A Caregivers Guide to Heart Disease
Author: Mark Parkinson BsPharm: President AFC-CE
Credit Hours 4 - Approximate time required: 360 min.
Educational Goal
Provide In-Home caregivers a guide on becoming familiar with heart disease.
Educational Objectives
- Describe the Anatomy of the heart
- Review the Physiology of the Cardiovascular system
- Familiarize the reader with the pathophysiology of the most common occurs of the heart
- Explain the major risk factors for developing heart-related problems
- Tell how to work with doctors
- List Coronary system tests
- Provide guidance for Caregivers on how to manage heart disease factors and medications.
Procedure:
Read the course materials. 2. Click on exam portal [Take Exam]. 3. If you have not done so yet fill in Register form (username must be the name you want on your CE certificate). 4. Log in 5. Take exam. 6. Click on [Show Results] when done and follow the instructions that appear. 7. A score of 70% or better is considered passing and a Certificate of Completion will be generated for your records.
Disclaimer
The information presented in this activity is not meant to serve as a guideline for patient management. All procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this article should not be used by care providers without evaluation of their patients’ Doctor. Some conditions and possible contraindications may be of concern. All applicable manufacturers’ product information should be reviewed before use. The author and publisher of this continuing education program have made all reasonable efforts to ensure that all information contained herein is accurate in accordance with the latest available scientific knowledge at the time of acceptance for publication. Nutritional products discussed are not intended for the diagnosis, treatment, cure, or prevention of any disease.
A Caregivers Guide to Heart Disease
Arguably one of the most important organs in the body is the heart. It is a remarkable organ that is responsible for pumping life-sustaining blood throughout the body. It is constantly working 24 hours a day, seven days a week. The more you work it, the stronger and more efficient it becomes. It works so well and so consistently that we take it for granted until something goes wrong. When things go wrong for the heart, things go wrong for the entire body.

The leading cause of death since 1950 is heart disease, a collection of pathological conditions affecting the heart and circulatory system of the body. Altogether they account for approximately 30% of deaths in the US. That figure represents one person passing away from problems related to the heart every 34 seconds. Heart disease costs the United States about $229 billion each year. That cost includes health care services, medicines, and the loss of productivity due to illness and death.
There are multiple risk factors for developing heart disease, ranging from genetics to lifestyle choices. Literally everyone is either born with or can make bad lifestyle choices that can potentially lead to heart problems. Heart disease is preventable and if it does occur it is manageable. Unfortunately, once it has developed the risk of worsening conditions will always be present.
The heart is remarkably resilient. Normally it takes care of itself. If heart disease does develop the patient can still lead a normal life if healthy lifestyle choices are made and therapy adhered to. In-home caregivers are in an excellent position to ensure that proper lifestyles are maintained, and medical orders are followed correctly. Caregivers can be more effective in these roles if they have a greater understanding of the heart and its pathological conditions. This course is designed to start you on the journey of achieving that goal.
Anatomy of the Heart
The heart and its circulatory system are too much material to cover. You’d fall asleep by the time I’d have finished covering it. I’ll only cover the material I think that you need that will help you manage your residents well and communicate effectively with other medical professionals. Also, I want to make things a bit more entertaining so I am going to slip in a video or two. You play the video by clicking on the start arrow. If you want the image bigger, click on the full-screen box icon in the lower right corner. When you are done watching, click on the same icon to shrink it down to size. There will be quiz questions covering the video materials. Sorry about the ads if they come up on your computer, it’s what makes the videos free for me to use.
That was the big picture. Now let’s take a look at the little details. The cardiovascular tissue is mostly made up of connective tissue, nerves, and muscle. Around the blood vessels is special muscle tissue called smooth muscle. They are designed to operate automatically in response to signals from the attached nerves. They tighten around the blood vessels to narrow the passage and increase blood pressure or loosen up to drop the pressure. For example, when you stand the blood is pulled away from the brain by gravity. The smooth muscle compensates for gravity’s pull by tightening up around blood vessels. The extra pressure keeps more blood in the brain, so we don’t pass out. The blood vessels provide a pathway for the blood to move around the body. The smaller the passageway becomes the leakier it gets. This allows nutrients, fluids, and such to pass out to the tissues where it’s needed. Waste products are moved into the veins and transported to the organs that take care of the unwanted material. The first two factors will be important when we talk about the pathophysiology of the heart and the medication used to treat it.
 The walls of the heart have three layers. The innermost layer is the endocardium. It covers the heart chambers and heart valves and connects to the tissue lining of the blood vessels. The outermost layer is called the epicardium which forms part of the pericardial sac that surrounds, protects, and lubricates the heart. The bulk of the heart wall is made up of the middle layer called the myocardium. It contains the specialized cardiac muscle cells that do most of the work of pumping the blood around. They are different than the other muscle tissues of the body in that they are 1. More connected physically and electrically to each other. This allows the heart tissue cells to work as one. 2. Have more intracellular structures that produce energy, allowing them to work all the time. Under normal conditions and given enough supplies they will work continuously without becoming fatigued. This will become important when we talk about heart attacks.
The walls of the heart have three layers. The innermost layer is the endocardium. It covers the heart chambers and heart valves and connects to the tissue lining of the blood vessels. The outermost layer is called the epicardium which forms part of the pericardial sac that surrounds, protects, and lubricates the heart. The bulk of the heart wall is made up of the middle layer called the myocardium. It contains the specialized cardiac muscle cells that do most of the work of pumping the blood around. They are different than the other muscle tissues of the body in that they are 1. More connected physically and electrically to each other. This allows the heart tissue cells to work as one. 2. Have more intracellular structures that produce energy, allowing them to work all the time. Under normal conditions and given enough supplies they will work continuously without becoming fatigued. This will become important when we talk about heart attacks.
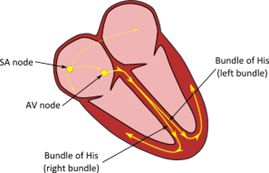 The last heart tissue that we need to talk about is the pacemaker cells. They are specialized nerve cells that are set up to fire automatically in a coordinated fashion on a set schedule. There are two bundles of them located in the right atrial chamber of the heart. The first to fire is the bundle called the sinoatrial node (SA node). It makes the atrial chamber muscle contract as one, pushing the blood into the ventral chambers. There is a small delay then the electrical signal reaches the atrioventricular node (AV node), and they fire. This signal makes the ventral muscle contract as one and they push the blood out and away from the heart. This coordination of nerve firing is essential for the regular rhythms of the heartbeat. The regular rhythm of contraction is referred to as sinus rhythm because the electrical impulses are generated by the sinus node.
The last heart tissue that we need to talk about is the pacemaker cells. They are specialized nerve cells that are set up to fire automatically in a coordinated fashion on a set schedule. There are two bundles of them located in the right atrial chamber of the heart. The first to fire is the bundle called the sinoatrial node (SA node). It makes the atrial chamber muscle contract as one, pushing the blood into the ventral chambers. There is a small delay then the electrical signal reaches the atrioventricular node (AV node), and they fire. This signal makes the ventral muscle contract as one and they push the blood out and away from the heart. This coordination of nerve firing is essential for the regular rhythms of the heartbeat. The regular rhythm of contraction is referred to as sinus rhythm because the electrical impulses are generated by the sinus node.
Pathophysiology of the Heart
Permanent damage and the new normal
 The heart and the cardiovascular system are an extremely dynamic and robust system. They can adjust easily to the changing demands of the body and quickly repair any damage that occurs. But there are limits to which the system can cope. Exceed these limits and permanent damage starts to occur. At first, you may not even notice the changes the damage is creating. Eventually, though there is so much permanent damage that it becomes debilitating and even life-threatening. Medical interventions and surgery can help compensate, but the cardiovascular system will never return to its normal functioning. In layman’s terms once you have heart disease you will always have it. You will be forced to adjust your lifestyle or face further heart troubles down the road. Helping the patient adapt to the new “normal” is what In-Home caregivers should be focused on. More about that later.
The heart and the cardiovascular system are an extremely dynamic and robust system. They can adjust easily to the changing demands of the body and quickly repair any damage that occurs. But there are limits to which the system can cope. Exceed these limits and permanent damage starts to occur. At first, you may not even notice the changes the damage is creating. Eventually, though there is so much permanent damage that it becomes debilitating and even life-threatening. Medical interventions and surgery can help compensate, but the cardiovascular system will never return to its normal functioning. In layman’s terms once you have heart disease you will always have it. You will be forced to adjust your lifestyle or face further heart troubles down the road. Helping the patient adapt to the new “normal” is what In-Home caregivers should be focused on. More about that later.
Types of Heart Disease
Heart disease is a general all-inclusive term that includes a range of conditions that results in heart problems. It's also called cardiovascular disease, which means heart and blood vessel disease.
Heart disease includes:
- Congenital Heart Disease (CHC)
- Coronary artery disease
- Irregular heartbeats (arrhythmias)
- Heart valve disease
- Diseases of the heart muscle (cardiomyopathy)
- Heart Failure
Congenital Heart Disease
Congenital Heart Disease is also a general term for patients who have one or more defects in the heart’s structure since birth. Its symptoms range from mild to life-threatening and can alter the way blood flows through the heart. Problems resulting from these defects can appear at the moment of birth or may only manifest themselves later on in life. Common congenital heart disease symptoms in adults include:
|
 |
For some people, the signs or symptoms of congenital heart disease aren't noticed until adulthood. It is also possible that symptoms may return years after a congenital heart defect is treated. Once diagnosed, patients will require at the very least regular doctor checkups. Most likely though, lifelong medication use or even surgery will be needed.
Coronary Heart Disease
Coronary Heart Disease also known as Coronary Artery Disease (CAD), is the most common form of heart disease. CAD occurs when the walls of coronary arteries supplying the heart become hardened and narrowed. This reduces the hearts’ ability to work hard and makes it easier to have a heart attack or stroke. It almost always occurs because of a buildup of fatty plaque on the walls of the arteries.
To understand why the plaque starts to build up you must first know that this is a long slow process that may take years to develop. First, the arterial wall is damaged because of things like prolonged high blood pressure. Inflammation occurs as part of the repair process. Too much exposure to inflammation can cause greater damage to the inner arterial wall. This creates a place where fatty material like lipids and cholesterol can stick and collect. If the harmful condition persists the plaque continues to build until the passageway is narrowed.
A person with plaque buildup will mostly not feel any adverse effects, but…. Plaque is not a durable material. Bits of plaque can break off and lodge downstream in narrower arteries. The plaque can also burst, accidentally setting off the clotting process inside the artery. The result is a blocked flow of vital nutrients like oxygen and the rapid build-up of toxic waste material. Cells will start to die. If it happens in the brain, you have a stroke. If it happens in the heart, you have a heart attack.
The following video is for the advanced reader. There will not be any test questions on it. For those who brave it anyway, you will see it is an excellent visual explanation of the clotting cascade of a heart attack.
The signs and symptoms of CAD depend on where the arteries are narrowed. For example- pain, numbness, weakness, or coldness in the legs or arms may be the result of the narrowing of the arteries in the limbs.
If a coronary artery is totally blocked, every cardiac cell downstream is going to be in a world of hurt. Kill off enough cardio muscle and the heart will stop functioning. You know what suddenly follows after that.
The outward signs of a heart attack are:
- Chest pain or discomfort. Most heart attacks involve discomfort in the center or left side of the chest. It lasts for more than a few minutes or goes away and then comes back. The discomfort can feel like uncomfortable pressure, squeezing, fullness, or pain.
- Feeling weak, light-headed, or faint. You may also break out into a cold sweat.
- Pain or discomfort in the jaw, neck, or back.
- Pain or discomfort in one or both arms or shoulders.
- Shortness of breath. This often comes along with chest discomfort, but the shortness of breath also can happen before chest discomfort.
Source https://www.cdc.gov/heartdisease/heart_attack.htm
If the coronary artery is only partially blocked, the heart can continue to beat. But there will still be problems. Men and women may experience different coronary artery disease symptoms. Studies have shown men are more likely to have chest pain. While women are more likely to have other symptoms along with chest discomfort, like shortness of breath, nausea, and extreme fatigue.
Angina is a type of chest pain caused by a reduced flow of blood in the heart. Angina sufferers describe it as a feeling of squeezing, pressure, heaviness, tightness, or pain in the chest. It may also feel like a heavy weight lying on the chest.
Angina is not a heart attack, but it is often a precursor to it. There are different types depending on the cause and whether rest or medication relieves symptoms. Being familiar with the different types gives caregivers important clues as to how to react to the situation and what to report to the doctor or emergency medical personnel.
Types of Anginas
|
Stable angina. |
The most common form of angina. It usually happens during activity (exertion) and goes away with rest or angina medication. For example, pain that comes on when walking uphill or in cold weather. Stable angina pain is predictable and usually similar to previous episodes of chest pain. The chest pain typically lasts a short time, perhaps five minutes or less. Record events and look for long term patterns of frequency or severity |
|
Unstable angina (a medical emergency) |
Unstable angina is unpredictable and occurs at rest. Or the angina pain is worsening and occurs with less physical effort. It's typically severe and lasts longer than stable angina, maybe 20 minutes or longer. The pain doesn't go away with rest or the usual angina medications. If the blood flow doesn't improve, the heart is starved of oxygen and a heart attack occurs. Unstable angina is dangerous and requires emergency treatment. Call 911 |
|
Variant angina (Prinzmetal angina) |
It's caused by a spasm in the heart's arteries that temporarily reduces blood flow not caused by CAD. Severe chest pain is the main symptom of variant angina. It most often occurs in cycles, typically at rest and overnight. The pain may be relieved by angina medication. |
|
Refractory angina |
Angina episodes are frequent despite a combination of medications and lifestyle changes. Standing orders from the doctor may be required |
Source https://www.mayoclinic.org/diseases-conditions/angina/symptoms-causes/syc-20369373 italic material added.
Arrhythmias
Arrhythmias are any sequence of nerve cells firing that causes a heart rhythm that is not a normal sinus rhythm. It can be a single extra beat causing a palpitation to a quick uncoordinated firing causing a heart chamber to quiver.
Some related terms you might have heard are;
- Bradycardia- Slow heartbeat
- Tachycardia- Fast heartbeat
- Fibrillation- Irregular heartbeats, often very fast
- Atrial Flutter- Regular fast contraction of the atria heart chambers
- Heart Block- The electrical signal that controls the heartbeat is partially or completely blocked.
Here is a quick video on arrhythmias
Arrhythmias can be continuous or intermittent. Sporadic irregularities can be difficult for the doctor to diagnose. They usually occur when the doctor is not listening or performing a medical recording of heartbeats. Both typically last for just a few seconds. A 30-day heart monitor may be worn by the patient. It will give the doctor a greater source of data that will help in assigning a diagnosis.
The factors that can contribute to arrhythmias include heart disease, high blood pressure, diabetes, smoking, heavy alcohol use, an electrolyte imbalance, drug abuse, and stress. Certain medications, herbs, and dietary supplements can also cause or aggravate the condition.
Irregular heartbeats can lead to irregular blood flow. Irregular blood flow increases the chance of unwanted blood clots that can cause significant harm. It is not uncommon for blood thinners to be prescribed in such cases as a preventative measure.
Arrhythmias also may or may not be felt by the patient. Hear again intermittent occurrences can cause a lot of fear and anxiety in the patient. In-Home caregivers can be of calming assistance by
- Keeping good records of occurrences and passing the info on to the doctor.
- Advocate for the need for a cardiac specialist.
- Assist with any specialized equipment used.
- Monitoring for irregularities
- Providing a safe environment that lessens the risks of injury from fainting
Real World example. Recently my mother-in-law was plagued by fainting spells. Her regular doctor was at a loss, blaming it on a side effect of her medication. The condition worsened and she was hospitalized. She even fainted while in the hospital. Finally, I moved her into my home and got her to see a cardiologist. He placed a 30-day monitor on her that was connected remotely to the internet. He was able to see the data from his office. After the thirty days were over, he was able to notice an arrhythmia that was occurring only 3% of the time. He called it a sick sinus syndrome caused by her natural pacemaker cells not firing or being blocked. He told us that it was a common condition resulting from the aging process. He surgically implanted an artificial pacemaker and said she was good for 10 years, after which the battery would need to be replaced.
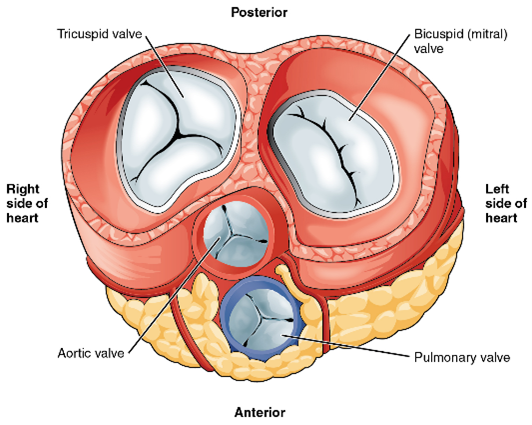
Your heart has four valves leading in or out of the heart chambers. If one or more doesn’t work well, you have Heart Valve Disease. You can be born with the defect (congenital) or it may develop over time as a result of aging or other damaging effects. Defective heart valves that develop later in life are usually associated with heart murmurs. It may cause a swooshing sound that is heard when listening with a stethoscope.
Heart valves can have three basic kinds of problems:
|
Regurgitation, or backflow, happens when the flaps of a valve don't close tightly. This allows the blood to leak backward. A common cause of regurgitation is prolapse, where the flaps of the valve flop or bulge back. Prolapse most often affects the mitral valve. |
|
Stenosis happens when the flaps of a valve become thick, stiff, or stuck together. This prevents the heart valve from opening all the way. Not enough blood can pass through the valve. Aortic valve stenosis is a common type of stenosis. It affects the valve that controls blood flow into the large artery that carries blood out of the heart to the body. |
|
Atresia happens when a heart valve did not form properly and does not have an opening for blood to pass through |
Sometimes a valve can have both regurgitation and stenosis.
Source: https://medlineplus.gov/heartvalvediseases.html
Heart valve disease can be treated by symptom reduction through lifestyle changes or medication. The valve can also be replaced or repaired through surgery.
Cardiomyopathy
Cardiomyopathy refers to a collection of disease conditions of the heart muscle tissue. It can alter the shape and reduce the function of the heart, especially the walls of the heart chambers. You may have heard stories about enlarged hearts, that is cardiomyopathy.
Watch this video for a quick overview.
Cardiomyopathy can either be inherited or caused by outside factors like alcohol abuse or infections. The condition tends to get worse over time, sometimes very quickly, and it can affect young children. It is a major contributing factor to other heart conditions like heart failure.
Heart Failure
Though the heart is robust and able to repair itself, permanent damage can and does happen. When damage occurs, the body will do things to compensate for the shortfall of function. If the unhealthy condition continues, even these measures will stop working. Eventually the heart starts to fail in its function to pump an adequate amount of blood around the body. This condition is simply called heart failure.
In heart failure the heart has not stopped, it is just not working well enough to meet the needs of the body. The overview is simple enough, but the details can be very complex. If you did an internet search on heart failure you would find it described as an ongoing problem (chronic) or it could happen suddenly (acute). It could be a right-sided failure (the heart is too weak to pump enough blood to your lungs to get oxygen). It could be the more common left-sided failure (the heart can't pump enough oxygen-rich blood out to your body). Or it could be both at the same time. It could be described as Diastolic (improper filling in the heart chambers- vs- Systolic (can’t pump hard enough). There are even math equations involved in describing heart failure (ejection fraction). We are going to let the doctors and nurses worry about all that and we’ll concentrate on what is important to In-home caregivers. How to recognize the symptoms and what to do about them.
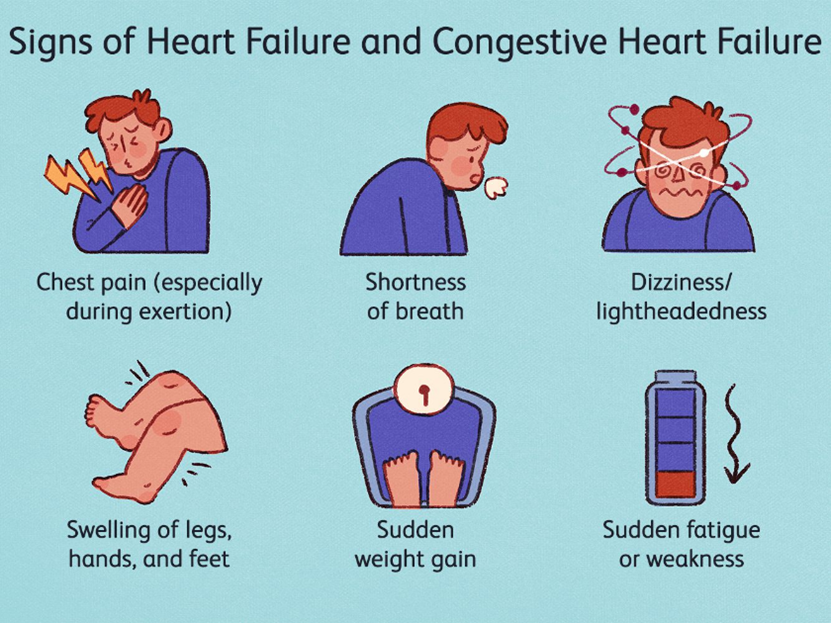
When the heart can’t pump well, blood builds up in the blood vessels. Excessive fluids leaks into the surrounding tissues. The fluid starts to accumulate and how it shows as symptoms depend on which side of the heart is affected. Remember the anatomy lesson from earlier in the course. In right-sided heart failure, the blood can’t move from the body into the heart, so swelling of extremities and organs occurs. In left-sided heart failure, the fluid backs up into the lungs, and signs of drowning slowly start to show. It is easy to understand why heart failure is also called congestive heart failure (CHF). Though left-sided heart failure is more common, it often leads to right-sided heart failure as well.
The common signs and symptoms of CHF are:
- Feeling short of breath, while doing normal activities or lying down. This may be one of the first symptoms caregivers will notice.
- Fatigue or weakness even after rest.
- Coughing or wheezing with white or pink blood-tinged mucus.
- Crackling sound when breathing (Rales)
- Swelling in the abdomen and rapid weight gain
- Pitting edema from fluid in the ankles and lower legs.
- Difficulty sleeping when lying flat.
- Nausea and loss of appetite.
- Swelling in the veins of the neck.
- Needing to urinate often.
- Angina
- Difficulty in concentrating or decreased alertness
If you as a caregiver starts to see a collection of the above symptoms, it’s time to get your resident to the doctor. The doctor will probably ask you to modify the resident’s lifestyle and add heart medications, more about that later. If these measures seem to fail, then either a ventricular assist device (VAD) or a heart transplant may be needed.
Identifying the Problem
In-home caregivers are the first point of contact for the medical establishment at large. Often it is your observations that initially identify health problems that may have gone unnoticed, were misdiagnosed, or started to develop in the residents under your care. Knowing the risk factors and the common sign and symptoms of heart disease will help you focus your attention on where it needs to be.
Risk Factors
Not everyone develops heart disease. There are medical conditions, lifestyle choices, and family genetics that can increase the risk of having cardiac problems. Understanding why certain factors increase that risk will make it easier for caregiver to spot potential problems sooner.
- High Blood Pressure- The long-term stress of high blood pressure in the cardiovascular system damages the arteries and organ tissues of the body. Arterial walls and the myocardium lose their elasticity and become stiff leading to loss of function. Damaged arterial walls create surfaces that make it easier for cholesterol or other fatty substances to attach, forming plaques and further reducing blood flow.
- High Cholesterol Levels- Cholesterol is a lipoprotein. A waxy, fat-like molecule made by the liver. It can also be found in certain foods we eat. It is used by the body for many functions. There are different types of Cholesterol. LDL (low-density lipoprotein) is considered to be bad because it can cause plaque to form. Think of it as a fluffy cotton ball that sticks in the arteries and cuts off blood flow. HDL (high-density lipoprotein) is good cholesterol because it can scoop up LDL and therefore protects the heart.
- Diabetes- Diabetics can have higher levels of glucose in the bloodstream. Glucose is a very reactive molecule. Glucose molecules can easily attach themselves to other molecules, disrupting their function and causing damage to structures in the cardiovascular system.
- Obesity- Those who are extremely overweight are more likely to have multiple contributing heart disease risk factors. Including high LDL, low HDL, diabetes, high blood pressure, and lower activity levels.
- Unhealthy Diets- Eating foods with high levels of saturated fats, trans fat, and cholesterol only increases their levels in the bloodstream. Foods high in salt increase the water level in the bloodstream (water follows salt). This leads to increased blood pressure. Refined carbohydrate food like bread and pasta leads to higher levels of glucose and increases the chance of diabetes.
- Lack of physical activity- Inactivity leads to reduced muscle tone and less capable muscles in the heart and blood vessels. It also contributes to diabetes, obesity, and high blood pressure.
- Alcohol- Too much alcohol can raise blood pressure, increase levels of triglycerides (a fatty molecule found in plaques) and damage the fine tissues of the cardiovascular system
- Tobacco- Cigarette smoke contains harmful substances that damage the heart, lungs, and blood vessels. Nicotine increases blood pressure and hardens arteries. Carbon monoxide reduces the amount of oxygen in the blood.
- Stress- Our body responds to stress by increasing blood pressure and heart rate. Too much stress can damage the heart.
- Genetics- Defects in the cardiovascular system can be inherited. Heart disease in family members is important information to obtain.
- Age and Gender- Tissue deterioration increases with age. The older you get the higher the risk of the structures of our bodies just wearing out. Starting at age 45, a man’s risk of heart disease begins to rise, while a woman’s risk begins to increase at age 55 (post-menopause).
- Medical Conditions- Other pathologies can aggravate or weaken the cardiovascular system. A caregiver should increase their monitoring of cases of Chronic kidney disease, Autoimmune and inflammatory disease, Chronic pain conditions, or Infections like rheumatic fever and measles.
- Medications- Harmful side effects are always a risk in medications. Watch for heart or blood pressure problems with the following drugs.
- Nonsteroidal anti-inflammatory drugs
- α1-blockers
- Antimalarial agents
- TNF-α inhibitors
- Antineoplastic agents.
- Oral Antifungal medications.
- Minoxidil
- Cocaine
- Anabolic Steroids
- Amphetamines (uppers)
Care home operators know their residents more intimately than any other medical professional. Who is better placed to notice abnormalities that may develop? In-home caregivers are not responsible for diagnosing heart diseases. You are responsible though in recognizing problems that need medical attention. That includes suspecting misdiagnoses when things just don’t add up right, (doctors are human too). Various pathological conditions have their own set of heart disease symptoms. You don’t have to worry about such fine details. You need to focus on what looks suspicious and report it to the doctor.
Keep a look out for:
- Chest pain, chest tightness, chest pressure, chest discomfort, and sweating
- Shortness of breath
- Pain in the neck, jaw, throat, upper belly area, or back
- Pain, numbness, weakness, or coldness in the legs or arms
- Wheezing or crackly breaths
- Difficulty sleeping while flat on their back or waking up early with feelings of breathlessness. Requests to be propped up with extra pillows
- Pitting edema (when poked with a finger an indentation remains)
- Complaints of weakness or difficulty completing normal activities
- Fainting or dizzy spells
- Complaints of palpitations (pounding, racing, or fluttering heartbeats)
-
Unexplained quick weight gain and or increases in girth around the stomach - Large neck veins (Jugular Vein Distention)
- Increase in nighttime urination
- Pale grey skin or blue-tinged lips or fingertips
- Unexplained wet-sounding cough
- Frequent nausea
- General complaints of feeling unwell or ill at ease
- Pains felt deep in the legs (deep vein thrombosis)
Feeling for irregular heart rate.
Place two fingers on either side of the windpipe or in the groove neck to the bone just below the wrist. Check your own pulse to get a feeling of what is normal then check the resident.
If you are unsure if you could feel an irregular heart rate check this video out.
High Blood Pressure
Taking blood pressures at home has become easier with advancements in automatic blood pressure machines. Due to natural variations in conditions, you never get excited about single readings. In-home caregivers need to concern themselves with changes in patterns over time.
|
|
Systolic |
Diastolic |
|
Normal |
Less than 120 |
Less than 80 |
|
Prehypertension |
120-139 |
89-89 |
|
Hypertension |
140 or higher |
90 or higher |
High Cholesterol
You can buy over-the-counter cholesterol tests, but I think it’s a waste of your time and money. The county regulators would probably frown on the idea and the doctor would take his or her own tests anyway. Caregivers can ask for copies of the doctor’s test or even see them online now.
Cholesterol levels indicating high risk
|
|
Good |
Bad |
|
HDL |
More than 60mg/dL |
Less than 40mg/dL |
|
LDL |
Less than 100mg/dL |
More than 160mg/dL |
|
Total Cholesterol |
Less than 200mg/dL |
More than 240mg/dL |
So you have seen enough bad signs to start having suspicions. Now what do you do? Just calling the primary care physician is ok but you are a professional. You need to take it up a notch. Trust me on this. Care provider efforts put in here will give you great benefits down the road. Your reputation will grow. Working with the doctor will get easier. You will get faster results. Your resident and their family will trust you more and you will experience fewer problems in caregiving. To achieve these benefits, I recommend the following.
- Make a record of your observations. Things in writing are unusual and are paid attention to.
- If you know what you are doing, use medical terminology. Buy yourself a medical dictionary if you have to.
- Include measurements. Doctors are scientists by training and they like lots of data. Measurements can be a little as the frequency of occurrence of symptoms. For example, had dizziness for about a minute upon standing three times this week and had fainting spells twice this month. Increase in weight of 10lbs in one week. Had to use 2 extra pillows at night to help in sleeping comfortably. B/P while sitting was 140/90, 148/92, 150/90 taken just after breakfast.
- Ask lots of questions. If you have suspicions phrase them in the form of a question. Do you think the wheezing I hear is from congestive heart failure? Can this fainting be caused by arrhythmia? Can these complaints about chest heaviness be angina? (see what I did there with the medical terminology?)
- Develop a partnership with the doctor. Ask him what he needs to help him do his job. If you need things yourself do not hesitate to ask.
- Let the patient answer the questions. The doctor is used to working one on one directly with the patient. Do not be overbearing or condescending toward the patient, it makes you look bad. You may have to supply clarifications or missing info though. Come on too strong and the doctor will get annoyed with you.
- Make friendly comments to the doctor’s staff. Joking with the staff creates a cooperative environment while keeping things respectful with the doctor.
- Strive for understanding. Keep communicating until everyone is comfortable with what is going on. Translate medical jargon into everyday language for the patient. Parrot back to the doctor what you think he or she means about key points and instructions. This will help to ensure you are understanding things correctly and show that you are taking the matter seriously.
- When calling the doctor's office, it is easier to talk directly with the nurse than it is with the doctor. Working just with medical assistants is questionable at best. If it is important, ask for a call back from the doctor or at the least insist on talking with a nurse.
Pushing for a specialist
Becoming a partner with the primary care physician (PCP) is all well and good, but sometimes you got to go beyond them and get a specialist. Cardiologists are the experts when it comes to all things heart-related. They know all the subtleties of symptoms and the tricks of treatments. They will work with you and help your resident have as normal a life as possible despite their heart problems. As the advocate for your resident that is what you are supposed to do.
Real-world example. Do you remember the story about my Mother in law’s heart problem from earlier in the course? I knew that something was amiss medically, but I lived an entire state away and couldn’t do much. I finally got fed up and took the time to go where she lived. I thought I could work with the doctor and fix things. Frustratingly, the doctor was entrenched in thinking the problem was caused by a drug side effect. I gave up. When I moved her here, I got her a new PCP and told him everything. The first thing he did was to get her to a Cardiologist. I was skeptical at first, thinking “great a totally new guy I have to work with”. I was a tad bit tired of doctors by this point. Well, you know the rest of the story. After doing the research for this CE course, I now know that the cardiologist knew all the right tests to use to make the correct diagnosis. I could have saved so much effort and worry if I’d known that while working with the first doctor. Sometimes hindsight can slap you right in the face and wake you up.
Testing for Heart Disease
 I hope that you can see that even an old dog like me can learn new tricks. Rarely does the outward signs point to an obvious conclusion. Usually, more tests are required to locate the hidden signs that can change the diagnosis. But nobody likes going to the doctor and taking more tests. If you have a fearful or uncooperative resident, reassure them that most screening tests for heart disease are done outside of the body and are painless. Tell them that the more information a doctor has the better decisions they can make.
I hope that you can see that even an old dog like me can learn new tricks. Rarely does the outward signs point to an obvious conclusion. Usually, more tests are required to locate the hidden signs that can change the diagnosis. But nobody likes going to the doctor and taking more tests. If you have a fearful or uncooperative resident, reassure them that most screening tests for heart disease are done outside of the body and are painless. Tell them that the more information a doctor has the better decisions they can make.
The doctor may choose to give one or more of the following tests:
- Electrocardiogram (ECG or EKG) makes a graph of the heart’s electrical activity as it beats. This test can show abnormal heartbeats, heart muscle damage, blood flow problems in the coronary arteries, and heart enlargement.
- Stress test (or treadmill test or exercise ECG) records the heart’s electrical activity during exercise, usually on a treadmill or exercise bike. If you are unable to exercise due to arthritis or another health condition, a stress test can be done without exercise. Instead, you can take a medicine that increases blood flow to the heart muscle and shows whether there are any problems in that flow.
- Nuclear scan (or thallium stress test) shows the working of the heart muscle as blood flows through the heart. A small amount of radioactive material is injected into a vein, usually in the arm, and a camera records how much is taken up by the heart muscle.
- Echocardiography changes sound waves into pictures that show the heart’s size, shape, and movement. The sound waves also can be used to see how much blood is pumped out by the heart when it contracts.
- Coronary angiography (or angiogram or arteriography) shows an x-ray of blood flow problems and blockages in the coronary arteries. A thin, flexible tube called a catheter is threaded through an artery of an arm or leg up into the heart. A dye is then injected into the tube, allowing the heart and blood vessels to be filmed as the heart pumps. The picture is called an angiogram or arteriogram.
- Ventriculogram is frequently a part of the x-ray dye test described before. It is used to get a picture of the heart’s main pumping chamber, typically the left ventricle.
- Intracoronary ultrasound uses a catheter that measures blood flow. It creates a picture of the coronary arteries that shows the thickness and other features of the artery wall. This lets the doctor see blood flow and any blockages.
- Carotid doppler ultrasound uses sound waves to detect blockages and narrowing of the carotid artery in the neck, both of which can signal an increased risk for heart attack or stroke.
- Electron-beam computed tomography is a superfast scan that provides a snapshot of the calcium buildup in your coronary arteries.
- Magnetic resonance imaging (MRI) is a scan using magnets and computers to create high-quality images of the heart’s structure and functioning. It is often used to evaluate congenital heart disease. The test can also detect severe blockages in coronary arteries in people who are having unstable angina or a heart attack, thereby allowing immediate treatment to restore blood flow to the heart.
- Holter monitoring. A Holter monitor is a portable ECG device that's worn for a day or more to record the heart's activity during daily activities. This test can detect irregular heartbeats that aren't found during a regular ECG exam.
Source: https://www.nhlbi.nih.gov/files/docs/public/heart/living_well.pdf
In-Home Caregiving for Heart Disease
When someone experiences bad news, it is only human to complain “Why Me!” Barring bad luck events like the defective genes you were born with; the usual answer is, “because you made too many risky choices and now it’s catching up to you”. If you want to avoid bad consequences make good choices. If the damage has already happened, then stop doing the things that will make a bad situation worse. In-home caregivers are in the perfect position to turn things around for the resident with heart disease.
Modifying risk factors
 Smoking- As we have already covered, smoking puts stress on the heart in many ways. Care homes need to have clearly written anti-smoking policies. If you have to allow smoking, (mental health patients often use nicotine as self-medication therapy so it’s really hard to stop) then you have to control the secondhand smoke. If the caregivers themselves smoke, then you are opening yourself up to “caused harm to heart disease patient” lawsuits.
Smoking- As we have already covered, smoking puts stress on the heart in many ways. Care homes need to have clearly written anti-smoking policies. If you have to allow smoking, (mental health patients often use nicotine as self-medication therapy so it’s really hard to stop) then you have to control the secondhand smoke. If the caregivers themselves smoke, then you are opening yourself up to “caused harm to heart disease patient” lawsuits.
If you or a resident are trying to quit, the number one recommendation I can make is to make the environment extremely uncomfortable to smoke in. No comfy chairs to sit in, no ashtrays (make them dig for an old can in the garbage) no after-dinner smoking sessions. The good news is that quitting smoking will immediately and significantly reduce the risk of further heart disease complications.
High Blood Pressure (HBP)- You can’t feel HBP until after it’s too late. You have to rely on BP monitoring and take HBP readings seriously. Taking your resident's BP regularly might not be a bad idea. If you do, keep a record of the readings and let the doctor see it periodically.
You can reduce HPB by:
- Losing weight, Just 5-10% weight loss starts to protect the heart.
- Exercising, In a care home, start by taking scheduled walks. Work up to 30 minutes on most days.
- Stop drinking alcohol
- Reduce salt intake- The Dash diet might be worth looking into.
Here is a good intro to the Dash Diet
High Cholesterol
You lower cholesterol blood levels by eating healthier, period ‘nuff said.
Cook from scratch. It’s cheaper (more profitable), looks good to potential new clientele, and makes the current residents more satisfied with staying in your home. It doesn’t take any talent. It just takes practice, planning, and shopping for the right foodstuffs. Include foods high in fiber, but low in saturated fat, trans fat, total fat, and cholesterol. The days of deep-fried pig fat on a stick are gone. Fat may be flavor, but it’s also pain and misery to heart disease sufferers.
If you want to take a short cut, look into the DASH diet. It will cover reduced salt and fats. Here again, the key to easy implementation starts with buying the right foodstuffs. Make a menu then use what is on it to make a shopping list.
Stress
Moving into your home and dealing with change can be stressful for the resident. But after that, a reduced stress environment is totally doable. I recommend concentrating on creating clean, tidy and quiet surroundings, and a stable predictable schedule. Predict stressful situations and take steps to prepare for them. And for heaven’s sake, reduce the number of choices that a resident has to make.
Fluids
Proper hydration is important, but you don’t want to aggravate the pathophysiology of congestive heart failure, high blood pressure, or any severe heart disease condition. If you have residents with any of these disorders consult with the doctor about how much fluids to give. Don’t forget what’s on the menu when totaling fluid intakes.
It probably wouldn’t be a bad idea to weigh the patient regularly and put a cloth tape measurer around the waist every so often. An increase of 2-3 lbs a day or 5 lbs a week are red flags and the doctor needs to be notified. Record the info and give it to the doctor when needed.
Sleep disturbances are a red flag in heart disease patients, especially congestive heart failure. The extra fluids easily flow into the lungs when lying flat. The extra fluid can also pool in the kidneys, increasing the need for nighttime urination. Extra pillows can help but foam wedges are better. I have even heard of caregivers putting the head of the bed on bricks to angle up the entire bed.
Complaints
Pay attention to complaints and don’t dismiss them out of hand. Complaints may be caused by new symptoms or worsening conditions that are starting to manifest themselves.
Misc.
- The more ill a patient is, the greater the need to get all their shots.
- Control diabetes and you control heart disease and vice versa. The therapies overlap each other considerably
- Mini Pedalers and hand weights are an easier-to-use exercise option in care homes. Consult with the doctor before anything strenuous.
- All of the above measures could be utilized for the entire household as part of a heart disease prevention strategy.
Heart Disease Therapy
Medications
There are a wide variety of medications that a prescriber can utilize in heart disease therapy to control risk factors or reduce symptoms. To make it easier for you we will list them by drug class. But first, you need to know some pharmacology terms and you also need to remember some of the stuff we covered in the anatomy and physiology sections.
- Vasodilators- drugs that reduce blood pressure by opening up the blood vessels. They usually do this by relaxing the smooth muscle that constricts around the vessel. A common side effect is orthostatic hypotension (the dizziness and falling side effect)
- Orthostatic hypotension (OH) or postural hypotension- Blood rushing away from the brain when you stand or sit up. The remedy is getting up slowly or in stages, pausing in between actions.
- Vasoconstriction- Tightening of the smooth muscle around blood vessels. Naturally the result of a nerve impulse.
ACE inhibitors
Vasodilator with names often ending in -pril (lisinopril). They work by stopping the body from producing a chemical that narrows blood vessels. It lowers HBP, reduces heart attacks, heart failures, and protects the kidneys in diabetes. Helps excrete some sodium. Watch for OH. May cause a constant dry cough.
ARBs Angiotensin II Receptor Blocker
Works similar to an ACE but with no cough.
Beta Blockers
Blocks the effect of epinephrine and norepinephrine causing the heart to beat more slowly and with less force, which lowers blood pressure. Also is a Vasodilator. Used to treat HBP, arrhythmias, and anginas and reduces the chance of a heart attack. Watch for OH. Their names can end in -olol (metoprolol)
Calcium Channel Blockers
Helps block the signal that causes certain nerves to fire. Reduces vasoconstriction and slows the heart. Used to treat HBP, arrhythmias, and anginas and reduces the chance of a heart attack. They are vasodilators so watch for OH.
Diuretics (water pills)
Drugs used to fight fluid buildup. Lowers HBP and reduces pitting edema. Loop directs like Lasix may cause low potassium problems like confusion or leg cramps. Diuretics may work too well so watch for dehydration signs. Giving them later in the day will cause extra urination at night so dispense them in the AM. Watch for OH
Digitalis
Helps the heart beat stronger and slower. Lots of side effects and interactions with other drugs. Watch for Nausea and Vomiting. If the resident starts to have vision changes like yellow or greenish halos, stop the digitalis and call the doctor right away.
Anticoagulants and antiplatelets (blood thinners)
Prevents harmful blood clots. Used to reduce heart attacks and angina. Includes low-dose aspirin and warfarin also called the bruiser med. Be prepared to deal with ugly bruises at the mere grip of the wrist or brush of the skin. If there is too much bruising call the pharmacy or doctor. The dose might be too high. Might have to watch the consumption of certain foods like grapefruit.
Drugs that relax blood vessels and promote blood flow by breaking down into Nitric Oxide. Used to prevent heart attacks and relieve angina. Nitroglycerin can evaporate from pills if left out or place under heat. If the pills don’t tingle when used, they have lost their potency. Can cause major headaches. Used as a rescue med, the dosage is prn pain, up to 3 times- 5 minutes apart before calling 911. There may be new guidelines coming out so talk to the doctor.
Cholesterol-lowering drugs
Drugs that lower LDL but sometimes may increase HDL. A popular family of these meds are the satins like atorvastatin (Lipitor). They may cause muscle pain or weakness. Call the doctor if it happens. May also cause memory loss in certain patients. Grapefruit will interfere with statins.
Managing angina can be summed up in a single sentence, “avoid the triggers”. Triggers are anything that makes the heart work harder. Common activities notorious for causing angina pain are a sudden increase in physical activity, emotional stress, cold weather, eating a big meal, high blood pressure, being overweight, cigarette smoking, and long bouts of constipation strain. Combining harmful activities like going out in cold weather after the thanksgiving feast or holding your breath while lifting is a no-no. Caregivers should start exercise programs gradually. If angina is occurring frequently, keeping an angina diary will help identify potential triggers to avoid in the future.
Heart attack Management
I know that most of you have had CPR training, so I’ll just put up a reminder list of heart attack warning signs.
- Chest discomfort or angina
- Discomfort in the arms, back, neck, jaw, or stomach
- Shortness of breath
- Lightheadedness
- Breaking out in a cold sweat
Surgery
Surgery as therapy is essentially modifying the problem areas of the cardiovascular system. They may include:
- Coronary Angioplasty (“Balloon” Angioplasty)- inflating a tiny balloon in an artery to increase blood flow.
- Plaque Removal- atherectomy (shaving off the plaque) or laser angioplasty (burning off the plaque)
- Stent Placement- inserting a tiny wire mesh to keep the artery open.
- Coronary Bypass Surgery- basically replumbing around the problem area.
Cardiac Rehabilitation
Cardiac Rehabilitation is a supervised program that includes a team of specialists working on all aspects of heart disease recovery. The team includes the doctor's office, exercise and nutrition specialists, physical therapists, and counselors. In-home caregivers should find out who’s in charge and fight to be included in the program. You might have to do some educating to let them know who you are and what you can do. I recommend that you tell them that you are the superman of facilitation and the captain of get ‘er done.
Conclusion
Heart disease can drastically alter the life of your residents. Your goal as the In-Home caregiver and patient advocate is to do what is necessary to help the resident return to as normal life as possible. You can help them understand what is going on and what things they need to do. You can help them manage their therapy, medication, and lifestyle choices. You can also provide a supportive stress-free environment to live in, which might be the most important thing that you can do.
As always, Good Luck in your caregiving efforts.
Mark Parkinson BsPharm
References:
- Heart Disease. MayoClinic.org. Oct/22 https://www.mayoclinic.org/diseases-conditions/heart-disease/symptoms-causes/syc-20353118
- An Osmosis Video: Congestive Heart Failure (CHF) Explained. Osmosis, Jun 21, 2016. https://www.youtube.com/watch?v=ypYI_lmLD7g
- Congestive Heart Failure (CHF) Pathophysiology, Nursing, Treatment, Symptoms | Heart Failure Part 1. RegisteredNurseRN, Aug 12, 2016. https://www.youtube.com/watch?v=HoN2EmBJXBk
- Mike Linares RN. Congestive Heart Failure (CHF) for Nursing & NCLEX. Simple Nursing. Sep 1, 2019. https://www.youtube.com/watch?v=uuXJNJ9LvdM
- Vishal Punwani. What is coronary artery disease? | Circulatory System and Disease | NCLEX-RN | Khan Academy. Khanacademymedicine, Oct 22, 2014 https://www.youtube.com/watch?v=EATkbpqlxvc
- Heart Diseases. Medlineplus, NIH, National Library of Medicine, Sep/22. https://medlineplus.gov/heartdiseases.html
- What is Cardiovascular Disease?. American Heart Association May 31, 2017. https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease
- Heart Disease Deaths. National Center for Health Statistics, Centers for Disease Control and Prevention, Aug 12, 2022. https://www.cdc.gov/nchs/hus/topics/heart-disease-deaths.htm
- Stephen L Kopecky MD. Ask Mayo Clinic: Coronary Artery Disease. Mayo Clinic Feb 11, 2022. www.youtube.com/watch?v=hE8xXevzcGE
- Congenital Heart Disease in Adults. MayoClinic.org, Aug/22. https://www.mayoclinic.org/diseases-conditions/adult-congenital-heart-disease/symptoms-causes/syc-20355456
- Living with Arrhythmias: What to Know When Your Heart is Out of Rhythm. Alliance for Aging Research, May 15, 2019. https://www.youtube.com/watch?v=_1buRmYJr0Q
- Congestive Heart Failure and Heart Disease. WebMD, August 20, 2022. https://www.webmd.com/heart-disease/guide-heart-failure
- Heart Failure. MayoClinic.org Oct/22. https://www.mayoclinic.org/diseases-conditions/heart-failure/symptoms-causes/syc-20373142
- Heart Attack Symptoms, Risk, and Recovery. National Center for Health Statistics, Centers for Disease Control and Prevention, July 12, 2022. https://www.cdc.gov/heartdisease/heart_attack.htm
- Heart Failure. Medlineplus, NIH, National Library of Medicine, Sep/22. https://medlineplus.gov/heartfailure.html
- Heart Valve Diseases. Medlineplus, NIH, National Library of Medicine, Sep/22. https://medlineplus.gov/heartvalvediseases.html
Exam Portal
click on [Take Exam]
Purchase membership here to unlock Exam Portal.
|
|
|
|
|
*Important*
Registration and login is required to place your name on your CE Certificates and access your certificate history.
Username MUST be how you want your name on your CE Certificate.
| Guest: Purchase Exam |
































 One trick I heard of is giving a baby doll to take care of. The doll can become real in a sense and have a great calming effect. Some memory care units even have baby stations.
One trick I heard of is giving a baby doll to take care of. The doll can become real in a sense and have a great calming effect. Some memory care units even have baby stations.








 When I was operating my own adult foster care homes there was one medication that constantly resulted in uncomfortable questions for county health officials, Warfarin (Coumadin). Warfarin is comely known as a blood thinner, we called it the bruiser medication. Blood thinners reduce the chances of dangerous internal blood clots that can cause a lot of damage. They also make it easier for minor cuts and abrasions to bleed profusely on the inside and outside. If an elderly resident bumped into the door a little too hard, a rather large bruise would inevitably form. It made it look like we took a bat and beat up the resident. Not a good look for a care home. It always resulted in abuse questions. Blood thinners are a high maintenance drug class that requires the In-Home caregiver to manage the patient and medication- carefully.
When I was operating my own adult foster care homes there was one medication that constantly resulted in uncomfortable questions for county health officials, Warfarin (Coumadin). Warfarin is comely known as a blood thinner, we called it the bruiser medication. Blood thinners reduce the chances of dangerous internal blood clots that can cause a lot of damage. They also make it easier for minor cuts and abrasions to bleed profusely on the inside and outside. If an elderly resident bumped into the door a little too hard, a rather large bruise would inevitably form. It made it look like we took a bat and beat up the resident. Not a good look for a care home. It always resulted in abuse questions. Blood thinners are a high maintenance drug class that requires the In-Home caregiver to manage the patient and medication- carefully. 







 Virus
Virus Bacteria
Bacteria
 Viruses have a protein coat that surrounds some genes, basically, that’s all. They do not have the biological mechanics to replace themselves or grow. They have to rely on a “living” host cell to do so. Once a virus penetrates the cell, it hijacks the cell's mechanisms and replicates itself continually until the cell dies. The cell then bursts, releasing many more viruses to invade other cells. If they don’t enter a cell, they just sit there doing nothing until the immune system comes along and cleans things up.
Viruses have a protein coat that surrounds some genes, basically, that’s all. They do not have the biological mechanics to replace themselves or grow. They have to rely on a “living” host cell to do so. Once a virus penetrates the cell, it hijacks the cell's mechanisms and replicates itself continually until the cell dies. The cell then bursts, releasing many more viruses to invade other cells. If they don’t enter a cell, they just sit there doing nothing until the immune system comes along and cleans things up.  If viruses aren’t technically alive the immune system cannot technically kill them. What the body does is send out antibodies that recognize the protein sequences in the outer coat. The antibody latches on to the virus and inhibits them from entering a cell and releasing its genes. They also signal other components of the immune system to come along and break up and destroy the virus. By the way that is what vaccines are, antibodies that recognize a certain virus. The important part for you to understand is that you have to catch the virus quickly before it enters a cell and hijacks the cell replication mechanisms. Only then will you stop the infection from spreading.
If viruses aren’t technically alive the immune system cannot technically kill them. What the body does is send out antibodies that recognize the protein sequences in the outer coat. The antibody latches on to the virus and inhibits them from entering a cell and releasing its genes. They also signal other components of the immune system to come along and break up and destroy the virus. By the way that is what vaccines are, antibodies that recognize a certain virus. The important part for you to understand is that you have to catch the virus quickly before it enters a cell and hijacks the cell replication mechanisms. Only then will you stop the infection from spreading. 

 So, after the prescriber hands you the prescription ask if it is an antibiotic. If it is or you recognize the drugs as an antibiotic beforehand it’s time to get pushy again by asking polite questions. I suggest, “Doctor I thought the symptoms were caused by a virus, isn’t there a test where you can use to rule out a viral infection. After all, if it is a virus time is important. By the way, the answer is yes, there are several virus antigens tests. If the doctor still insists on the antibiotic, then go with it and monitor the patient during therapy. If after 3 days the symptoms do not lessen or get worse, it’s time to call the doctor again. Bring up the virus question again or get a second medical opinion depending on how severe the symptoms are becoming. Use tact because you are going to have to work with this guy in the future.
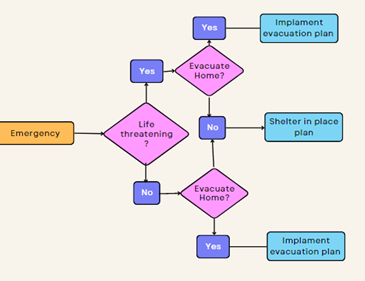
So, after the prescriber hands you the prescription ask if it is an antibiotic. If it is or you recognize the drugs as an antibiotic beforehand it’s time to get pushy again by asking polite questions. I suggest, “Doctor I thought the symptoms were caused by a virus, isn’t there a test where you can use to rule out a viral infection. After all, if it is a virus time is important. By the way, the answer is yes, there are several virus antigens tests. If the doctor still insists on the antibiotic, then go with it and monitor the patient during therapy. If after 3 days the symptoms do not lessen or get worse, it’s time to call the doctor again. Bring up the virus question again or get a second medical opinion depending on how severe the symptoms are becoming. Use tact because you are going to have to work with this guy in the future.  There is a fifth place where skilled In-Home caregivers have to act, monitoring therapy. After two or three days if symptoms are not lessening or getting worse call the doctor. Depending on how severe the symptoms are, you might have to skip the doctor and go to the hospital. Especially in cases of difficulty breathing. Remember the pneumonia thing.
There is a fifth place where skilled In-Home caregivers have to act, monitoring therapy. After two or three days if symptoms are not lessening or getting worse call the doctor. Depending on how severe the symptoms are, you might have to skip the doctor and go to the hospital. Especially in cases of difficulty breathing. Remember the pneumonia thing.
/__opt__aboutcom__coeus__resources__content_migration__serious_eats__seriouseats.com__2019__08__20190819-salt-guide-vicky-wasik16--1500x1125-af406f896440419d8abdead0027a1d04.jpg)
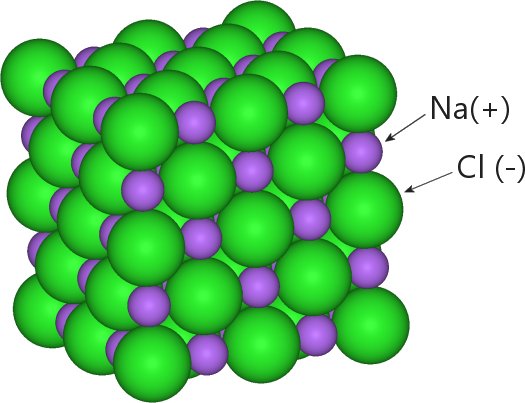 Common table salt is a crystalline compound of sodium and chloride atoms. When chlorine and sodium atoms get together, chlorine takes an electron from the sodium, giving each a charge. Chlorine has a negative charge and sodium gets a positive charge. Like magnets, the opposite charges attract each other, and a uniform crystalline lattice forms.
Common table salt is a crystalline compound of sodium and chloride atoms. When chlorine and sodium atoms get together, chlorine takes an electron from the sodium, giving each a charge. Chlorine has a negative charge and sodium gets a positive charge. Like magnets, the opposite charges attract each other, and a uniform crystalline lattice forms. 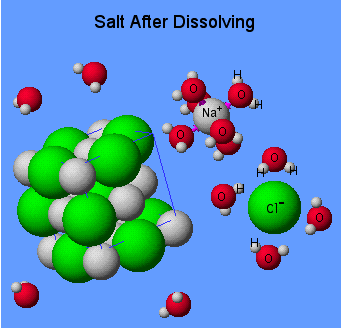

 What can be done to reduce the hidden salt?
What can be done to reduce the hidden salt? Salt from a saltshaker may not be as big a deal as you might have thought but it is an area that still needs to be worked on. The 10% of our salt consumption that comes from a shaker is used to fine-tune the flavor of the foods we eat. At least that is what we tell ourselves. In my years of cooking for a care home, I noticed that the saltshaker was used even before the food was tasted. Often saltshaker use was a habit more than a flavor selection.
Salt from a saltshaker may not be as big a deal as you might have thought but it is an area that still needs to be worked on. The 10% of our salt consumption that comes from a shaker is used to fine-tune the flavor of the foods we eat. At least that is what we tell ourselves. In my years of cooking for a care home, I noticed that the saltshaker was used even before the food was tasted. Often saltshaker use was a habit more than a flavor selection.  There are those who just don’t learn a lesson until they suffer through the consequences of making a mistake. Following instructions, understanding the underlining principle or cooperation is just not their style. One would think that doing things the right way, in the beginning, would be easier but nooo. They feel it would be much easier to be lazy and put much more effort into correcting mistakes later on. Apparently, they just don’t feel successful until they mess up, get caught by government inspectors, and are forced to correct something later on.
There are those who just don’t learn a lesson until they suffer through the consequences of making a mistake. Following instructions, understanding the underlining principle or cooperation is just not their style. One would think that doing things the right way, in the beginning, would be easier but nooo. They feel it would be much easier to be lazy and put much more effort into correcting mistakes later on. Apparently, they just don’t feel successful until they mess up, get caught by government inspectors, and are forced to correct something later on. Initials
Initials

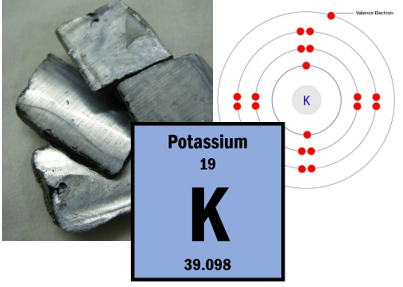
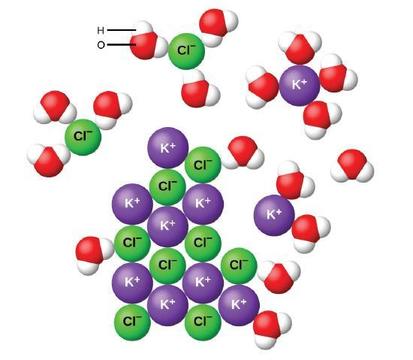 The ion charge also explains why water follows salt. Water molecules have partial magnetic poles. There is a potential weak positive and negative end to each water molecule. Throw in a positive potassium ion (K+) and all the negative ends of the surrounding water molecules will be drawn to it. The more K+ ions the greater the magnetic pull. That magnetic attraction is one of the main driving forces of water flow due to osmosis. If the body wants water to flow past a membrane it pumps salt ions past the membrane and the water naturally follows.
The ion charge also explains why water follows salt. Water molecules have partial magnetic poles. There is a potential weak positive and negative end to each water molecule. Throw in a positive potassium ion (K+) and all the negative ends of the surrounding water molecules will be drawn to it. The more K+ ions the greater the magnetic pull. That magnetic attraction is one of the main driving forces of water flow due to osmosis. If the body wants water to flow past a membrane it pumps salt ions past the membrane and the water naturally follows. 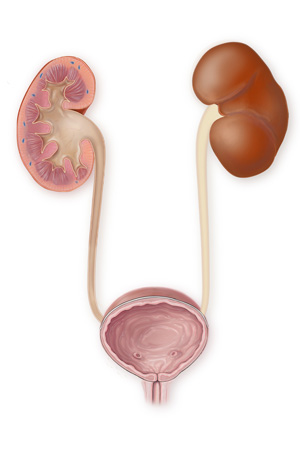

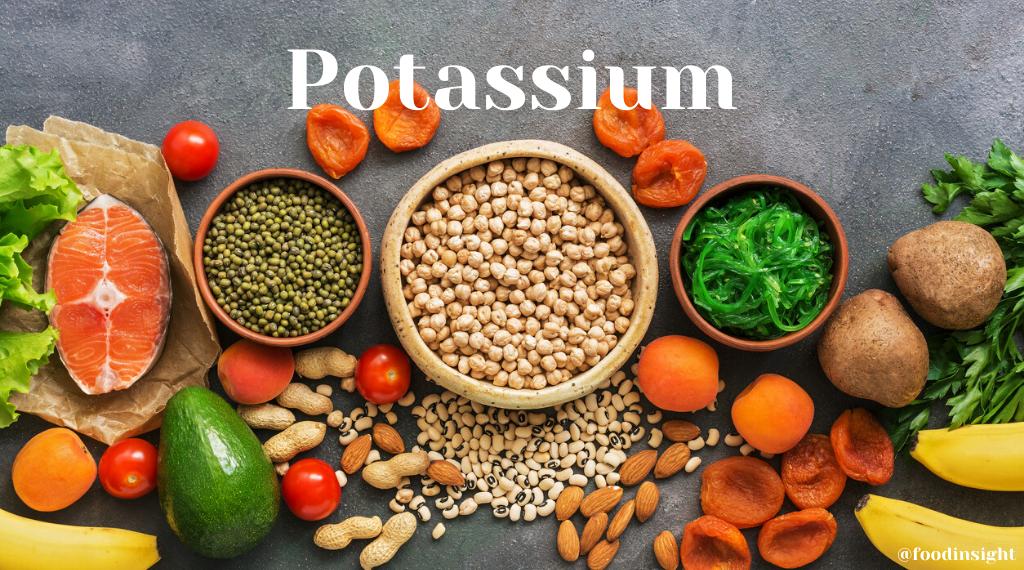
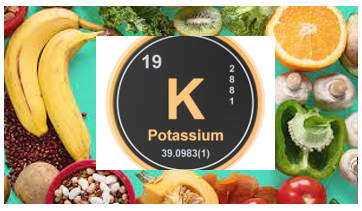
 You might be thinking if potassium is so important why don’t I just go buy an over-the-counter mineral supplement. After all, there has got to be a “pill for every ill”, right? Yes, you can purchase potassium supplements and potassium is added to most multivitamins and other combination supplements. But read the label. You will never find a pill that contains more than 99mg. Why? The National Institute on Health website says the following.
You might be thinking if potassium is so important why don’t I just go buy an over-the-counter mineral supplement. After all, there has got to be a “pill for every ill”, right? Yes, you can purchase potassium supplements and potassium is added to most multivitamins and other combination supplements. But read the label. You will never find a pill that contains more than 99mg. Why? The National Institute on Health website says the following.

