What’s the Deal with Potassium?
What’s the Deal with Potassium?
Author: Mark Parkinson BsPharm: President AFC-CE
Credit Hours 2 - Approximate time required: 120 min.
Educational Goal
Teach the basics of potassium metabolism.
Educational Objectives
- Teach about the importance and physiology of potassium.
- Provide a basic understanding about the pathophysiology of sodium.
- Teach caregiving techniques on how to manage blood potassium.
- Tell about potassium supplements and medications.
Procedure:
Read the course materials. 2. Click on exam portal [Take Exam]. 3. If you have not done so yet fill in Register form (username must be the name you want on your CE certificate). 4. Log in 5. Take exam. 6. Click on [Show Results] when done and follow the instructions that appear. 7. A score of 70% or better is considered passing and a Certificate of Completion will be generated for your records.
Disclaimer
The information presented in this activity is not meant to serve as a guideline for patient management. All procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this article should not be used by care providers without evaluation of their patients’ Doctor. Some conditions and possible contraindications may be of concern. All applicable manufacturers’ product information should be reviewed before use. The author and publisher of this continuing education program have made all reasonable efforts to ensure that all information contained herein is accurate in accordance with the latest available scientific knowledge at the time of acceptance for publication. Nutritional products discussed are not intended for the diagnosis, treatment, cure, or prevention of any disease.
What’s the Deal with Potassium?
What’s the deal with potassium? You have probably heard stories about the stuff and wonder just how important is it? More significantly, as a caregiver should you even care? What does it have to do with in-home caregiving anyway? Well, it turns out that potassium is very important for our bodies to function properly. And surprisingly, in-home caregivers have an unusual amount of control in its therapeutic application. But with the power to control comes the responsibility to act appropriately. Let’s give you that knowledge.
What is Potassium?
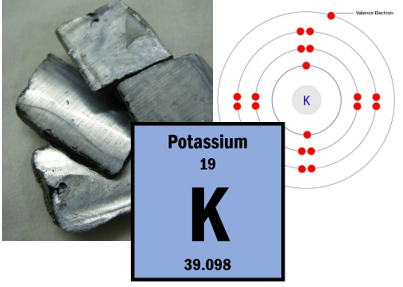
Potassium is a silvery-white metal that has the atomic number 19 and the chemical symbol K. It has several chemical properties that make it very useful to our bodies.
How is Potassium used by the body?
Potassium is an essential mineral used by every single cell of our body. It is also an important cofactor in several enzyme and membrane channel functions. Potassium keeps the heart pumping, the muscles contracting and relaxing, nerves firing and bowels digesting. Simply put without potassium our bodies would not function. The main reason why this occurs results from potassium’s positive change when dissolved in a fluid. This chemical property makes potassium an electrolyte.
An electrolyte is any material that breaks apart into ions (charged particles) in solution, making it capable of conducting electricity. For example, Potassium Chloride when placed in water will break apart into K+ and CL- ions. All the charged particles floating around create a pathway for the electricity to follow. The charge jumps from ion to ion.
That is how nerve signals are created and sent down nerve fibers in the nervous system. The nerve cell pumps sodium and potassium ions in and out of the cell membrane. Sodium has a greater charge than potassium thus creating a difference in electrical charge potential. By changing the balance between two ions the cell creates a charge potential pathway for the nerve signal to follow. After the signal is sent, the cell moves around the ions to “reset” the cell membrane for the next signal charge.
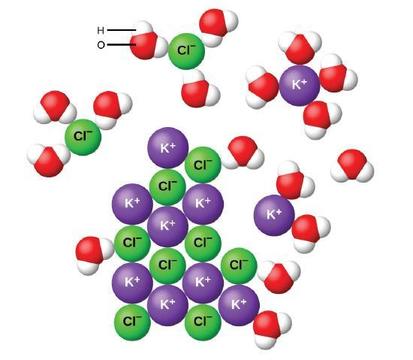 The ion charge also explains why water follows salt. Water molecules have partial magnetic poles. There is a potential weak positive and negative end to each water molecule. Throw in a positive potassium ion (K+) and all the negative ends of the surrounding water molecules will be drawn to it. The more K+ ions the greater the magnetic pull. That magnetic attraction is one of the main driving forces of water flow due to osmosis. If the body wants water to flow past a membrane it pumps salt ions past the membrane and the water naturally follows.
The ion charge also explains why water follows salt. Water molecules have partial magnetic poles. There is a potential weak positive and negative end to each water molecule. Throw in a positive potassium ion (K+) and all the negative ends of the surrounding water molecules will be drawn to it. The more K+ ions the greater the magnetic pull. That magnetic attraction is one of the main driving forces of water flow due to osmosis. If the body wants water to flow past a membrane it pumps salt ions past the membrane and the water naturally follows.
For example, when the body needs to cool off, it pumps the salt ions into the sweat glands and the water follows. The water then evaporates and cools the body. The salts remain behind creating a salty crust on the skin. It is also a major factor in how the kidneys function.
Keeping the right balance of the salt ions around the body and each individual cell is critical for proper bodily functions.
Storage and Control
Potassium is found throughout the body’s fluids. We will divide those fluid areas into three parts. Intracellular (within the cell), Interstitial (the spaces in between the cells), and blood plasma. Knowing the details and potassium concentrations are not that important for caregivers. What is important to know is that most of our potassium is stored in the intracellular space. If the cell needs some action done, it will pump out the potassium into the interstitial space through ion pump channels in the cell’s membrane.
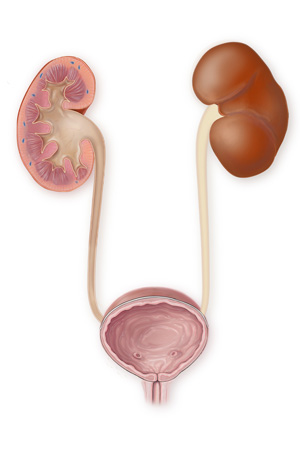
This potassium storage inside the cell is strictly controlled by the body’s homeostatic mechanisms. As potassium is lost (mainly through the urine) it is replaced from the foods we eat. If there is too much potassium around, the hormone aldosterone will make the body urinate more to get rid of the excess. If we don’t take in enough potassium in our diet, our kidneys will try to retain more potassium from the urine.
Of course, the potassium metabolism is a lot more complicated than what I just explained. Some significant concepts that I did not explain are:
- Potassium is also lost in sweat and feces.
- There are mechanisms that move potassium in and out of the individual cells.
- There is a strong relationship between potassium and the pH of bodily fluids.
The caregiving takeaway is potassium is so important to the body that it has multiple ways it takes care of it under normal conditions. So usually, the caregiver does not have to worry about potassium levels except for supplying a good diet. More about that later.
The Hyper and Hypo of Potassium
“Under normal conditions”, I bet you would love things to be normal. But if you are involved in taking care of someone else, things are not normal. In-home caregiving is all about striving to take an abnormal situation and getting as close to normal as possible. In-home caregiving is all about monitoring the patient and utilizing all the resources available to make things right when things seem to go wrong.
When things go wrong
Interesting fact- Potassium was originally called kalium. That is why potassium’s chemical symbol is K and why disorders involving potassium often have "kal" in their names.
A caregiver can count on the body to take care of its own potassium stores and balances. But some things can with interfere potassium homeostatic mechanisms. Fortunately, In-home caregivers do not have to diagnose the problem or find ways to remedy the situation. That is the doctor’s worry. Your worry is to look for the signs and conditions that will lead you to suspect there is a problem. Then you push the medical system until your worries are relieved or the problem is being treated. The trick is to know what to look for.
Too Much Potassium
Determining how much potassium is in the cell and interstitial spaces is just too hard. That leaves monitoring how much potassium is in the blood. Not the ideal way to monitor for problems but it’s the best we got.
If there is too much potassium in the blood, then the patient has Hyperkalemia. I love medical terminology. Just knowing how a word is put together tells you what is going on.
- Hyperkalemia
- Hyper= too much
- kal= potassium
- emia= pertaining to the blood
Yeah I know, I’m a nerd for getting excited about such things.
What caregivers should look for to suspect Hyperkalemia
The symptoms of hyperkalemia are:
- Weakness and fatigue
- Nausea and vomiting
- Shortness of breath
- Chest pains
- Heart palpitations and irregular heartbeats
- A burning or prickling sensation in the extremities
I know what you are thinking. Those signs are pretty general and could be caused by a lot of conditions. To make things more complicated many times the patient will be asymptomatic (without outward signs of symptoms) until the problem is very severe. How can caregivers narrow things down a bit? You don’t want to be the one who cried wolf too many times.
As I said earlier, you can count on the body to take care of itself regarding potassium levels. It’s only when the body’s homeostatic mechanisms are messed up that caregivers should start being concerned about the signs and symptoms of too much potassium.
Who is at risk for Hyperkalemia?
So when do you start to worry about hyperkalemia? It’s all about those who are having problems being able to pee and those who take drugs that affect potassium levels. The kidneys and the adrenal gland which makes the hormone aldosterone are key potassium control organs. For those with chronic kidney disease or adrenal insufficiencies, caregivers will have to monitor for the signs of hyperkalemia. Contact the primary care physician for this info.
Medical science has learned how to manipulate how to body uses water to reduce blood pressure. The drug classes ACE inhibitors (angiotensin-converting enzyme inhibitors), ARBs (angiotensin receptor blockers), or potassium-sparing diuretics all can lead to too much potassium. Read the drug information sheets that come with the prescription or just ask the pharmacist.
Those with uncontrolled diabetes (especially type 1), congestive heart failure, and liver disease should also be monitored for hyperkalemia.
Too Little Potassium
- Hypokalemia
- Hypo -too little or under
- kal- potassium
- emia- pertaining to the blood
For the longest time, I had trouble with the hypo thing. I kept thinking of shots and needles, not poking under the skin.
What caregivers should look for to suspect Hypokalemia
This time it’s all about not taking in enough potassium and or losing too much potassium from the body. Muscle cramps are the symptom of low potassium that everyone knows about. Also, look for muscle weakness and fatigue, and constipation. In more severe cases paralysis and heartbeat irregularities occur. Still pretty general symptoms but now you know what type of patient you are looking for.
Who is at risk for Hypokalemia?
Possible at-risk groups are much broader in scope than Hyperkalemia. The most common cause of excessive potassium loss is due to prescription diuretic medications that increase urination. They are also known as water pills. Caffeine is also considered a diuretic. Chronic vomiting and or diarrhea can also result in extra potassium loss. Mental Health homes will need to monitor their anorexic and bulimic patients who are having trouble with their therapies. Pica patients who eat clay are also at risk. The clay binds up the dietary potassium and it passes straight through the patient.
Potassium is pretty common in the foods we eat so it is pretty rare that the primary reason for low potassium is from poor diet. Cases I can think of are bedridden patients that are fed through NG tubes. They are pretty rare in the In-Home setting but not unheard of.
What concerned caregivers should know is that multiple contributing factors have accumulative effects. Those with poor diets who have a case of diarrhea and take water pills are naturally at higher risk. Caregivers must keep their eye on the bigger picture when symptoms start to occur. For example, water pill patients who usually have no muscle cramps may get them after a case of chronic vomiting.

Interesting Fact- Licorice has a chemical that can mimic aldosterone, the hormone that controls how much potassium we lose through urination. Those who chronically consume a lot of licorice can eat themselves into hypokalemia. Pretty rare I know but I actually know of an elderly gentleman who used to buy black licorice pipe candy by the case lot who got sick.
Caregiving skills and Potassium
Now let’s talk about how In-home caregivers have an unusual amount of control of therapeutic potassium. When the body uses up its potassium stores it pulls in what is needed from the foods we eat. If a caregiver starts to suspect hyper or hypo K+ problems they can compensate by altering the menu. This is a first-line therapy that does not need a prescription. Often minor cases of potassium problems can be alleviated in this way. But, this gets kind of tricky and can land you and the patient in a lot of hot water if things go wrong. So, don’t be lazy and mess up.
Caregiving techniques that will help you not to mess up
- Know your patient. Pay attention to your people until you know what is normal for them. Create a file for them. List all the medical problems, medications histories, and observations. Just the mere fact that you write all this down will kick up your caregiving a notch or two. After you have written things down, actually use the info. Bring the file with you to the doctor. Use it to train substitute caregivers. Use it when dealing with any member of the care team, therapists, and government regulators.
- Increase monitoring when abnormalities occur. When strange things happen first ask yourself, “Why is this happening?” Review the side effects of all the drugs being taken. Note any recent causation events like illnesses, strenuous events, hot weather, etc. Look for patterns in behaviors especially events that repeat themselves. The Mars and the PRN log will be very important data to monitor.
- Act with a plan in mind. You are essentially implementing a medical experiment. Do so in an orderly fashion.
-
- What is the goal of the experiment?
- What steps are you going to take?
- What are you going to measure?
- When does the experiment stop?
- Every intervention is just temporary in nature. You are just trying to help the body solve little hiccups in events. If things become chronic then a doctor needs to be involved.
- Reoccurrences require the doctor’s attention. When events repeat themselves, they are probably a symptom of other medical problems. After the doctor has taken a look at things ask if you need standing orders to intervene in the future. Educate the doctor on what you can do and even make suggestions in writing for his yes or no approval. Include the standing orders in the patient’s file. More about what you can do later on. “When in doubt send them out” Get the doctor's attention when you have a worry. Emails are a great way of communicating and documenting at the same time. If this doesn’t work, try the nurse or work thru the pharmacist. (They are the back door to the doctor’s attention)
If a diagnosis of Hyper or Hypokalemia is given by the doctor you will have to work with the them on what to do. He may not even consider you in his therapy decisions. It never hurts to remind him that you are there and can have a big impact on what can be done. Let’s talk about that concept now.
How much Potassium is needed?
Giving an exact figure for how much potassium is needed by a body is just too hard. There are too many variables involved. But the National Institute of Health, Office of Dietary Supplements has published an “Adequate Intake” guideline. Source https://ods.od.nih.gov/factsheets/Potassium-HealthProfessional/
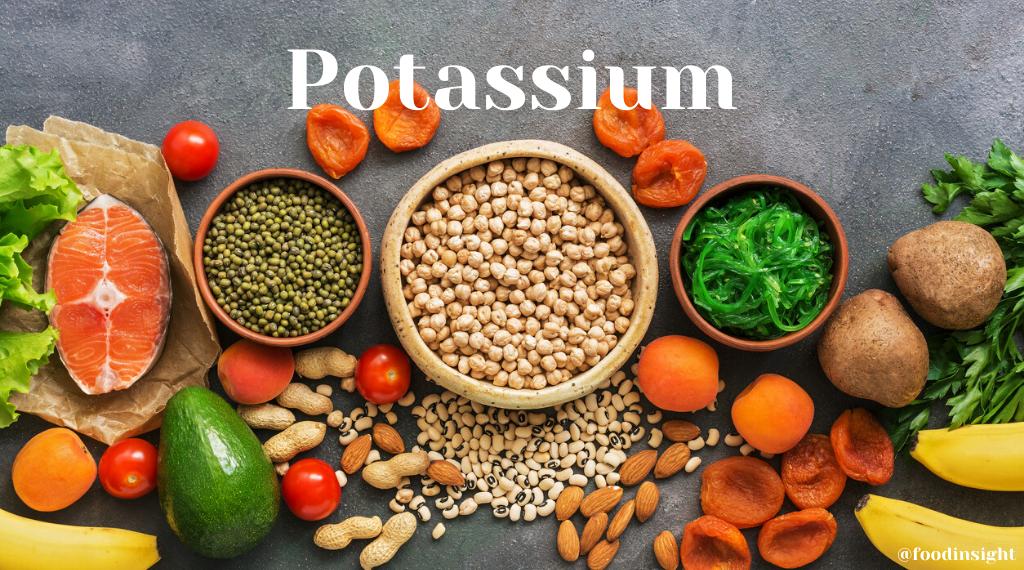
From an In-home caregiver's point of view, such tables and guidelines are practically worthless. You are not measuring out mg of potassium or looking up how much food contains what amount. A more useful guideline is based on potassium being abundant in nature. It’s pretty easy to obtain normal amounts if you- Cook from scratch. Have a balanced diet. Include lots of color on the plate. Have two servings of fruits or vegetables at the main meal and at least one serving for lunch and breakfast. Include whole grains, dairy, and seafood (including tuna fish)
Interesting fact- Potassium and sodium are closely interconnected but have opposite effects on the body. Both are essential nutrients that play key roles in maintaining physiological balance, and both have been linked to the risk of chronic diseases, especially cardiovascular disease. High salt intake increases blood pressure, which can lead to heart disease, while high potassium intake can help relax blood vessels and excrete sodium while decreasing blood pressure. Our bodies need far more potassium than sodium each day, but the typical U.S. diet is just the opposite: Americans average about 3,300 milligrams of sodium per day, about 75% of which comes from processed foods, while only getting about 2,900 milligrams of potassium each day. Source https://www.hsph.harvard.edu/nutritionsource/potassium/
Foods that have Potassium
Now that we have got the “Adequate Intake” covered let’s look at how to manipulate the diet when more potassium is needed. Or conversely what foods to avoid if you need to cut back. I have been where you are now. I have taken the education courses and told myself, “This sounds easy enough, I can do this potassium thing”. But, when I was standing in my kitchen deciding what to cook it all fell apart. In my opinion, there were three reasons why I failed.
- I did not have enough of the right foods in my kitchen in the first place.
- Trying to save money I shopped for whatever was the cheapest, not what was the most nutritious.
- Spur of the moment deciding what to cook is a terrible way to plan a menu. Appetites and conveniences usually win out over specific nutrition plans.
Here is one plan that will make it easier to make this potassium menu thing happen much easier. First, start by knowing what foods are high in potassium. Print out a list of the foods that you and the ones you cook for like. Second, with this list in hand sit down with the weekly grocery store sales ads and make up your shopping list. Take note of which items are on your potassium list that are on sale. Third, after you know what you are going to buy, plan out your menu for the week. I always found it was much easier to sit down at the computer with a form that I could fill in. Something like the following.
__________________________________________________
Monday
Main dish-
Veg 1-
Veg 2-
Dessert-
___________________________________________________
You can build this form out any way you want and include breakfast and lunch too. Then print it out and place it in the kitchen or pantry. Then next week when the sales ads come out do the same thing over again. The bottom line is having some budget-friendly stocks of potassium-rich foods and a preplanned menu before you get into the kitchen to cook.
Table 2: Potassium Content of Selected Foods
|
Food |
Mg per serving |
|
Apricots, dried, ½ cup |
1,101 |
|
Lentils, cooked, 1 cup |
731 |
|
Prunes, dried, ½ cup |
699 |
|
Squash, acorn, mashed, 1 cup |
644 |
|
Raisins, ½ cup |
618 |
|
Potato, baked, flesh only, 1 medium |
610 |
|
Kidney beans, canned, 1 cup |
607 |
|
Orange juice, 1 cup |
496 |
|
Soybeans, mature seeds, boiled, ½ cup |
443 |
|
Banana, 1 medium |
442 |
|
Milk, 1%, 1 cup |
366 |
|
Spinach, raw, 2 cups |
334 |
|
Chicken breast, boneless, grilled, 3 ounces |
332 |
|
Yogurt, fruit variety, nonfat, 6 ounces |
330 |
|
Salmon, Atlantic, farmed, cooked, 3 ounces |
326 |
|
Beef, top sirloin, grilled, 3 ounces |
315 |
|
Tomato, raw, 1 medium |
292 |
|
Broccoli, cooked, chopped, ½ cup |
229 |
Source https://ods.od.nih.gov/factsheets/Potassium-HealthProfessional/
We all have heard that bananas are high in potassium, but you will notice what foods have more potassium per serving. Potatoes with the skins on have even more potassium than what is listed above. Who knew that a side dish of Potato JoJos or a handful of raisins in your oatmeal would be better than a banana, at least as far as potassium is concerned.
There are other lists out there on the internet detailing how much potassium is in certain foods. If you want, look them up yourself. The real caregiver magic comes from grocery sales ad- potassium-rich food, menu planning. If you have a specific potassium need, shop for your groceries with that need in mind. Then cook your way to making your patient’s temporary potassium problems away. All while saving money. Pretty cool isn’t it?
In-Home Caregivers Secret Weapons
The following are three extra ways to kick your potassium-rich menu into overdrive when you need it too. If you are wondering when that would be think of cases of leg cramps.
- Daily Values. In America, prepackaged foods are required to have a Nutrition Facts panel printed on the package. It includes how many milligrams of potassium per serving and what percent of the total daily requirement (DV) each serving has. That makes it really easy to pick up a package of “Classic Caeser Croutons” and notice that it has only 6mg of potassium per serving or 0% DV. Safe food for Hyperkalemia but not so great for Hypokalemia.
- Snack therapy for Hypokalemia. An easy way to add potassium to the diet is by providing potassium-rich snack foods like a can of low sodium V8 vegetable juice (900 mg), a ½ cup of dried apricots (1,101 mg), or ½ cup dried prunes (699mg).
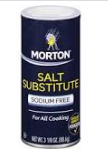
- Salt substitutes products are straight potassium chloride instead of sodium chloride. Just a ¼ tsp contains 690 mg or 20% of the DV. Look for products like N0-Salt, NU Salt, or Morton’s Salt Substitute in the spice aisle of the grocery store. A caution to remember when using a lot of these products. Potassium triggers stomach acid production which may lead to an upset stomach. The remedy is antacid tablets or saltine crackers.
 |
 |
 |
Medications and Potassium
I’m a pharmacist by training so you know I am going to talk about drugs. It’s what I do. Let’s start with supplements.
Supplements
 You might be thinking if potassium is so important why don’t I just go buy an over-the-counter mineral supplement. After all, there has got to be a “pill for every ill”, right? Yes, you can purchase potassium supplements and potassium is added to most multivitamins and other combination supplements. But read the label. You will never find a pill that contains more than 99mg. Why? The National Institute on Health website says the following.
You might be thinking if potassium is so important why don’t I just go buy an over-the-counter mineral supplement. After all, there has got to be a “pill for every ill”, right? Yes, you can purchase potassium supplements and potassium is added to most multivitamins and other combination supplements. But read the label. You will never find a pill that contains more than 99mg. Why? The National Institute on Health website says the following.
“Many dietary supplement manufacturers and distributors limit the amount of potassium in their products to 99 mg (which is only about 2% of the DV) because of two concerns related to potassium-containing drugs. First, the FDA has ruled that some oral drug products that contain potassium chloride and provide more than 99 mg potassium are not safe because they have been associated with small-bowel lesions. Second, the FDA requires some potassium salts containing more than 99 mg potassium per tablet to be labeled with a warning about the reports of small-bowel lesions” Source: https://ods.od.nih.gov/factsheets/Potassium-HealthProfessional/
Two percent of the DV is nothing. An insignificant amount if you are looking for a temporary solution for hypokalemia problems. Small bowel lesions risk is another reason why excessive dietary potassium therapy should be temporary in nature. Anything more permanent has got to go through the doctor.
Drugs with potassium concerns
I’ll make this simple for you by listing all the drugs on a table.
Table 3. Drugs with potassium concerns
|
Name |
Effect on Blood K+ |
|
NSAIDs |
Hyper |
|
ACE inhibitors (angiotensin converting enzyme inhibitors) · Benazepril (Lotensin) · Captopril (Capoten) · Enalapril (Vasotec) · Fosinopril (Monopril) · Lisinopril (Zestril) · Moexipril (Univasc) · Perindopril (Aceon) · Ramipril (Altace) · Trandolapril (Mavik |
Hyper |
|
Heparin |
Hyper |
|
Cyclosporine |
Hyper |
|
Sulfamethoxazole and Trimethoprim · (Bactrim) · (Septra) |
Hyper |
|
Beta-blockers · Labetalol (Trandate) · Metoprolol (Lopressor, Toprol-XL) · Propranolol (Inderal) |
Hyper |
|
ARBs (angiotensin II receptor blockers) · Atacand (candesartan) · Avapro (irbesartan) · Benicar (olmesartan) · Cozaar (losartan) · Diovan (valsartan) · Micardis (telmisartan) · Teveten (eprosartan) |
Hyper |
|
Spironolactone (Aldactone) |
Hyper |
|
Thiazide diuretics · Hydrochlorothiazide · Chlorothiazide (Diuril) · Indapamide (Lozol) · Metolzaone (Zaroxolyn) |
Hypo |
|
Loop diuretics · Furosemide (Lasix) · Bumetanide (Bumex) · Torsemide (Demadex) · Ethacrynic acid (Edecrin) |
Hypo |
|
Corticosteroids |
Hypo |
|
Antacids |
Hypo |
|
Insulin |
Hypo |
|
Fluconazole (Diflucan) |
Hypo |
|
Theophylline (TheoDur) |
Hypo |
|
Albuterol · (ProAir) · (Provental) |
Hypo |
|
Laxatives |
Hypo |
Special Note. ARBs and ACE inhibitors are combined with hydrochlorothiazide (HCTZ), like in lisinopril/HCTZ and valsartan/HCTZ. The hypo and hyperkalemia effects sort of cancel each other out.
If you start to see abnormality symptoms and are suspect any of the above-listed drugs, bring it to the attention of the doctor or pharmacist. Talk in specifics backed up by measurable data and you’ll get their attention easier. The doctor may or may not do anything. If the problems continue or get worse, you may have to push for a blood test. In the case of HypoK+, the doctor may just order a potassium prescription.
Potassium Prescriptions
Potassium prescriptions come in 8mEq, 10 mEq and 20mEq strengths. The brand names are Klor-Con or K-Tab. They are produced in delayed-release tablets or capsules and powder packets. They are made delayed-release to reduce the stomach upset side effect of potassium.
What is important for In-home caregivers to know is that you cannot crush break or chew the tablets. Too much potassium will be released at one time into the stomach. The tablets have been known to stick in the throat so take them with plenty of water.
Potassium tablets/capsules and NG feeding tubes have problems. If there is an NG tube, if your patient is a tablet chewer or if there is a swallowing difficulty (the tabs are kinda big) I suggest you talk to the doctor about the following suggestions.
- Powder packets. Add to a liquid and administer the medication.
- Capsules. You can pull apart the capsules and mix the time-release beads into pudding or a liquid that is easier to swallow.
- Ktab 8mEQ are smaller tabs and are easier to swallow whole.
Final notes, Taking potassium prescription with food reduces the chances of an upset stomach. Also, you might find a tablet in the stools. Don’t worry, all the potassium has been released and digested by the time the tablet reaches the toilet.
Conclusion
Potassium is a big deal. Every cell of our body counts on potassium being around in a very controlled concentration. Though the body is very good at regulating intracellular and extracellular quantities of potassium by itself sometimes things can go wrong. Medication and illness can throw off potassium’s balance. When symptoms of Hypo or Hyperkalemia start to manifest themselves in patients, In-home caregivers can reduce the problem through diet modification. If skill is used caregivers can handle minor occurrences and work with the doctor on bigger potassium issues.
As always good luck in your caregiving
Mark Parkinson BsPharm
References:
- James L. Lewis III, MD. Overview of Potassium's Role in the Body. Merck Manuals Consumer Version. Oct 2021 https://www.merckmanuals.com/home/hormonal-and-metabolic-disorders/electrolyte-balance/overview-of-potassiums-role-in-the-body
- Barbie Cervoni MS, RD. What Is Potassium? Benefits, Side Effects, Dosage, and Interactions Verywell Health. May 14, 2020. https://www.verywellhealth.com/health-benefits-of-potassium-4588613
- Body fluids and electrolytes. https://www.youtube.com/watch?v=__97EkVevb0&t=294s
- Potassium Chloride. Drugs A to Z, Drugs.com https://www.drugs.com/potassium_chloride.html
- Potassium. Linus Pauling Institute at Oregon State University https://lpi.oregonstate.edu/mic/minerals/potassium
- Potassium. MedlinePlus.NIH. Oct 20 2017. https://medlineplus.gov/potassium.html
- Potassium Fact Sheet for Consumers. NIH National Institutes of Health Office of Dietary Supplements. Mar 22, 2021 https://ods.od.nih.gov/factsheets/Potassium-Consumer/
- Potassium Fact Sheet for Health Professionals. NIH National Institutes of Health Office of Dietary Supplements. Mar 26, 2021 https://ods.od.nih.gov/factsheets/Potassium-HealthProfessional/
- Potassium. The Nutrition Source. Harvard T H Chan, School of Public health. https://www.hsph.harvard.edu/nutritionsource/potassium/
- Potassium. Wikipedia, the free encyclopedia. Nov 4 2021 https://en.wikipedia.org/wiki/Potassium#Nutrition
- Potassium Content of Foods List. Drugs.com Nov 1, 2021. https://www.drugs.com/cg/potassium-content-of-foods-list.html
- Potassium. Health Encyclopedia, University of Rochester Medical Center Rochester https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=19&contentid=potassium
Exam Portal
click on [Take Exam]
Purchase membership here to unlock Exam Portal.
|
|
|
|
|
*Important*
Registration and login is required to place your name on your CE Certificates and access your certificate history.
Username MUST be how you want your name on your CE Certificate.