Pain School for Caregivers
Course 3- Chronic Pain
Author: Mark Parkinson RPh: President AFC CE
Credit Hours 2.5 - Approximate time required: 150 min.
Educational Goal:
To provide Adult Foster Care providers with information that will help them understand and manage chronic pain.
Educational Objectives:
1. Instruct about Chronic Pain and how to manage it.
2. Explain about chronic pain management tools
Procedure:
1. Read the course materials. 2. Click on exam portal [Take Exam]. 3. If you have not done so yet fill in Register form (username must be the name you want on your CE certificate). 4. Log in 5. Take exam. 6. Click on [Show Results] when done and follow the instructions that appear. 7. A score of 70% or better is considered passing and a Certificate of Completion will be generated for your records.
Disclaimer
The information presented in this activity is not meant to serve as a guideline for patient management. All procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this article should not be used by care providers without evaluation of their patients’ Doctor. Some conditions and possible contraindications may be of concern. All applicable manufacturers’ product information should be reviewed before use. The author and publisher of this continuing education program have made all reasonable efforts to ensure that all information contained herein is accurate in accordance with the latest available scientific knowledge at the time of acceptance for publication. Nutritional products discussed are not intended for the diagnosis, treatment, cure, or prevention of any disease.
Pain School for Caregivers
Course 3- Chronic Pain
The definition of chronic pain is pain lasting over 3-6 months. But chronic pain is more than just the mere passage of time. Prolong pain presents other challenges to cope with. Patients and their care givers must learn to deal with the biological, emotional and social stresses that come from the prolonged exposure to pain. To successfully cope with these new concerns caregivers and patients must have a change of mindset.
Change of care giving goals
The care giving goal in acute pain is to eliminate it. After six months of suffering it’s time to realize that’s probably not going to happen. Caregivers have to help their patients to start looking at the problem from a different angle. Instead of striving to eliminate pain it’s time to start working toward the more obtainable goal of managing pain to reach tolerable levels. The goal of care giving should be switched from being pain free to living a normal life despite the pain that won’t completely go away.
Chronic Pain Management tools
In order to successfully switch to a new pain management mindset you’re going to need a few new care giving tools in your medical tool chest. As you will see, I’m mostly talking about the mental medical tool chest in the caregiver’s and patient’s head.
Clean out the tool box
Whether they intended to or not those who suffer from chronic aches have started to adjust to a life with pain. Maladaptive behaviors are common, especially in pseudo-addiction cases.
Usually driven by the fear of pain and the lack of knowledge patients will start to;
- Horde tablets, creating “just in case” stock pile.
- Insisting that a specific brand or medication is the only drug that works.
- Go to several doctors at once or frequently change doctors and dentists (doctor shopping).
- Paying for pain meds with cash, bypassing their insurance “refill too soon” limitations.
- Adopting an “avoidance”, sedentary lifestyle (with the accompanying weight gain) and becoming socially withdrawn.
- Becoming depressed, with frequent aggressive mood swings.
- Mistrusting and bullying health professionals to get what they want.
- Borrowing medications or outright theft.
- Rely on Placebos- There is a lot of information floating around the internet, and there are a lot of home remedies that are passed down in families. There is a tendency to think that if a person tried a treatment and pain levels became less, then what they did worked in “curing” the pain and will work in all future cases. That’s just not the case. The resident may have gotten lucky the one time but most often the remedy worked because they thought it would work. Or in other words a placebo. Don’t get me wrong I believe in the effectiveness of the placebo effect and it has its place, but only if the doctor agrees with it. Some placebo cures are downright wrong and in fact scary. They should be cleared out of the tool chest.
Living with long term, sometimes severe pain is very hard. It is easy to understand why the resolve of pain victims gets worn down and over time maladaptive behaviors arise. Most patients aren’t trained in chronic pain management and are simply doing the best they can to just survive. It is up to the caregiver to help them see what they are doing and help them clean out all these dull and broken pain management tools. To accomplish the task it is critical that a proper patient assessment be done and that a relationship of trust is developed between the caregiver and their patient.
Getting new tools that work
Filling up the medical pain management tool box is going to be a process. Some things will have to be un-learned; some things will have to be learned. Not all tools will be needed every time and you’ll develop your favorites. And don’t forget, “practice makes perfect”. So let’s talk about the tools now.
Involvement tool
Modern society has trained patients to just show up at the doctor’s office and passively do whatever they are told to do, almost completely ignoring personal responsibility for their own health. In chronic cases where pain can’t be eliminated that approach leads to a lot of problems. The doctor can’t be with the patient all the time but the pain can be. If the patient is only relying on the doctor to eliminate the pain whenever it pops up, they will become frustrated when the pain continues despite following the doctor’s instruction. In other words the person in pain is looking for a magic bullet to permanently kill the pain monster and gets mad and depressed when the doctor doesn’t give them one.
Patients must learn to go from a completely passive role to a more active participation role, forming a partnership with the doctor. Caregivers can place themselves right in the middle to make things happen. On the one hand are the doctor and the care team, with all their knowledge and prescriptive power. On the other is the patient, taking on more personal responsibility for their own pain management.
Caregivers roll
The caregiver’s role is to facilitate both efforts to reach the goal of a normal lifestyle for the chronic pain patient. How? Communication and follow through.

The doctor’s side- The caregiver can help the doctor by making sure all of their instructions are followed. More importantly they can give feed back to the doctor about what is working and to what degree it is working, what is not working and what other problems and concerns are popping up. The doctor can’t be with the patient all the time but their influence can be; through the caregiver’s efforts.
The patient’s side- The ability of patients to take care of themselves varies a lot. They have hired the caregiver to help them do what they can’t do. It will be up to the caregiver to help the patient take a more active role in their pain management. To help them understand the doctor’s instructions and what the requirements are in managing their own pain. To help them establish realistic expectations about eliminating their aches. To help them communicate the important details about the outcomes of their pain therapy back to the care team. They can succeed at living a normal life because you are there all the time to help them through every event, expected and unexpected, that effects their pain levels.
Patience tool
Being in the middle is sometimes not fun. It helps to remember some basic realities in pain management and compensate for them with copious amounts of patience.
- Most doctors have minimal chronic pain therapy training. If they can’t fix the underlining problem they are at a loss of what to do. If you suspect this is the case, ask the doctor or have the family ask the doctor if they have had chronic pain management training. If they haven’t you might ask for a referral to a pain specialist.
- Living with chronic pain is stressful and takes a lot out of a person. A client’s social emotional and especially biological coping mechanisms can get depleted. When they’ve got nothing left, often the patient will lash out at anyone close by. In these cases the patient literally can’t help themselves from exploding on you. Let them vent and keep coming back with plenty of understanding and empathy. It helps to explain to the client about the biological reasons they feel so out of control with their emotions. I personally have found that it helps a lot to tell them that “It’s ok to vent, you’ve just used up all your coping chemicals in your system and it’s time to build up your supply with rest, proper exercise and nutrition”.
Measurement tools
Chronic pain is treated differently than other chronic conditions. Therapy decisions are driven by how a patient feels more than what the doctor thinks is the next logical medical step concerning the progression of the underline disease state. The course of therapy is determined by feedback from the patient more than what can be measured with other medical instruments. But quantifying how much pain is felt is very difficult. Pain is a biological and emotional experience therefore literally each case is different from all others. How do you measure how much pain there is so the doctor can decide what to do next? Answer, pain scales and symptom journals.
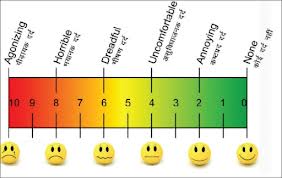
Pain Scales
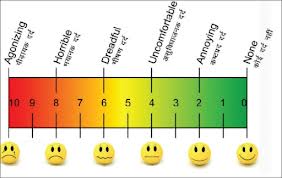
Pain scales are assessment systems where the patient is asked to rate their pain on a set scale. For example a numerical pain scale would be 1 through ten with ten being the worse pain ever experienced. Other pain scales add cartoon figures or colors to help patients better describe their pain.
It is important for the caregiver to use the pain scale properly.
- Find out which scale the doctor uses.
- Help the patient set a reference point that stays the same. Example, 10 is the worse pain you have ever felt, like when you gave birth or had kidney stones.
- There are different types of pain (stinging, hot, dull, sharp). It is not unusual for several types of pain are felt at the same time. The types of pain felt are important clues for the doctor. So report the types of pain and which one predominates
Example- The pain today is a 7, predominately a dull ache.
- Sometimes it’s easier for a person to point to a picture than to verbally describe their pain. Print out a picture of the pain scale and always have it ready to use.
Symptom Journals
Because pain is subjective and is emotionally influenced, what is going on in the rest of the client’s life is also important factors to consider when treating pain. It is entirely possible for a patient to experience pain at level 8 and cope with it because they are feeling happy that day, whereas on down days a pain level 0f 5 might be hard to cope with. Other factors can affect pain like uncontrolled blood sugars or blood pressure.
Some doctors have their patients keep a symptoms diary to help the doctor understand the bigger picture. Symptom diaries give the doctor more information about the condition of the patient. Consider the different answers to the question, “How have you felt over the past week?” 1. I feel fine, sometime painful. 2. Here is a record of the symptoms I felt last week. If you were a doctor which answer would you want?
Here again the caregiver must know how to properly complete a symptoms journal.
- Entries must be brief and to the point. Too much unusable info is pointless
- Find what information the doctor wants and how he wants it recorded.
- Try to be clear in recording info. Recording. “Sue had at 7 pain day, predominately a sharp shooting pain in her lower back, plus she was depressed and had a bad night sleep, is better than sue was in pain today.
- These aren’t medical chart notes; pain journals are just an unscientific record of what events that you and the patient feel are important for the doctor to know.
Giving the doctor more information is always good. In addition you will find that once a journal is kept that self-management of pain will become easier to accomplish. It forces the client to evaluate what is going on and what they are doing that effect the pain levels they experience. It also helps keep track of what works and how much improvement happens over time. Success breeds optimism and more success.
Communicating how a patient feels is a critical piece of information that the doctor needs in order to achieve effect pain therapy. Knowing how to collect that information is a critical role that a well-informed caregiver can fulfill. It is a “must do” function in order to have happy (therefore easier to take care of) residents.
Sleep tool
Pain disturbs sleep and not getting enough sleep causes you to feel pain more. It also reduces your ability to handle stress. It’s a downward spiral that around 2/3 of pain patients experience. But the cycle can be broken. It takes a bit of work but it’s worth the effort. A good night of restorative sleep is an excellent pain killing technique.

Sleep has a natural pattern that we don’t even have to think about. But when that pattern is disrupted we do have to make a concerted effort to maintain our regular sleep cycle. We have to pay attention to our sleep hygiene which is a fancy way of saying what we do that affects our sleep.
Proper Sleep Hygiene
- Make sleep times a habit. Establish a set sleep and wake pattern and stick to it.
- Control day time napping. You may have to suffer through a couple of grouchy periods of day time drowsiness until night time sleep kicks in. It helps to remind the patient you are trying to get control over the pain and sleeping properly helps.
- 4-6 hours before bedtime avoid; alcohol, spicy foods, a big meal and caffeine (from all sources) I know caffeine reduction causes withdrawals, again look at the long term goal of pain management.
- Exercise, but not at night
- Before bed try relaxation techniques like, meditation, calming music, and reading.
- Control the sleep environment. Pay attention to light, noise and temperature issues.
- Train the resident to view the bed as for sleeping only. Watching TV, reading in bed, eating in bed all creates habits that work against the sleep cycle.
- A light snack can get rid of a loud and demanding stomach. The old remedy of a glass of warm milk really can help.
- Beds are for sleeping not for worrying and thinking about the stress of the day. A pre-sleeping ritual of taking care of the problems and purposeful relaxation can be of great benefit.
- If the resident wakes up in the middle of the night and can’t get to sleep in 15-20 minutes, then have them get out of bed and try some relaxation techniques. Then go back to bed. Remember beds are for sleeping, not for rolling around back and forth.
One final note on the subject of sleep; many patients forget to talk about their sleep problems with their doctor. You as an informed caregiver should not. There are many sleep inducing options to choose from, including those medications that have a side effect of drowsiness. But watch the daytime napping that may occur as well.
Emotional tools
It is an established medical fact that people with positive mental attitudes can handle pain better. Conversely it is also known that stress, worry, depression or those thing that affect us negatively emotionally makes us feel pain more. In other words a positive, warm, caring and stress free environment is a good pain killer. If the patient can’t manage it by themselves the caregiver can greatly influence the client’s environment to create a positive attitude.
Here are a few helpful hints for you.
- Reduce stress by believing the patient’s report about pain levels. Pain is subjective and our perception of pain changes all the time. The caregiver can never really know how their client is feeling pain. Nothing is more aggravating to a chronic pain patient than to have those around them thinking that “the pain is all in their head” or “they’re just doing this for attention”. It’s really stressful to be in pain and no one believes you.
- Lack of information can lead to fear. Fear leads to negative emotions. Educate your clients; keep them informed in a positive way.
- Watch for signs of depression. I know you can’t diagnose but the old caregiver rule works, “When in doubt, send them out- to the doctor that is”
- Stress free environments create stress free clients. It is no coincidence that most Alzheimer centers have giant calming fish tanks, calming music and subdued color schemes.
- Anti-anxiety meds are a two edge sword. If a client has to rely on drugs to control themselves they will most likely be a very “Negative Nell”. Relying on medicine to keep a person calm has its own set of problems to deal with. I recommend using meds as a last resort, not a first line therapy.
- Social interactions usually lead to positive attitudes. Humans are social creatures and suffer emotionally when we don’t get enough interactions. Pain tends to isolate a person. Caregivers have to fight that and find ways to compensate. Wheel chairs, chair lifts, canes, swivel discs and gait belts are all devices that can help your clients get up and interact with people.
Exercise/Mobility tool
Uncontrolled chronic pain creates an intense fear of pain. The fear of pain creates a down ward cycle of pain avoidance; avoidance leads to inactivity, inactivity lead to a sedentary life style, a sedentary life style leads to poorer health which increases the pain that is felt. Exercise and staying mobile breaks this harmful cycle.
Exercise benefits the chronic pain patient by;
 Releasing endorphins, the body’s natural pain killer and mood enhancer.
Releasing endorphins, the body’s natural pain killer and mood enhancer.- Relieves stress and works off anxiety.
- Strengthens muscles and joints
- Creates a sense of accomplishment that leads to optimism
- Leads to a sense of well being
- Increases blood flow which speeds healing
- Decreases fatigue and increases energy
- Improves sleep
Two major hurdles to overcome in establishing an exercise routine are the fear of pain and overexertion caused pain. Both can be overcome by the principle of low and slow. Start with the easy stuff and gradually increase. I’m a huge fan of daily walks. Other easy exercises are shopping trips, stationary bikes, tread mills and steppers. Exercise articles always suggest water aerobics but that’s very problematic for care homes.
Mobility
Set exercise routines are not the only way to go. Any movement is exercise. Just keeping mobile will have its benefits. Keeping mobile also makes regular exercising easier.
Some mobility exercise ideas for you to try are;
- Tae chi, you can buy or check out instructional videos
- Hobbies
- Simple household chores like dusting one’s own room, setting the table etc…
- Gardening
I think you get the idea. These types of activities also give back to the client a sense of control in their life that they might feel they have lost. Mobility aides help tremendously. You could buy them and rent them to the patient, (another income source for you).
Alternative/complementary therapy tools
Drugs are not the only way to handle chronic pain. There are a number of different therapies that could be utilized. Frankly though that is not an area that caregivers have much to do with. You could make suggestions to the doctor or the family of the client could make the suggestions. You could also plant the idea in the head of the doctor or family by asking the right questions. But for the most part these therapies are for the doctor to worry about.
It would be nice though for you to have a list of therapies and a short description to consider.
Massage

Massage is probably the oldest pain relieving therapy that has ever existed. Numerous studies have proven its therapeutic benefits over and over again and yet modern medical science still haven't figured out exactly why it works. Current thinking is massages are beneficial for several different reasons.
- Pumps more oxygen and nutrients into tissues and vital organs while helping to remove metabolic waste.
- Helps the body enter a relaxing rest-and-recovery mode that enhances the healing processes. (reduces inflammatory responses and increases healing and pain killing hormones)
- Reduces stress and tension, factors that slows the healing process.
- Increases the general since of well-being which helps fight depression, another factor that slows healing and makes you feel pain more.
- Better attitudes also help bear pain easier which enables you adhere to other healing therapies better
Therapeutic massage should be done be a licensed professional. The care provider can perform everyday duties that can have massaging benefits such as apply lotion on the legs and back or just a simple back rub.
Posture
There are neutral positions for our bodies that present the least amount of stress on our systems. In the classic pain management theory "good posture relieves chronic pain" the goal of therapy was to relieve pain by trying to keep the body in those neutral positions for as long as possible. There are pain experts who question that assumption but it is undeniable that bad posture can add to pain if the area still has damage. So good posture takes stress off of areas where it's not supposed to be, resulting in less pain. Once the body is healed good posture may still have a role to play in convincing the mind that there is no need for pain. New studies show correct posture has a great positive effect on mental attitudes. Patients with positive attitudes can bear chronic pain better. So sit up straight, be proud and smile. There are devices such as “Back Joy” and various kinds of back and leg braces that the doctor could choose from. The care provider must know that holding a body in any one position for too long is actually bad for chronic pain. The body is built to move around not to stay in one place.
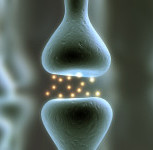
TENS Units-
Transcutaneous electrical nerve stimulation unit. It is a device that sends mild electrical current to the skin with the goal of disrupting nerve signals. It sounds modern and high tech but the use of electricity in pain control has been around for some time. There are even pictures of ancient Egyptians using electric eels to cure pain. Science has yet to figure out how it actually works. The current theory is that the electrical signal shuts the “pain nerve gate” so the pain signals never reach the brain. It has also been discovered that lower electrical signals stimulate the release of the body natural pain killing chemicals called endorphins.
Trigger Point Massage
Trigger Points are hyperirritable spots in muscle tissue. They are associated with nodules of taut muscle fibers thought to be a defensive mechanism to protect injury sites. They can contribution to chronic pain flairs, referred pain and unexplained pain in larger areas. Trigger points develop when muscle structures become weakened or damaged resulting in tiny tears appearing in muscle tissue. As these tears heal they contract or shorten the muscle tissue causing twisted and knotted fibers. These knots restrict blood flow and muscle movement. The nerve senses something is different and sends signals to the brain. The brain then produces pain as a warning and protection against the abnormality. Due to nervous system "wiring" the body may feel the pain in a larger area or even at distant areas of the body. Deep tissue massage by the use of a “Thera Cane” or similar device can resolve the trigger point.
Chiropractic Manipulation
Chiropractic medicine is a controversial area of therapy because of its many unscientifically proven tenets of practice. In regards to pain, its basis of practice is to manipulate the spine and joints thus effecting nervous system signals to the brain in order to alleviate the pain.
Acupuncture
Acupuncture is another controversial area of medicine because of its unscientifically proven tenets of practice. In regards to pain its technique is to inset pins into the specific points on the body for a set amount of time.
Range of Motion.
There are multiple therapies that effect pain through the movement and exercise of the body. It is thought to affect pain by, increasing blood flow, strengthening of muscle and joints, reducing stress, increasing relaxation. They also might combat the “fear of pain” by proving to the body and the mind that activity can be done without significant damage to the body. Therapy should always be done by skilled experts so harm can be avoided. Therapies include; water aerobics, physical therapy, yoga, tae chi, Feldenkrais method and others
Nerve block
Nerve block is as the name suggests, is a therapy that blocks the nerve from functioning. It can be temporary or permanent. Temporary nerve block is achieved by the injection of anesthetic drugs to a specific region where the pain originating nerves are. Usually the injections are a combination of numbing agents and anti-inflammatory medication. Permanent nerve block is killing the nerve through the use of chemicals, freezing (cryoanagesia) or heating the nerves (radiofrequency radioabaltion)
Cognitive and Biofeedback
Cognitive and Biofeedback are psychological therapies practiced by mental health professionals design to help the pain patient develop greater mental coping skills. Many pain patients get confused and worried when their doctor refers them to a mental health professional. You the care provider can help them understand that they are there to help the client cope with the pain and not any mental health issues.
Pain Pumps
Pain Pumps are medication delivery devices that inject pain medicines directly into the spine. To lower the risk of infection they are usually surgically placed under the skin. Since the medicine is injected directly into the spine the quantities needed are greatly reduced. Medicines are replenished by injecting the drug into a reservoir in the pump. Dosages can be altered through the use of a remote control device.
Care plan tool
As with any chronic condition, chronic pain is best managed by establishing a plan of action. In medical terms that’s called a care plan. As a medical professional and as part of the care team it is perfectly normal (and in most states legally required) for you the caregiver to ask the doctor to give you a pain management care plan. Pain specialists will have one all set up. They may not be used to working with residential care providers. It will be wise to educate them about what you are and what you can do. Doctors who don’t have pain training might stonewall you. Be patient they probably don’t know what to put into a pain care plan and don’t want to look like they don’t know what to do.
Elements of a basic pain care plan
Each care plan is unique to the patient and their condition but there are elements common to most care plans. If the doctor isn’t forthcoming with a plan of action you can use the following form that might get the process kick started.
---------------------------------------------------------------------------------------------------
Dr _________.
Your patient _________________ is in (care home name) and under my care. It is required by the state that I get detailed instruction from you in regards to the management of (patient’s name) chronic pain condition.
I understand that most likely we will not be able to totally eliminate all the pain. I also understand that patient feedback is critical in the management of pain. I feel confident that by working closely with you we can manage the pain so that the patient can live a normal life.
Please provide me with your pain management care plan for (patient’s name). I would like to have your instructions about the following.
What pain measurements/evaluations would you like to see and how often?
Would you like a pain/symptom journal kept?
What pain medication and instructions am I to use for base line pain control?
What PRN pain medication and instructions do you have for breakthrough pain?
What preventative, complementary or alternative pain therapy and instruction do you have?
Do you have any instructions about the chronic pain issues of?
Sleeplessness
Pain caused anxiety and fear,
Depression
Exercise (endurance, range of motion, etc…)
Pain medication induced constipation
Pain medication tolerance
Bed rest
---------------------------------------------------------------------------------------------------
This form works on a couple of different levels.
- It makes you look very professional and you get more cooperation from both sides
- It gently educates the doctor about chronic pain issues.
- It gives you some back up when you’re trying to change patient attitudes and beliefs.
Common sense Helpful hints.
A lot of good care giving practices are just a good helping of old fashioned common sense. Here’s a few that have been found to help in reducing pain.
- Put client walks on the daily chore list, right along with cooking meals and making beds
- Lighten the wallet. Big bulky wallets can make the resident sit funny.
- Look at the shoes. Too loose, too tight, too much heal, no padding left?
- Loose fitting clothing is better for chronic pain.
- Make friends with the doctor’s staff and the pharmacy techs. You'd be surprised at the power of a plate of thank you cookies.
- Keep info you bring to the doctor brief, Keep it around 1 page or you'll lose the full attention of a busy doctor.
- Get the patient to quit smoking- Nicotine causes blood vessels to constrict blood flow leading to increased pain. (Proven in studies) A nicotine fix is just not worth the extra pain.
- It's easier to get through to your doctors nurse than it is the doctor.
Overall Focus
I have talked to you about a lot of things and it’s easy to get lost in all the details so let us get back to the overall focus. Chronic pain management is more than just eliminating pain. It’s dealing with all the contributing factors that affect the pain levels of your client. As you have been shown it is much more than trying to find that “magic bullet’ pill. It goes beyond the “Just fix me Doc” attitude of patients. It’s realizing that doctors do not have a crystal ball and they need your observations and feedback. It’s realizing that many things affects pain levels and it up to you to help find them and help control those events with the goal of making your client feel better. It’s realizing that your pain management efforts will mostly likely never be done. It’s realizing that the most important member of the pain management team is the patient and you as their advocate will have to help them in all their efforts. It’s realizing that good pain management is good care giving and will ultimately make your job easier in the long run.
 |
Conclusion
Pain is the most prevalent aspect of practicing medicine today. Our focus on pain has become more sharpened. Ongoing research has given us a clearer understanding about what it is and where it comes from. With that new understanding, new and better methods of dealing with pain are being developed.
Care givers must realize that because pain is felt so subjectively, the most effective pain management techniques are patient driven. Because care givers have so much interaction with patients and are their advocates, care givers are the engines that drive the patient’s efforts.
So, after reading these courses about the different aspects of pain, how does your current pain management tool box look? Are there any dull, broken or just plain wrong tools cluttering up your tool box? What efforts are you going to do to get the tools you need and sharpen the dull ones in your pain management tool box?
Good luck in your efforts, I hope you become a pain management expert. Many of your clients certainly need you to be one.
Speaking of pain..... it's time to take the test now.

PS congratulations on finishing pain school.
Other resources
Here are places you can go more information and training. They are designed with the patient in mind. You will get the most out of them by placing yourself in the role of the patient.
- painAction.com -http://painaction.com/
- American Chronic Pain Association-http://www.theacpa.org/
- Partners against Pain- http://www.partnersagainstpain.com/
- WebMD Pain Management Center- http://www.webmd.com/pain-management/default.htm
References:
1. Thomas E.Quinn. Pain Topics, What is Pseudoaddiction?. PainRreliefCconnection Vol 2 #1.Jan 2004.
http://www2.massgeneral.org/painrelief/pain%20topics/what%20is%20pseudoaddiction.pdf
2. Stephan F. Grinstead. Addiction Versus Pseudoaddiction. Addiction-Free Pain Management blog. Jan 2008 .http://www.addiction-free.com/blog/addiction-versus-pseudoaddiction/
3. Back Pain treatment. Back Pain Center. eHealth.com http://ehealthforum.com/healthcenter/back-pain/back_pain_treatment-e82.html
4. AAPM Facts and Figures on Pain. American Academy of Pain Medicine. http://www.painmed.org/patientcenter/facts_on_pain.aspx
5. Partners Against Pain. http://www.partnersagainstpain.com/
6. American Chronic Pain Association. http://www.theacpa.org/
7.WebMD Back Pain Health Center. http://www.webmd.com/back-pain/default.htm
8. Suzanne Levy. 6 Mistakes Pain Patients Make. Health.com http://www.health.com/health/gallery/0,,20387697_7,00.html
9. John P Revord. Pain Management for Chronic Back Pain. Spine-Health.com.10/12/2012
http://www.spine-health.com/treatment/pain-management/invasive-pain-management-techniques
10. Pain Treatment Topics. Glossary of Terms. Pain Topics.org. http://pain-topics.org/glossary/
11. Massage Therapy: An Introduction. National Center for Complementary and Alternative Medicine 8/2010.
http://nccam.nih.gov/health/massage/massageintroduction.htm#safety
12. Pain Action. http://www.painaction.com/
13. Pain Medications. Drugs.com http://www.drugs.com/condition/pain-generic.html
14. Massage. Wikipedia The Free Encyclopedia http://en.wikipedia.org/wiki/Massage
15. Anesthetic. Wikipedia The Free Encyclopedia http://en.wikipedia.org/wiki/Anesthetic
16. Nora Volkow, The Essence of Drug Addiction. The Brain-Understanding Neurobiology, Teachers Guide. National Institute of Drug Abuse, National Institutes of Health
http://science.education.nih.gov/supplements/nih2/addiction/guide/essence.htm
17. NINDS Chronic Pain Information Page. National Institute of Neurological Disorders and Strokes. 5/22/13
http://www.ninds.nih.gov/disorders/chronic_pain/chronic_pain.htm
18. Sleep Hygiene: Helpful Hints To Help You Sleep. Sleep Disorder Center. University of Maryland Medical Center 8/3/2010
http://www.umm.edu/sleep/sleep_hyg.htm
19. R. Morgan Griffin, When Aches and Pain Disrupt Sleep. Osteoarthritis Health Center. WebMD 2/1/07
http://www.webmd.com/osteoarthritis/features/when-pain-disrupts-sleep
20. Exercise to Help Manage Chronic Pain And/Or Fatigue. War Related Illness and Injury Center, Office of Public Health, Department of Veterans Affairs.
http://www.warrelatedillness.va.gov/education/factsheets/exercise-to-manage-pain.pdf
21. Using the Pain Scale: How to Talk About Pain. Living With Chronic Pain, WebMD.3/9/11
http://www.webmd.com/pain-management/chronic-pain-11/pain-scale?page=2
22. Chiropractic. Wikipedia The free Encyclopedia http://en.wikipedia.org/wiki/Chiropractic
Pain School for Caregivers
Course 3- Chronic Pain
Exam Portal
click on [Take Exam]
Purchase membership here to unlock Exam Portal.
*Important*
Registration and login is required to place your name on your CE Certificates and access your certificate history.
Username MUST be how you want your name on your CE Certificate.