What’s the Big Deal with Insulin
What’s the Big Deal with Insulin
Author: Mark Parkinson BsPharm: President AFC-CE
Credit Hours 3 - Approximate time required: 180 min.
Educational Goal
Provide instruction about the history and science of insulin and how to manage its administration.
Educational Objectives
- Tell the history of the discovery and development of insulin
- Explain the anatomy and physiology of insulin
- Instruction how to store, administer and manage synthetic human insulin.
Procedure:
Read the course materials. 2. Click on exam portal [Take Exam]. 3. If you have not done so yet fill in Register form (username must be the name you want on your CE certificate). 4. Log in 5. Take exam. 6. Click on [Show Results] when done and follow the instructions that appear. 7. A score of 70% or better is considered passing and a Certificate of Completion will be generated for your records.
Disclaimer
The information presented in this activity is not meant contraindications may be of concern. All applicable manufacturers’ product information should be reviewed before use. The author and publisher of this continuing education program have made all reasonable efforts to ensure that all information contained herein is accurate in accordance with the latest available scientific knowledge at the time of acceptance for publication. Nutritional products discussed are not intended for the diagnosis, treatment, cure, or prevention of any disease.to serve as a guideline for patient management. All procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this article should not be used by care providers without evaluation of their patients’ Doctor. Some conditions and possible
What’s the big deal with Insulin

You would be hard-pressed to find someone who has not heard of insulin. As an in-home caregiver, you probably know it as the stuff you have to store in the refrigerator and inject with needles. You also probably just had a shiver run down your spine and thought, “I hate needles. Just thinking about them gives me the willies.” So why the refrigerator and the needles? (shiver again) Why can’t they just take a pill like normal sick people? What’s the big deal with insulin and all the blood and poking stuff?
Insulin is simple to understand but very complex in how it is used by the body. Insulin is a hormone produced in the pancreas. It is produced so that our body can utilize important nutrients we have digested. Without it, we die. If its use gets messed up in the body, we can get sick with a variety of illnesses and eventually die miserably. You're probably thinking, “Hey Budy, there’s way too much talk about dying and sickness … and needles (shiver). All this dark talk is making me nervous. Can’t you tone it down a bit? I wanted a CE course that is a bit more on the entertainment side”.
Okay, let’s switch gears and talk about something more pleasant- history. I like stories about history.
Before the 1890s medical scientists didn’t know anything about insulin. They didn’t know how it worked. They didn't know where it came from. They didn't even know that they didn’t know anything. But they did know that certain children would suddenly get very thin and sick. They would get very thirsty, have to go to the bathroom a lot, become very weak, be prone to infections, and get very skinny no matter how much they ate. And the oddest thing of all, their urine had a lot of sugar in it. I wonder how they found the sugar in the urine.
Oh yuck, don’t even think that. They wouldn’t have tasted it would they?
I just looked it up. They noticed that sugar ants were attracted to the urine. They named the disease after its odd sugar symptom, Diabetes Mellitus. In Latin, that means to siphon off sugar.
Meanwhile in Berlin, in 1869 a medical student by the name of Langerhans noticed clumps of special cells in the pancreas. Today we call them the “Islets of Langerhans”. Langerhans didn’t know what the cells did but later Edouard Laguesse suggested they might have something to do with digestion. In 1889 Dr Oskar Minkowski wanted to test the idea so he removed the pancreas from a dog to see what would happen. (They had different ideas about animal rights back then.) The dog started to get the same Diabetes Mellitus symptoms as the children, thus confirming Laguesse's suggestion. The medical profession had started to close in on the idea of insulin.
Well, scientists knew something in the pancreas was helping but didn’t know what to look for. There were lots of doctors grinding up the pancreas and giving them to patients with no success. You see the pancreas also creates digestive enzymes as well. When you use the whole pancreas, you’re giving the patient way too many digestive enzymes. It caused extreme nausea and didn’t help the diabetes symptoms all that much.
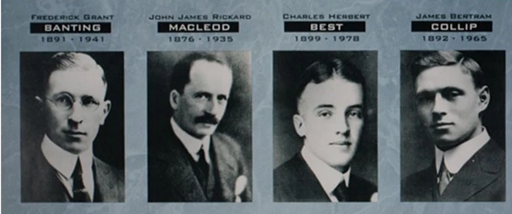
Then World War I happened. (Wars tend to sidetrack everyone’s attention). After the war around 1920 Canadian Fredrick Banting (a trained surgeon) wanted to explore Laguesse’s ideas. He guessed that the islet of Langerhans was the key. He had to separate it from the rest of the pancreas and extract what it was producing. Sounds complicated right? It was, and he needed help in doing so. He went see to Professor John Macleod of Toronto University in hopes that he would help in doing the research. Macleod was skeptical of this surgeon. He didn’t have any training in how to do research. Finally though, he did agree to help and gave him some unused lab space for the summer and an assistant, Charles Best, a student as a helper.
In 1921 Banting and Best were able to extract a chemical soup from a healthy dog’s islets of Langerhans in its pancreas and inject it into a Diabetic dog, and it worked. Within an hour the sugar levels in the urine dropped by 40%. Macleod saw they had something there and he gave them a better lab and more funds and told them to try to repeat the success. Science is getting closer to insulin now.
Banting and Best started to have success but was having a lot of trouble working with the canine Islet of Langerhans. The dogs kept dying and they were running out of dogs. Over 400 died during the experiments. Seeing they were having some difficulties with the chemistry, Macleod gave the team a biochemist James Collip to help with the chemistry stuff. The team switched to calf’s pancreas, which was easier to obtain, and the pace started to pick up. Collip had the expertise to go from extracting the islets of Langerhans soup to isolating the insulin in it. So now we have the idea man (Banting), the research helper (Best), the money and organization boss (Macleod), and the chemistry guy (Collip). They were able to extract and isolate enough of the stuff that was starting to be called insulin to have a human trial.
On January 11, 1922, Leonard Thompson, a 14-year-old diabetic who lay dying at the Toronto General Hospital, was given the first injection of insulin. And it worked, sort of. The injection he was given came from the extracts Banning and Best had done. That means dog insulin. His symptoms got better (yahoo) but he had a severe allergic reaction (boo). Too much dog in the dog extract. Very close but not quite there yet. They knew they were in the ballpark but needed a purer batch.
So Collip went back to the lab and worked day and night to isolate a purer batch. This time no allergic reaction. Hoorah, a cure for Diabetes Mellitus. No more kids dying horrible deaths. Insulin was now ready to help all those unfortunate kids. Yah….no. There was no way a college lab and one biochemist were going to isolate enough insulin for a bunch of test patients let alone thousands of desperate parents clambering for the new miracle drug. Oh so close, but still a swing and a miss.
Macleod arranged for Collip to set up shop in the Canadian government-owned Connaught Labs. Finally, enough insulin was purified from cow pancreas….. for just a few test subjects only. Also, Banting, Best Macleod, and Collip started arguing a lot about who was going to get the credit for insulin’s discovery. Collip got fed up and left. Another swing and a miss. No score yet.
Eli Lilly a pharmaceutical company in Indiana heard about the project and volunteered to help. Everyone agreed. Eli Lilly switched to pig pancreases, set up the purification process to produce in bulk, and things were set for mass production. Yah….no (again). You see, Eli Lilly shelled out big bucks to get the ball rolling and wanted the patent on insulin. They wanted to protect their future profits from their investments. Banting and Macleod had a hard time sharing control of the insulin project amongst themselves. They weren’t going to let anyone else butt in. So they didn’t cooperate with the patent thing. They also wanted to keep insulin as cheap as possible so that everyone could afford it.
patent thing. They also wanted to keep insulin as cheap as possible so that everyone could afford it.
There’s the pitch, the batter swings and …..foul ball. No score yet.
Finally, the Banting-Mcleod team applied for a patent so no one else could. They gave the patent to the University of Toronto for 1 dollar, so that insulin would stay cheap. Eli Lilly filed for patents on some of their manufacturing processes and insulin was being produced for the masses. There’s the pitch, the batter swings and grazes the ball. It dribbles into the outfield and the runner gets on base. No score yet.
“What!?!, you gotta be kidding me”, you say. This is getting ridiculous. The problem that is preventing a homerun score is, that the insulin that is being isolated is either pig or cow insulin, not human insulin. There are slight differences. That means the possibility of allergic reactions and problems with matching human insulin’s effects. But at least we’ve got something that works, right? Yes, solid base hit.
Fast forward in time a few decades and several medical and manufacturing advancements. (Too many to mention) Science has figured out how to get E. coli (the bacteria that gives us food poisoning) to produce insulin. It is the closest thing yet to human-made insulin. I mean, come on. That’s so cool! Tricking a deadly bacterium to be an insulin factory for us. We have switched from isolating animal insulin to manufacturing insulin. Science has also been able to map out all the molecules in insulin. Chemically they can dink around with it to produce insulin analogs that have specific effects. (like being long-lasting). They have even made a nasal spray version. So no needles are needed. The chemistry side of me is geeking out about it all. The base runner rounds third base and crosses home base. SCORE!!!. And the crowd goes wild….. sort of (again).
“Not again…. Now what’s wrong” you say. You see, it’s the cost. All that science stuff is really expensive and difficult. You try tricking bacteria to make something. It ain’t a cheap process buddy.
So the price of insulin products has soared in the last few years. Thank goodness for insurance, right? If they cooperate that is. When they don’t cooperate and deny the drug payments they’re about as bad as….. insulin needles (shiver).
So that’s a brief history of insulin. Easy to understand, but really complex and difficult in the details. How’s that for an entertaining CE? History stories, baseball analogies, and science all in one. Are we good now? Let’s keep on going. We’re moving on now to the anatomy and physiology of insulin in the human body. What, you thought we were done? Not by a long shot, baby. Insulin is too complicated a subject to fit into a short CE lesson.
Anatomy and Physiology of Insulin
The reason we produce insulin from the pancreas is to help us process glucose and some of the fatty stuff that results from the digestion of the foods we eat. Simple enough to understand but there are a lot of details that you need to know to truly understand what is going on. That greater understanding will help you react more appropriately when needed in your caregiving. Let’s get into the details of what insulin is, where it comes from, where it goes, and how it is used in the body. (sorry- no more history or baseball stories) Now wait a minute, I know you are probably thinking, “Ug this is going to read like a boring encyclopedia.” Give me a chance, you might be surprised by some of the scientific details about insulin.
What is Insulin
You’re probably used to thinking of insulin as a drug, but it’s actually classified as a hormone. What exactly is a hormone? By definition, a hormone is a substance that is produced in an organ that is transported around the body. It stimulates a chemical action that increases a bodily function. Another important detail is chemically, insulin is classified as a protein. “What do you mean, like meat?” you are thinking. Well, a protein is actually a sequence of amino acids that are strung together to form a larger molecule. Picture it as a long chain that is twisted up and it forms a certain shape. You see I told yah, surprising little details that will be important later on.
Where does Insulin come from
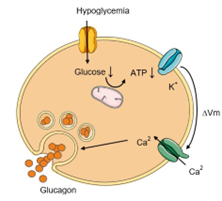
You already know that insulin is produced in the Islets of Langerhans in the Pancreas. The details that you don’t know yet are that there are several different kinds of cells in the islets of Langerhans. The important ones in insulin production are called the alpha and beta cells. The alpha cells produce glucagon, and the beta cells produce insulin. (More little details that will be important later on.) The islets of Langerhans only comprise about 1% of the pancreas. The rest of the pancreas is comprised of the acini tissue that produces enzymes and bicarbonates used in digestion. The important thing to remember is that there is only a small, limited supply of insulin-producing beta cells in the pancreas.
As you can imagine, insulin production is quite complex and involves several steps. The process ends with the insulin and other molecules being stored up in little bubbles called vesicles. When glucose concentrations are high, the vesicles are stimulated thru several more steps. It involves potassium and calcium that help fuse the vesicles to the beta cell's membrane wall and they “pop”, releasing the insulin into the bloodstream.
Where Does Insulin Go
A lot of blood goes thru the pancreas. The important direction of flow concerning insulin is that it comes from the small intestine loaded with nutrients like glucose and amino acids. Then the pancreas adds insulin to the mix and then the blood flows to the liver. In the liver, insulin has 4 times the effect as compared to other parts of the body. After the liver, the nutrient and insulin-rich blood flows to the rest of the body. It even crosses the blood-brain barrier into the central nervous system which includes the brain. Wherever nutrients are required, insulin goes along to help get the important stuff inside the cells where it is needed.
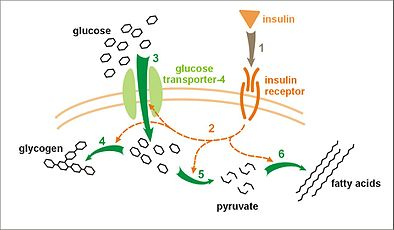
What Does Insulin Do
Think of insulin as a key that unlocks cellular doors. Around each cell, there is a membrane that keeps the important bits and chemicals from mixing with the chemical soup that surrounds it. If you want molecules to pass through the cellular membrane, you have to open channels that are designed to let that certain thing inside. Once that is done the channel closes so important stuff doesn’t leak out and unwanted stuff doesn’t leak in. One of the more important chemicals that we want in our cells is glucose, the primary fuel that powers the cell's workings. Insulin is the hormone that opens the glucose channels in the cellular wall. There are other chemicals that rely upon insulin to get into cells. For example, amino acids that the muscles use to build proteins are also insulin-dependent.
A few words about glucose. Glucose is a very reactive molecule. It easily combines with other molecules and tissues, and it messes things up. (Remember that fact when we talk about Diabetes). You don’t want a lot of excess glucose floating around but it’s too important to just flush it away in the urine with the rest of the body's waste products. Our bodies have two ways to convert the excess glucose into safer, easily stored molecules. The liver turns glucose into glycogen and the adipose cells convert glucose into triglyceride. You might know the triglyceride-packed adipose cells as your fat stores. When the body needs glucose and there’s not enough in the blood, the body breaks apart the storage molecules back into glucose.
How Does Insulin Work
Insulin not only is the key that unlocks cellular doors, but it is also a key that when inserted, starts certain cellular processes working. Things like producing cellular energy, making muscle material, and of course fat production. I will spare you all the complex details, but for those science nerds out there, the list of primary cellular processes is:
- Glucose uptake
- Lipogenesis
- Amino Acid uptake
- Glycolysis
- Glycogenesis
- Protein synthesis
The way that insulin does all these processes is complex but easily understood. There are certain structures within the cell wall that are called receptors. The insulin receptor has a part that extends outside the cell and a part that hangs inside the cell. The outside part has a pocket shaped so only insulin fits in it. When insulin floats near enough, it fits into the pocket. The receptor changes so that certain molecules fall off the end and float around on the inside of the cell. Those molecules in turn connect to the inner workings of the cell and the right cellular machinery starts up.
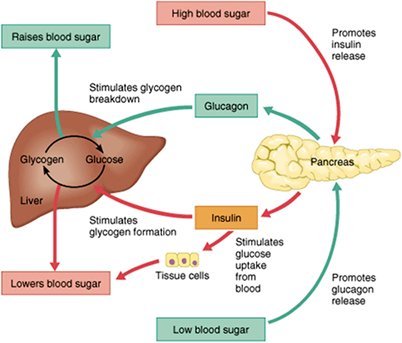
Any insulin-dependent activity that can be started up, needs to be able to be turned off as well. If you don’t, all the glucose will be used up. The “turn-off switch” is located back in the islets of Langerhans again. This time were dealing with the Alpha cells and a hormone called glucagon.
Glucagon does the opposite of insulin. It tells the liver to convert glycogen to glucose and the adipose cells to release and break up triglycerides into glycerol and fatty acids. Glycerol and the fatty acids can then be converted into glucose. In addition, glucagon can also tell muscles to break apart some of their proteins into amino acids. The amino acids can be turned into glucose as well. Finally, glucagon tells the beta cells in the pancreas to slow down the making of insulin. All of these processes make it easier to build up the concentration of glucose in the blood even if there is no food being consumed. When the concentration of glucose is high enough insulin production starts up again and glucagon production is inhibited.
The glucagon vs insulin is a balancing act based on a negative feedback loop. It happens automatically as part of the dynamic system we call homeostasis. It enables cellular machinery to adapt to the changing needs of the body. For example, you don’t need a lot of glucose fuel in the brain if it’s sleeping.
If this is getting to sound a bit too complicated, of course it is. Everything about insulin is always complex.
Don’t get too caught up in the details though because of course insulin is simple too. Keep your focus on the big picture. Glucose up, insulin up. Insulin goes into cells, and glucose and amino acids go into cells. Glucose in blood goes down and glucagon starts up, then insulin production is slowed down until the glucose levels are right again.
Diabetes and Insulin
You can’t talk about insulin without bringing up Diabetes. There are two versions of the disease. Type I is where the beta cells have all died off. Injecting insulin is the only option for treatment. In Type II the body is becoming insulin resistant. Insulin is being produced but the process is messed up somewhere. In the beginning of Type II the doctor can give some pills that help increase insulin effectiveness. You can also control glucose levels thru diet and exercise. If therapy fails, then insulin injections will probably be needed.
I think that you have had just about enough of me being a science nerd and sounding like an encyclopedia. I am going to mix things up a bit and show you a video about diabetes instead. It’s great to be shown what’s going on instead of reading about what’s going on. Warning there will be at least one test question on the video material.
Okay, we’ve had some history, baseball, encyclopedia stuff, and a video about diabetes. Let’s see, what’s left to cover… hummm. Oh yah, Drugs and Caregiving.
Caregiving and Insulin Drugs
The goal of insulin drug therapy is to regulate the body so there is a normal flow of blood glucose. The cells need to have enough fuel no matter what happens. But as you now know, blood glucose changes a lot throughout the day. It rises with each meal, it lowers after exercise, and it increases if there is a sickness. It’s enough to make your head spin. What does that all mean for the patient and their caregiver? It means there will be no easy “one size fits all” drug regime. No “one and done on the run”. You may even have two different types of insulins to inject at different times of the day. It is going to take a lot of monitoring and adjusting as you go.
Insulin therapy may be complex, but it is also easy to understand. The basics are you find out where the blood glucose concentration is at by doing a finger stick. Then you adjust the regime according to the doctors’ instructions and you’re done.
If the blood glucose doesn’t come under control, you notify the doctor and let them worry about changing the regime. There is even a surgically inserted insulin pump that does the monitoring adjusting and injecting automatically. For more information about diabetes management see my other CE lessons or contact the patient’s Diabetes care team.
Blood, injections, needles, Yikes! Why can’t there be some simple pills to take? Let’s talk about why there are no insulin pills. Remember, insulin is basically a complex protein. We can crystalize that protein and put it in a pill. We can even concentrate it down and store it in a capsule. That’s not the issue. The problem occurs when the insulin protein goes through the digestive tract. The body just digests it before it can reach the blood. Man-made insulin has to be delivered directly into the bloodstream for it to have any effect. For you needle haters, that’s a real bummer.
Alternatives to injectables
Recently several inhaled versions of insulin have been approved by the FDA. Yes! No needles. Unfortunately, they cost more than injectable insulins (a lot more). Insurances are not very cooperative about paying the extra cost. They see inhaled versions as more of a convenience than a therapeutic necessity. A swing and a miss. (more baseball jargon)
If you are thinking that the insulin pump thing sounds like an easy alternative to needles, you would be wrong. They also cost a lot more and require a lot of maintenance and expertise. There is also the constant danger of infections that reach the bloodstream fast.
A hit, but a foul ball- if the batter is an In-home caregiver.
Synthetic Insulins
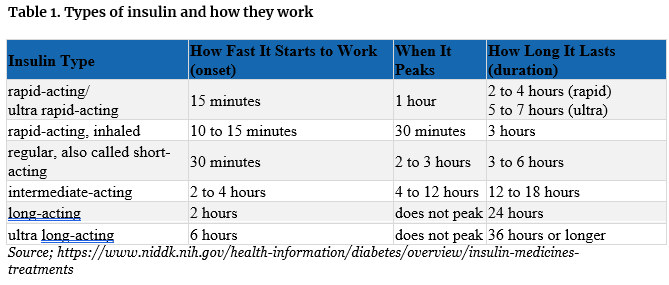
Now we have come back full circle and are ready to talk about the stuff you have stored in your refrigerator. Harvested and purified, bovine (cow) and porcine (pig) insulin is not used much anymore. I haven’t seen a bottle of it in decades. The stuff you’re used to seeing is manufactured. (remember the tricked bacteria thing). It is officially known as synthetic human insulin. It comes in several different types, all based on how fast you want the injected insulin to work. To understand what that means to your clients, it’s best if you know three different terms. They describe the timing of when the patient’s insulin prescription works.
- Onset -is the length of time before the insulin hits the bloodstream and begins to lower blood glucose.
- Peak- is the time when insulin is at its maximum effectiveness at lowering blood glucose levels.
- Duration -is the length of time the insulin continues to work at lowering blood glucose levels.
Here’s a table of the different types of synthetic insulins and how fast they work and for how long.
Basal and Pulse levels
So why all the complex variety? Because it’s insulin, of course, complex is its middle name. It’s also easy to understand if you know two factors of endogenous insulin production (natural insulin production in the body). Basel levels and pulse doses.
- Basal levels - As long as the cells of the body are alive there will be a need to send fuel to them. Even when you are asleep there are lots of cells working. To meet the constant need, the pancreas constantly has to produce insulin. That’s the base level of insulin concentration.
- Pulse doses- If cellular activity increases or food is eaten, blood glucose levels fluctuate. The pancreas is stimulated to send out extra insulin to take care of the fluctuations in blood glucose.
Diabetic insulin therapy regimens try to copy these varying endogenous levels by using different types of synthetic human insulins. Long-acting versions copy the basal level, while fast-acting is meant to copy the pulse doses. There are even prescriptions that have a mix of both short and long-acting insulins.
Do your job right
As an In-Home caregiver, your job is to monitor how drug therapies are working. That means keeping track of the good effects that are supposed to happen and the bad effects that might happen. You’re monitoring the drugs so that you can tell if you’re doing a good enough job of taking care of your paying customers. You’re also monitoring the drugs to tell the prescriber if his chosen therapy is doing what he expected it to do. If you are not actively pursuing this aspect of In-Home caregiving, I highly recommend that you change your business priorities. Those who just act like a glorified babysitter are being lazy. Lazy caregivers are ironically making their jobs harder because sick patients take more caregiving effort. Also, they lose paying customers faster than they ought to. If you want an easier more stable source of income, then monitor the drugs for effect and tell the doctor when things don’t go as anticipated, and do it quickly.
Goals of Therapy for Insulin
You can tell if the insulin therapy is doing what it’s supposed to do by paying attention to two measurements. Blood glucose concentrations and Hemoglobin A1C
Blood glucose concentration measurements are acquired from a blood sample. A drop of blood is placed on a test strip inserted into a blood glucose meter. The blood sample usually comes from poking the finger with a lancet device. The procedure is commonly called getting sugar levels from a finger stick, or just a finger stick.
Readings can vary depending on the time of day, the place where the blood is taken, the health of the patient, etc.… If it sounds complicated, of course it is, insulin is involved. It will be important to get some training from the doctor or diabetes educator.
In general, the Centers for Disease Control (CDC) states,
“A blood sugar target is the range you try to reach as much as possible. These are typical targets: Before a meal: 80 to 130 mg/dL.
Two hours after the start of a meal: Less than 180 mg/dL.”
Because of the variability of the finger sticks, doctors also take a Hemoglobin A1C test, A1C for short. I won’t go into the details because of course it’s complicated. According to the American Diabetes Association (ADA),
“The goal for most adults with diabetes is an A1C that is less than 7%.”
A good insulin prescriber will tell you what the treatment goals they are shooting for. If they don’t tell you, ask for them. (It will also make you look professional too). From then on, therapy management is simply comparing your individual reading to the goals set by the prescriber. I recommend that you keep a record of your finger sticks and send them with the patient whenever they see the doctor. Don’t worry so much about individual readings. There are always going to be “one-off” spikes in the readings. You’re looking for patterns over time. (Too low and too high) If you see any patterns developing, call the doctor.
Side Effects
Synthetic human insulin is pretty well tolerated with few side effects. There is always the possibility of an allergic reaction or infections developing. Look for lumps, pits, swelling, redness, or itching at the injection site. Rotating the injection site and finger stick location will help prevent tissue scarring from developing. There is also the real chance of the insulin working too good and crashing blood sugar levels (hypoglycemia). Always have a  sugary snack handy just in case. Look for:
sugary snack handy just in case. Look for:
- Fast heartbeat.
- Nervousness or anxiety.
- Irritability or confusion.
- Hunger
Finally, weight gain is always possible. You’ll have to take the residents’ weight from time to time and place the information in their records.
Storage and Dispensing Insulin
Why the refrigerator?
Insulin is a rather fragile molecule. It degrades fairly easily. If you shake the vial the molecules can break. If it gets too cold or freezes it can break. If it gets too hot, it breaks. Even at room temperature, it starts to degrade after 28 days. So, you have to store unused vials in the frig to keep the insulin fresh. Here is what that means to you as an In-home caregiver.
You have to store the insulin in a secured box in the fridge, just like the rest of the drugs you’re in charge of. The temperature of the area of the fridge you keep the storage box in has to be between 36°F to 46°F. A thermometer will have to be kept somewhere near the box. There are easy-to-read frig thermometers you can buy. No freezing of the insulin in the cold spots at the back of the frig, where the air circulation is bad.
The one vial that you’re giving the shots from has to be watched as well. You can’t store it in the sun or near a heater. Keeping it in a car is a no-no too unless it’s kept in a special insulated insulin storage device. They keep the insulin from getting too hot. You can buy those too, for when your insulin using resident goes on day trips or longer. You can’t keep the insulin in a coat pocket. It shakes too much. You can’t keep it in a shirt pocket. It gets too hot. They do make fanny packs specially built to carry insulin on the patient or caregiver.
If the resident has permission to self-inject, you have to have that in writing from the doctor. Keep the permission slip in your records and make copies when necessary. You also have to ensure that when the insulin is out of your control (like on trips, job sites, or in the resident’s room) the insulin is being stored properly or don’t give out the insulin at all.
Why, you ask? Two reasons;
- Broken insulin molecules are not insulin. They won’t fit into the insulin receptors and trigger the proper reaction. And those broken bits of “not insulin” floating around, who knows what they are going to do. Probably nothing, but I am not going to be the one responsible for finding out if that’s true or not.
- “Not insulin” molecules reduce the real insulin’s concentration so you’re not giving enough insulin at the time of injection.
You can tell if the insulin has gone bad by comparing it to a fresh vial. If the fresh insulin is clear, watch for floaties or color changes. Longer-acting insulin has ingredients added to make the insulin last longer. That makes the long-lasting insulin look cloudy and the particulates can settle out. Before using the long-acting insulins, you will have to gently roll the vial 10 times. Resist the temptation to shake the container. You can tell if these types of insulins have gone bad by color changes and the vial looks like frost is collecting on the inside of the containers. Each container of insulin has an expiration date printed on it. Throw away any expired or suspicious-looking insulins. Don’t take chances with the “not insulin” stuff.
Delivery Devices
 We’re not talking delivery by FedEx here. We are talking about vials of insulin, delivered via needles. (Shiver, Shiver). Oh stop that! It’s not that bad. Today’s insulin syringes are so fine (thin) that getting poked by one hurts less than pinching yourself. In fact, they are so thin that there is a danger of snapping off the needle in the skin if handled too ruffly. Then you have to go get it like you would a sliver of wood, with a magnifying glass and tweezers.
We’re not talking delivery by FedEx here. We are talking about vials of insulin, delivered via needles. (Shiver, Shiver). Oh stop that! It’s not that bad. Today’s insulin syringes are so fine (thin) that getting poked by one hurts less than pinching yourself. In fact, they are so thin that there is a danger of snapping off the needle in the skin if handled too ruffly. Then you have to go get it like you would a sliver of wood, with a magnifying glass and tweezers.
Insulin prescriptions come in multi-use vials. Each vial has a rubber stopper where you insert the needle. Then you hold the vial straight up and draw out the proper dose. Keep the tip of the needle out of the air space to prevent drawing up bubbles.
Drug Manufacturers also make multidose insulin devices that look like a pen. Except there is insulin instead of ink and you have to screw on the needle. (Good, you didn’t shiver that time). The pens are more expensive, but they are easier because you don’t have to draw up insulin from a vial. They are especially handy for those residents who take insulin when you’re not around to supervise them. If you can’t quite visualize all of this, don’t worry. I’m going to post videos of what this all looks like at the end of the lesson.
The final thing you have to worry about as an In-home caregiver is what to do with the needles and the lancet blades after  you are done with them. Legally you have to place them in a red sharps container or a thick-walled plastic jug, like an empty laundry soap container. You then have to properly dispose of the sharps container with the garbage service. Just to warn you it’s going to cost more. Call the garbage company for details. You can make the sharps containers last longer and reduce disposal costs by putting just the screw-on needles, the lancet blades and the needle portion of the syringe into the sharp’s container. The rest of the syringe can be thrown out with the regular garbage.
you are done with them. Legally you have to place them in a red sharps container or a thick-walled plastic jug, like an empty laundry soap container. You then have to properly dispose of the sharps container with the garbage service. Just to warn you it’s going to cost more. Call the garbage company for details. You can make the sharps containers last longer and reduce disposal costs by putting just the screw-on needles, the lancet blades and the needle portion of the syringe into the sharp’s container. The rest of the syringe can be thrown out with the regular garbage.
Conclusion
Well that’s that then. You’re all ready to go aren’t yah? Not so many worries now and no shivering, right? Good good, I know you can do it. After all, you are a professional and now know quite a bit about insulin and how to deal with dispensing it. Also, take comfort that you are an important part of a diabetes care team. If you are still unsure of the details, lean on the other members of the team for support. Ok, are we good now? That’s excellent. Here are the links to the videos I promised. There will be test questions.
Insulin Administration Videos
For this video you have to visit AARP website. Click on the image or link - Once you are done click on the back arrow in the top light hand coner of you computer
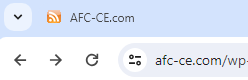
Managing Medications: Administering Insulin Injections
For the following videos just click on the arrow in the picture.
How to Inject Insulin with a Pen and Pen Needle
How to Inject Insulin with a Syringe
As always Good Luck in your caregiving efforts.
Mark Parkinson BsPharm
References:
- Clevland Clinic.org. Oct/23. https://my.clevelandclinic.org/health/articles/22601-insulin
- Wikipedia the Free Encyclopedia https://en.wikipedia.org/wiki/Insulin
- The Discovery of Insulin, The Miracle- Part 1. Extra History. Nov 18, 21
https://www.youtube.com/watch?v=Qs_QCJv3HrA&t=523s
- Banting's Miracle Drug. World Collaborative. May 8, 18
https://www.youtube.com/watch?v=kVG7xlY7xVg
- How insulin works. Novo Nordisk insulin-containing products. Aug 2, 18
https://www.youtube.com/watch?v=HJGjNTJgf48
- Endocrinology Pancreas: Insulin Function. Ninja Nerd. Medical Lecturers. May 11, 17. https://www.youtube.com/watch?v=w4jHtPUNg6E&t=7s
- Philip Newsholme, Vinicius Cruzat, Frank Arfuso, Kevin Keane. Nutrient regulation of insulin secretion and action. Journal of Endocrinology. Volume 221: Issue 3. Jun/14. https://joe.bioscientifica.com/view/journals/joe/221/3/R105.xml
- Diabetes Mellitus | Type I and Type II Diabetes Mellitus. Ninja Nerd. Medical Lectures. Apr 22, 20. https://www.youtube.com/watch?v=-axOMKLkLLQ
- Endocrinology | Pancreas: Glucagon Function. Ninja Nerd. Medical Lectures. May 11, 17. https://www.youtube.com/watch?v=b2Kcp5hJBXE
- Amy Hess-Fischl, E.Lisa Jaffe. What Is Insulin? com. Feb 15, 22. https://www.healthcentral.com/condition/type-1-diabetes/what-insulin
- Insulin, Medicines, & Other Diabetes Treatments. National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Oct/22https://www.niddk.nih.gov/health-information/diabetes/overview/insulin-medicines-treatments
Exam Portal
click on [Take Exam]
Purchase membership here to unlock Exam Portal.
|
|
|
|
|
*Important*
Registration and login is required to place your name on your CE Certificates and access your certificate history.
Username MUST be how you want your name on your CE Certificate.
| Guest: Purchase Exam |