. I also tried to separate the resident and the condition. Thus, I create the impression of a monster that we can slay. I also worked on explaining that there is a root cause to why they are feeling the way that they do that is outside their core self. Depending on how deep down the rabbit hole they have traveled, you might have to repeat the L and G steps multiple times. Remember the goal of this step is to provide hope and useful facts.
E – Encourage appropriate professional help.
As we discussed earlier, this is where Adult Foster Care providers will have to operate differently than other mental health first-aiders. You are in charge of getting them the appropriate medical help they need. You will have to help them navigate through the medical system and past the insurance roadblocks. It will be important for you to record your observations and your suspicions and get them to the doctor, especially if you can’t be with them at the doctor’s office. All of that can be included in your patient files that you send with the resident.
The resident still has the right to refuse therapy, so you will have to use your caregiver skills to gain their cooperation. Don’t take it for granted that they will be cooperative.
A final thought on the subject. It will be important for you to review the medication to see if they are already on any anti-depressants. If they are and they still are getting depressed, then you might have to ask the doctor if a change is required or if a recent addition to the medication list is interfering with therapy.
E – Encourage self-help and other support strategies.
Some of the major factors in achieving full remission from a major depressive episode are the support that you can give and adherence to their therapy. Just by living in your well-ran and supportive adult foster care home is a huge leap forward toward recovery. You will ensure that they are following their therapy and seeing the doctor as often as needed. But be prepared. Once they have recovered enough to feel normal, it is natural for them to want to get off therapy. Sometimes they can get off therapy but more often than not, stopping therapy leads to a relapse. Lean heavily upon the doctor to decide if therapy can be discontinued. But- it also doesn’t hurt to bring up the subject with the doctor occasionally. It also doesn’t hurt to remind the resident that it is living in your home that is making the difference in their recovery. A final thought on the subject. You can recruit and coordinate other sources of support for the resident. Family members, support groups, online resources, and the like all can be utilized as tools in your caregiving toolbox.
Conclusion
I hope you can see why I thought you could benefit from a CE course about Mental Health First Aid. I think it’s pretty good stuff. The systematic way it untangles difficult behavioral issues is a really good caregiving technique.
- It helps you suspect that the behavioral problem may have its roots in an actual mental illness.
- It helps keep the residents safe and reduces the amount of work that you do. (less flopping around and spinning your wheels)
- It makes you more effective in resolving issues.
- It helps you focus on what the real problem is.
- It makes you more effective at getting the resident to the appropriate therapy they need.
- It makes your follow-up efforts much more effective.
I also have enjoyed showing you specific In-Home caregiver responses that you can use. You don’t often get this type of Adult Foster Care Provider focused actions from other sources. I hope you found them useful.
If you would like to see more material on this subject go straight to the source. https://www.mentalhealthfirstaid.org/
As always, good luck in your caregiving efforts.
Mark Parkinson BsPharm
Exam Portal
click on [Take Exam]
Purchase membership here to unlock Exam Portal.
|
|
|
|
|
*Important*
Registration and login is required to place your name on your CE Certificates and access your certificate history.
Username MUST be how you want your name on your CE Certificate.