TENS Units- An Electrifying Topic of Caregiving
TENS Units- An Electrifying Topic of Caregiving
Author: Mark Parkinson BsPharm: President AFC-CE
Credit Hours 1 - Approximate time required: 60 min.
Educational Goal
Tell Adult Foster Care Providers what TENS unit is and how to use it.
Educational Objectives
- Tell what Transcutaneous Electrical Nerve Stimulation therapy is.
- Instruct how to use a TENS unit.
- Discuss using the TENS unit in AFC home settings.
Procedure:
Read the course materials. 2. Click on exam portal [Take Exam]. 3. If you have not done so yet fill in Register form (username must be the name you want on your CE certificate). 4. Log in 5. Take exam. 6. Click on [Show Results] when done and follow the instructions that appear. 7. A score of 70% or better is considered passing and a Certificate of Completion will be generated for your records.
Disclaimer
The information presented in this activity is not meant to serve as a guideline for patient management. All procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this article should not be used by care providers without evaluation of their patients’ Doctor. Some conditions and possible contraindications may be of concern. All applicable manufacturers’ product information should be reviewed before use. The author and publisher of this continuing education program have made all reasonable efforts to ensure that all information contained herein is accurate in accordance with the latest available scientific knowledge at the time of acceptance for publication. Nutritional products discussed are not intended for the diagnosis, treatment, cure, or prevention of any disease.
TENS Units- An Electrifying Topic of Caregiving
Recently my wife had to use a TENS unit as part of her physical therapy for an injured shoulder. It brought back memories of when I first had to deal with a TENS unit as a caregiver many years ago. I thought, what’s a TENS unit? How do I operate the dumb thing? How much does it cost? Is it dangerous to operate? Is it worth the effort? Let me tell you about what I found out.
What is a TENS unit?
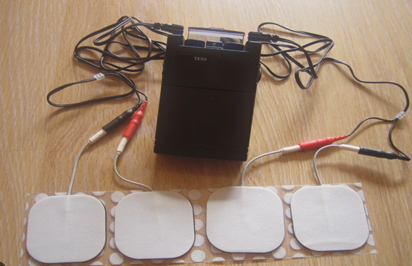
A TENS Unit is a small mobile electrical device about the size of a cell phone used for pain relief. It has wires that connect to electrodes embedded in pads that are attached to the skin. The device sends a small electrical current via the electrode wires into and through the area of pain. It is powered by a 9-volt battery system. The batteries are either replaceable or rechargeable.
How does it work?
 TENS stands for Transcutaneous Electrical Nerve Stimulation. (Transcutaneous means applied across a depth of skin).
TENS stands for Transcutaneous Electrical Nerve Stimulation. (Transcutaneous means applied across a depth of skin).
As the name implies, the device is designed to send a small electrical current from one pad to another through the skin. The exact method of pain relief is currently not known. It is believed to be one or a combination of the following.
- Blocks pain nerve signals from reaching the brain. The brain has only a limited supply of nerves that signal pain. The electrical impulse sensation occupies many of the nerves that otherwise would be sending pain sensations.
- Sends a counterirritant signal to the brain. The brain is distracted away from the pain sensations. Something similar to rubbing a banged elbow.
- The electrical impulse stimulates the release of endorphins. They are hormones that your body produces to relieve pain, reduce stress, and improve your mood.
Side Effects?
Used as directed, TENS therapy is tolerated quite well. The only significant side effect that has been reported is minor skin irritations at the site of the pads. There are cases though where the TENS therapy would potentially cause harm.
Contraindications:
- The patient already has an implanted electrical device, like a heart pacemaker or insulin pump.
- Has metal implants.
- Used during pregnancy.
- Epilepsy
- Has a malignancy (Cancer).
- Deep vein thrombosis
- Avoid the areas of the face and head, front of the neck, front of the chest, anywhere internally, over tumor or malignancy, directly on the spinal column, or around open wounds
Does it Really Work?
The use of electricity for pain relief dates back to ancient Rome and Egypt. Patients were told to step on electric eels in water. TENS therapy is an “add-on” therapy because it will not eliminate pain by itself. It just reduces how intensely it is felt. It does not heal the injury either, so its effect is only temporary. Unfortunately, there are those who receive no significant reduction in pain at all. One video made by a pair of physical therapists I saw claimed only about 50% of patients received benefits from the use of a TENS unit. In 2009 The American Academy of Neurology published guidelines for TENS unit use that stated that the TENS therapy was not effective in chronic lower back pain but was effective in diabetic neuropathy. My wife said the TENS unit helped her with her post-surgery shoulder pain.
Does Insurance Cover the Cost?
 As of the writing of this article, TENS units cost between $20 to $70, with some fancier models going for as much as $125.00. They are available for purchase online or at a medical equipment store without the need for a prescription. You also can rent a device from a medical supply store. Having said that, will insurance pay for a TENS unit? Not automatically. Each insurance policy is different. There are going to be some hoops and loops to jump through. At the bare minimum, a prescription will be required. I recommend that you go through a medical supply store and let them handle the details. If that is not an option, call the help desk number on the insurance card and ask them how you get reimbursed if you pay for the unit yourself. The website CAREX.com says,
As of the writing of this article, TENS units cost between $20 to $70, with some fancier models going for as much as $125.00. They are available for purchase online or at a medical equipment store without the need for a prescription. You also can rent a device from a medical supply store. Having said that, will insurance pay for a TENS unit? Not automatically. Each insurance policy is different. There are going to be some hoops and loops to jump through. At the bare minimum, a prescription will be required. I recommend that you go through a medical supply store and let them handle the details. If that is not an option, call the help desk number on the insurance card and ask them how you get reimbursed if you pay for the unit yourself. The website CAREX.com says,
Quote
Generally, the criteria for getting a TENS unit covered by insurance are the same. Here are the basics: TENS therapy must be deemed medically necessary and effective in treating the primary health issue – in this case, pain. For TENS therapy to be deemed medically necessary, patients must undergo a 30-day trial of transcutaneous electrical nerve stimulation treatment, preceded by a reassessment of the symptoms.
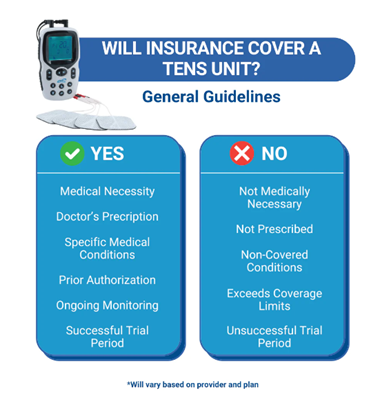 The post-trial reassessment of the patient’s pain-related symptoms must indicate:
The post-trial reassessment of the patient’s pain-related symptoms must indicate:
-
- The frequency with which the TENS unit was used during therapy and the average duration of use during each therapy session.
- The effectiveness of TENS in relieving the patient's pain-related symptoms.
In addition, the following criteria need to be met:
-
- The pain has been unresponsive to conservative medical therapy for a minimum of 3 months; AND
- The trial occurs under the direct supervision of a medical professional.
Continued use of the TENS unit will be deemed medically necessary for the treatment of pain if the following criteria are met:
-
- The TENS unit was used throughout the initial TENS therapy trial.
TENS therapy, including the TENS unit, will not be covered if:
-
- TENS therapy is not deemed medically necessary.
- TENS therapy is only deemed necessary for post-operative pain, not for acute pain.
- TENS therapy is being used to treat non-pain-related conditions, such as dementia and headaches.
End Quote
Which is the Best?
I personally have no preferences for which brand is best though the insurance company or the prescriber may. If a physical therapist is involved ask them for a recommendation.
TENS Units and Adult Foster Care
TENS therapy is generally well accepted as a safe “add-on” treatment in pain management. It may or may not help, but it won’t hurt the patient either. The overly simplified justification for its use is “It can hurt so let’s give it a try and see if it helps. Thus, TENS therapy becomes a tool for In-Home caregivers to ask the doctor when regular methods are not effective enough in managing the resident’s pain levels. However, its use presents some challenges for AFC providers.
 TENS is therapy. You have to get a prescription from the doctor and write it in the MARS. If you go to a physical therapist (PT) and they suggest its use, then you have to go back to the doctor for the prescription. The PT may do that for you.
TENS is therapy. You have to get a prescription from the doctor and write it in the MARS. If you go to a physical therapist (PT) and they suggest its use, then you have to go back to the doctor for the prescription. The PT may do that for you.- Each TENS unit comes with easy-to-follow instructions, but it does take some skill. Does that mean you have to get a nursing delegation to operate a TENS unit? I don’t know. To be safe talk to your county home inspector to be sure. If the answer is Yes- you need a delegation. Ask the person who said you need a delegation if the PT can do the delegation training. If they say no to the PT remind them that PTs are considered the experts over and beyond nurses.
- Determining which setting to use on the TENS unit would be considered choosing a therapy. The PT would have to tell you which setting to use as part of the delegation training or the doctor would have to include that in the prescription. (Including it in delegation training is a whole easier to accomplish. But it would require a referral from the doctor to see a PT)
- The prescription will often say- UD- use as directed or PRN as needed. For AFC providers, UD means training required and PRN means PRN log entries required in the MARS.
- Remember to put all actions taken (referrals, delegation training, etc.…) in the resident’s file.
The Settings and Modes
The modes and settings of the TENS unit will be determined by someone else, but it does not hurt to know what they are talking about in advance.
Modes
Most TENS units come with a pre-selected group of settings called a mode.
For example:
Normal- The device sends out a pulse rate that is consistent and never changes.
Burst- The device sends out a burst of pulses with a break in between.
Modulation- The pulse rate cycles through several preselected settings.
Which mode is best depends on the type of pain and the goals of therapy. There is always an element of guesswork in determining the mode so be prepared to monitor for effect (PRN log) and report back to the PT or Doctor your observations.
Settings
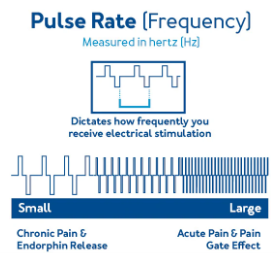
- Rate/Frequency- The flow of electricity comes in waves (measured in hertz). The pulse rate concerns how fast the waves come. It is also called frequency or how frequent the waves come. The higher the frequency the faster the waves.
Note- Low frequencies stimulate the release of endorphins and fast reacts interrupts pain signals to the brain.
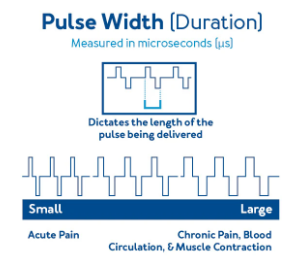
- Width/Duration- This is the measure of how long a pulse lasts. (in microseconds). The more extended the pulse time the stronger the stimulation is.
Note- Having high frequencies and durations may get too strong and become uncomfortable for the resident.
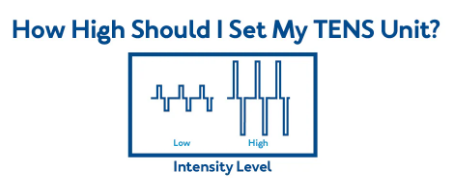
- Intensity- This is an indication of how strong the electric signal is (measured in microAmps). How strong the signal needs to be is also determined by guesswork. Normally you start low and then increase the amps until the desired effect is achieved. (titration)
Note- Titration should be part of the delegation training. I might also suggest you watch the body language of the resident for clues of effect. (blank face versus grimacing face). I also would suggest that you try the TENS unit on yourself to give an in-depth perspective on therapy.
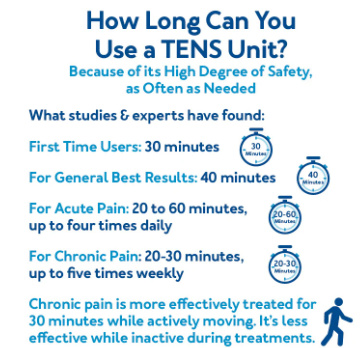
Unless the unit has automatic shut-off features, the duration of therapy sessions will have to be done manually. Because of how safe the therapy is, you can go for as frequently or as long as needed. (Timing is also determined by someone else, even if it is PRN). Here are some general guidelines as presented by an article in Carex.com
Note- The body can get used to stimulation. You may have to increase the therapy as you go for continued effect. Consult with the powers that be before doing so and include the action in your files.
A few More Caregiver Notes
- Do not use it while sleeping. You can’t feel pain while sleeping, so why use the device and get the resident desensitized to therapy?
- Turn the device off before removing or moving electrode placement. Failure to do so can result in the device “zapping” you.
- Remove the pads by peeling from the side. If you pull by the wires the connection will wear out sooner.
- The pads usually come sticky out of the package. To make the sticky last longer, remove oils from the skin before placement and or clean the pads with water after use. After removing the pads, place them back onto the plastic they came on originally.
- Replacement pads can be purchased, or you can Velcro the pads to a belt or sash. That may be caregiver convenient, but then you have to monitor for belt or sash slippage.
- Leaving the pads on between sessions may save some caregiving efforts but you will have to monitor the skin for redness and irritation.
- TENS Units can come with a clip that can be placed on a belt or clothing. Ensure the dangling wires are secured so they don’t catch on things. Also, the clip may come loose when going to the bathroom. Having the electronic device fall into the toilet is a bad thing.
- Hot or cold packs can be used on top of the TENS units. There may be some synergistic effects achieved. Ice may sensitize the skin.
- It doesn’t matter which wire goes to which pad, even if they are color-coded. The idea is to have the current flow through the painful area, from the sending to the receiving electrode. See pad placement.
 Decrease or stop therapy if the muscles start to twitch.
Decrease or stop therapy if the muscles start to twitch.
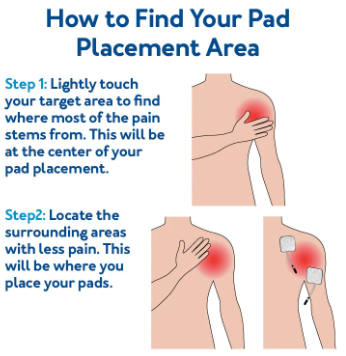
Pad Placement
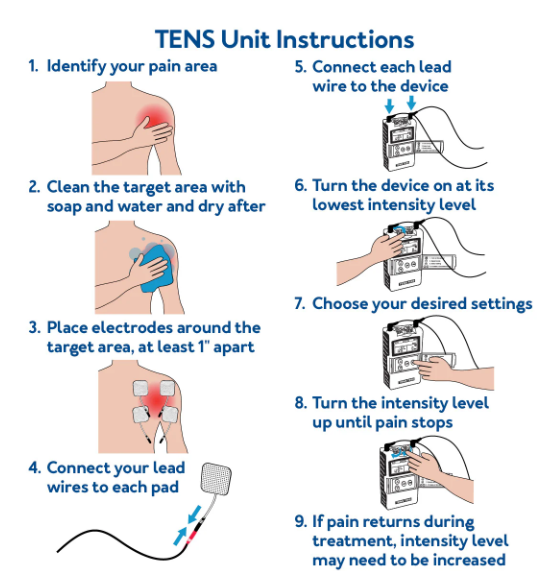
The ideal position for pad placement is going to be a matter of experimentation and adjustment. The PT will give you some directions on where to place the pads. If you forget, here are some general guidelines.
Overview of Instructions
#Source- https://carex.com/blogs/resources/how-to-use-a-tens-unit
For visual learners here are two YouTube videos I found, or you can do an internet search. Type in the search field - (your brand name), how to use, TENS. Watching is recommended but not required. There will be no exam questions on the videos.
Conclusion
Pain management especially chronic pain is one of the more difficult caregiving tasks that In-Home caregivers have to deal with. TENS units are another tool in your caregiver toolbox that you could call on to help your resident. It will take a prescription and training to use but often there is no other choice when pain meds aren’t enough.
As always, Good Luck in your caregiving efforts
Mark Parkinson BsPharm
References:
- Guideline: Widely Used Device for Pain Therapy Not Recommended for Chronic Low-Back Pain. American Academy of Neurology. https://www.aan.com/PressRoom/Home/PressRelease/784
- Brandon Landgraf. How To Get A TENS Unit Covered By Insurance. Carex.com. Nov 06, 2024 https://carex.com/blogs/resources/how-to-get-a-tens-unit-covered-by-insurance?srsltid=AfmBOopqhqN0dz5MZ36ABoF6dyEeVMikcbjdJ927EqFiZxX-Pc4TJ94r
- How to Use A Tens Unit. Drugs.com Dec 2, 2024. https://www.drugs.com/cg/how-to-use-a-tens-unit.html
- How to Use a TENS Unit. The University of Vermont Medical Center, Jul 2, 2019. https://www.youtube.com/watch?v=EB3d57MXtG8
- How to Use a TENS Unit for Back Pain 2024. Total Therapy Solution - Physical Therapy, Jan 19, 2023. https://www.youtube.com/watch?v=jcDvevu0MCI
- Tens Unit Training. Florida Sports & Spinal Reha, Jan 20, 2015. https://www.youtube.com/watch?v=h-fcSPozMxQ
- Transcutaneous Electrical Nerve Stimulation (TENS) For pain control. University of Washington Medicine. Apr 2016. https://healthonline.washington.edu/sites/default/files/record_pdfs/Transcutaneous-Electrical-Nerve-Stimulation-(TENS).pdf
- Brandon Landgraf. How to Use a TENS Unit. Carex.com July 07, 2023 https://carex.com/blogs/resources/how-to-use-a-tens-unit
Exam Portal
click on [Take Exam]
Purchase membership here to unlock Exam Portal.
|
|
|
|
|
*Important*
Registration and login is required to place your name on your CE Certificates and access your certificate history.
Username MUST be how you want your name on your CE Certificate.