Caregiver Primer on Contact Lenses
Author: Mark Parkinson BsPharm: President AFC-CE
Credit Hours 2- Approximate time required: 120 min.
Educational Goal
Enable caregiver support of residents with contact lenses.
Educational Objective
- Help the care provider to decide whether or not to allow contact use in their homes
- List the reasons why people wear contacts
- Give a basic understanding of the types of contacts in use
- Tell what will be required to maintain the different types of contacts.
- Instruct how to prevent infections and eye damage caused by contact use
- Provide examples of the consequences of not following contact use instructions
Procedure:
Read the course materials. 2. Click on exam portal [Take Exam]. 3. If you have not done so yet fill in Register form (username must be the name you want on your CE certificate). 4. Log in 5. Take exam. 6. Click on [Show Results] when done and follow the instructions that appear. 7. A score of 70% or better is considered passing and a Certificate of Completion will be generated for your records.
Disclaimer
The information presented in this activity is not meant to serve as a guideline for patient management. All procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this article should not be used by care providers without evaluation of their patients’ Doctor. Some conditions and possible contraindications may be of concern. All applicable manufacturers’ product information should be reviewed before use. The author and publisher of this continuing education progra
m have made all reasonable efforts to ensure that all information contained herein is accurate in accordance with the latest available scientific knowledge at the time of acceptance for publication. Nutritional products discussed are not intended for the diagnosis, treatment, cure, or prevention of any disease.
Caregiver Primer on Contact Lens

In-home caregivers are amazing health professionals. With little or no training, they step up to the plate and take care of any and every need their residents have. There is no shirking of responsibility, no passing the buck to another. They just shoulder the responsibility and sees that the job gets done.
One such duty is contact lens care. It does not happen often, but there are times when a resident who wears contact lenses moves into a care home. The care provider suddenly finds themselves having to manage an activity of daily living that most caregivers are ill-prepared for. This course will attempt to prepare the caregiver to move forward with managing this responsibility.
The Reasons for Contacts
 Should a care home allow one of its residents to wear contacts? It is a care-home-policy decision that every care homeowner may have to face. Finding the answer comes from balancing the labor requirement of maintaining the new activity of daily living and the perceived need for contacts. Why does a person wear contacts? Are the reasons worth the extra effort that will be required by the resident and the caregiver?
Should a care home allow one of its residents to wear contacts? It is a care-home-policy decision that every care homeowner may have to face. Finding the answer comes from balancing the labor requirement of maintaining the new activity of daily living and the perceived need for contacts. Why does a person wear contacts? Are the reasons worth the extra effort that will be required by the resident and the caregiver?
Contact lenses, also known as just contacts, are thin lenses made of varying materials that are placed directly on the surface of the eyes. Medically known as ocular prosthetic devices, contacts are worn to correct vision, enhance appearance or for other cosmetic purposes, and to apply a specific medical therapy. Worldwide, over 150 million people wear contacts at least part of the time. The average age of a contact wearer is 31, and two-thirds of all people who wear contacts are women. Each year, $11.7 billion is spent on contacts or contact care products.
Individual reasons for wearing contacts vary from person to person. In addition to correcting vision problems, there are several additional advantages that contacts have over traditional glasses.
They are:
- Aesthetics – contact wearers think they look better without glasses.
- Contacts do not fog up.
- It is easier to wear sunglasses and goggles with contacts.
- Contact lenses move with your eye, allowing a natural field of view.
- Contacts have no frames to obstruct vision and greatly reduce distortions.
- Peripheral vision improves.
- You do not have to reach for or keep track of glasses.
- There are certain eye conditions that are better corrected with contacts.
Caregivers must find out all of the reasons why a resident wears their contacts. They then can better decide if they will allow their use in their home. Here is a gem of advice that comes from my own caregiver experience: Contacts can make a resident feel better about themselves and happy—and content residents are easier to take care of. Don’t underestimate the power of a positive self-image on the tranquility of your home.
The Types of Contacts
Not all contacts are the same. There is a surprising amount of variety in the type of contacts that a resident can wear. Before a decision to allow contacts is made, the caregiver must find out what type of contacts their residents have or will have. The type of contact will determine how much maintenance is involved. Caregivers must understand how and when the contacts are to be used, how they are maintained, and when to replace them.
 The concept of contact lenses to correct vision is centuries old. Leonardo da Vinci first introduced the idea of altering vision by placing a person’s head in a clear glass bowl filled with water. Since then, advances in science, materials, and manufacturing technologies have given us the wide variety of products that are used today. Each type of product has its own purpose and instructions for use. It would be too confusing to discuss each product type. I will simplify matters by reducing the types to just Hard vs Soft contacts and extended ware versus disposable lens.
The concept of contact lenses to correct vision is centuries old. Leonardo da Vinci first introduced the idea of altering vision by placing a person’s head in a clear glass bowl filled with water. Since then, advances in science, materials, and manufacturing technologies have given us the wide variety of products that are used today. Each type of product has its own purpose and instructions for use. It would be too confusing to discuss each product type. I will simplify matters by reducing the types to just Hard vs Soft contacts and extended ware versus disposable lens.
Hard vs. Soft
The first contacts were made of glass and were very uncomfortable to wear. They were replaced by the plastic polymethyl methacrylate (PMMA), also called Plexiglas. These hard contact lenses were more comfortable than glass to wear and gave excellent optics. Unfortunately, they also blocked oxygen from getting to the cornea, which put a limit on contact use. PMMA lenses were replaced by rigid gas-permeable lenses (RGP) made of materials that allowed oxygen to get to where it is needed. This greatly enhanced the wearability of the hard contact lens.
Compared to soft contacts, hard contact lenses are easier to handle, more durable, and less likely to tear. They tend to be less expensive over the life of the lens because they last longer than soft contacts. They are also less likely to have foreign material build up on their surfaces. Initially, hard contacts take longer to get used to wearing than soft contacts. It may take a few weeks to get comfortable wearing RGP lenses, compared to several days for soft contacts. When properly cared for, RGP contacts can last for months to years before they need replacing. Because of their rigid nature, RGP contacts may also be used for other therapeutic effects.

By far, the most common type of contacts that caregivers will encounter will be soft contacts. In the United States, about 76 percent of all contact lens prescriptions are for soft contacts. They are preferred because of their comfort and ease of use. Soft contacts are made out of soft flexible plastics, also called hydrogels. They are flexible enough to conform to the surface of the cornea, making them more comfortable to wear. Newer hydrogels incorporate silicone, which permits even more oxygen to reach the cells of the eye. This allows for extended periods of contact use.
Daily vs. Extended vs. Continuous
While we’re awake, the eye is exposed to enough oxygen to allow contact use without any problems. But at night, when the eyes are closed, the gas permeability factor of the contact becomes much more critical. Without enough oxygen reaching the eye, optic cells can die, causing ulcers on the surface of the eye to form.
There are three basic categories of contacts, based on their oxygen permeability:
- Daily wear —used while awake and must be removed during periods of sleep, including long naps, unless approved by the doctor.
- Extended wear — can be worn overnight, usually for seven days consecutively without removal.
- Continuous wear — can be worn for up to 30 consecutive nights, the maximum amount of time allowed by the FDA.

Replacement Schedule
No matter the type of contacts the resident has, they will eventually need to be replaced. For various reasons, contacts only last so long and need to be exchanged with a new pair. Hard contacts last the longest, while some disposable soft contacts are designed to be replaced on a daily basis. Each type has its advantages. As far as the caregiver is concerned, the longer the replacement schedule, the more important the lens care maintenance instructions become. Each set of contacts will come with instructions detailing when to best replace the old lenses with new. If the instructions are missing, contact the eye doctor for advice.
|
In general:
- Daily disposable lenses — discard after a single day of wear
- Disposable lenses — discard every two to four weeks
- Frequent replacement lenses — discard monthly or quarterly
- RGP lenses — discard every six months or longer
- PMMA — can last for five years or more
|
 |
Caregiver note: Daily disposable contacts require no maintenance because they are thrown out after one use. Those contacts that must be removed nightly and stored away for the next day’s use are the most labor-intensive lenses. Which contacts are chosen is a balancing act between cost, ability of the resident to handle the contact, and your willingness to be responsible for supervising the extra maintenance steps.
How to Use Contacts
A resident who has contacts will have been taught how to use them by the doctor. Whether the resident follows those instructions is a different matter. Even the most cooperative patient can pick up bad habits. The Centers for Disease  Control and Prevention (CDC) reports “Between 40%-90% of contact lens wearers do not properly follow the care instructions for their contact lenses. Approximately 99% of respondents reported at least one contact lens hygiene behavior previously associated with an increased risk of eye infection or inflammation.”
Control and Prevention (CDC) reports “Between 40%-90% of contact lens wearers do not properly follow the care instructions for their contact lenses. Approximately 99% of respondents reported at least one contact lens hygiene behavior previously associated with an increased risk of eye infection or inflammation.”
As a caregiver, you are not in a position to teach or advise the resident on proper contact use. But you can question the resident by asking if that was how the doctor initially taught them to use their prescription. You can also monitor and report any difficulties or abnormalities to the eye doctor. It is also your responsibility to ensure that the appropriate supplies are always handy. I recommend that you read the written material that came with the contacts and compare that with what you observe.
General instructions for use are:
Applying
- Wash hands (but don’t use soaps that have added oils or fragrances as they can stick to the surface of the lens)
- Gently shake the lens storage case to loosen the contact lens if it is sticking to the container. Carefully slide the lens into your hand. Use your fingertips (not your nails) to handle the lens.
- Fully rinse the lens with contact lens solution. Do not use tap water to rinse the lens.
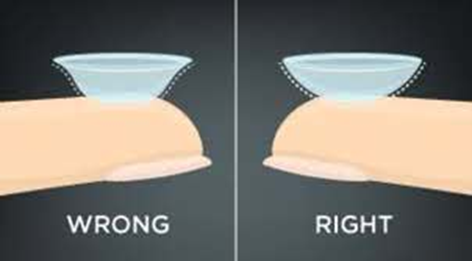
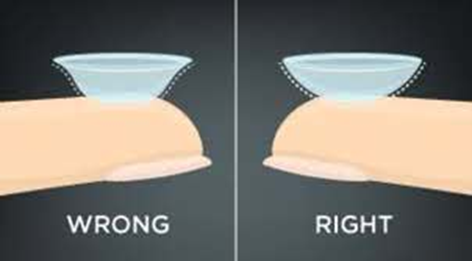 Place the contact lens on the tip of your pointer (index) or middle finger of your dominant hand (the hand you write with). Look closely at the lens to check for torn or damaged areas. Also, make sure the lens is right-side out. If the lens forms a bowl and the edges turn up, it is ready to be placed on the eye. If the lens looks like a lid (edges turn out), it needs to be reversed.
Place the contact lens on the tip of your pointer (index) or middle finger of your dominant hand (the hand you write with). Look closely at the lens to check for torn or damaged areas. Also, make sure the lens is right-side out. If the lens forms a bowl and the edges turn up, it is ready to be placed on the eye. If the lens looks like a lid (edges turn out), it needs to be reversed.- Hold your upper eyelid open with your other (non-dominant) hand while looking in the mirror. Hold down your lower eyelid with your middle or ring finger of the dominant hand (whichever finger is not holding the contact lens). Or, you may also use your thumb and fingers of your non-dominant hand to open your upper and lower eyelids very wide instead.
- Place the lens on your eye. You can look in front of you or up toward the ceiling while putting the lens in.
- Close your eyes slowly and roll them in a full circle to help settle the lens properly in place. You may also gently massage your closed eyelid. Then open your eyes and gently blink a few times. Look in a mirror to see if the lens is centered on your eye.
Source: https://www.aao.org/eye-health/glasses-contacts/how-to-put-in-contact-lenses
Removing
First, wash and dry your hands before removing any lenses. To take out soft lenses, pull down your lower lid. Look up or to the side, and gently move your lens to the white of your eye. Using your thumb and index finger, gently pinch the lens and lift it off your eye. For gas-permeable lenses, open your eyes wide and pull the skin near the corner of your eye toward your ear. Bend over your open palm and blink. The lens should pop out into your palm.
Source: https://www.allaboutvision.com/contacts/contact-lens-tips.htm
Notes for the Caregiver
- The kind of soap you supply to the contact wearer matters. The soap and all of its ingredients must be able to rinse off completely. The rule of thumb is that if you can smell a scent or feel a lotion after rinsing, that substance will
 stick to the surface of the contact and cause problems.
stick to the surface of the contact and cause problems.
- Fingernail hygiene matters to contact wearers. Help your resident keep their fingernails trimmed and clean.
- Towel hygiene also matters to contact wearers. Ensure that there is always a lint-free, clean towel handy to dry the hands.
- Encourage the contact wearer to inspect the contacts closely before putting them into the eye. If the contact feels uncomfortable after it is inserted, remove it and rinse the contact with the appropriate solution. If the contact continues to be uncomfortable, you inspect the contact for damage and the eye for inflammation. If the problem continues or if there are signs of infection or an allergic response, have the resident use their regular glasses. Then get the resident to the eye doctor.
Show and Tell
There are those who follow instructions better if they are shown what to do. You can ask for suggested video links from the doctor or view the following videos. I like these because it is an actual eye doctor putting in real contacts into his own eyes. Consider watching these videos as part of this course.
For those who are not computer savvy, click on the link to watch the video. If the video replaces this lesson screen, after you are done watching the video, click on the back arrow—usually it will be in the top left-hand corner. It will bring you to come back to this course. Or you can simply reload the course from afc-ce.com.
Inserting: https://www.youtube.com/watch?v=wlPyYkq3LnY
Removing: https://www.youtube.com/watch?v=kq2WRc99on4
The Care of Contacts
Our eyes are very delicate tissues. In order to survive in our germ-infested and dirt-clogged world, our eyes have a very impressive array of protective mechanisms. Improperly cared-for contact lenses can compromise those defenses and can lead to damaged eye tissues. Once the tissue has been damaged, germs, single-cell parasites, and other such nasties can invade and grow into a full-blown infection very quickly.
To prevent such damaging outcomes, the patient will have been given a set of instructions on how to take care of the lenses. But as contact lenses are a medical device, caregivers are responsible for ensuring that contact care instructions are followed. To help you more effectively monitor these activities, let us discuss some important concepts of lens care. Here is another video to get us started on explaining how to take care of contacts.
https://www.youtube.com/watch?v=CaeSkPAykkU
Monitoring Concept 1 – Comfort
After the resident has gotten used to wearing contacts, discomfort is an important warning sign that something is wrong. Inspection should follow. If no obvious cause is evident, have the resident wear glasses and contact the doctor. It might just be that the eyes are fatigued and need a break from contact use, but you should let the doctor decide that. If it is just a matter of dry eyes causing the discomfort, get a prescription for a dry-eye relief product. Don’t forget to have a doctor’s “permission to self-medicate” order on file.
Monitoring Concept 2 – Cleaning and Disinfecting
General Instructions for Reusable Soft Contact Lenses:
The Contacts
Protein in the resident’s tears or foreign material from the environment can adhere to the lens and build up over time. This film can compromise the eye’s defenses and cause irritation. To prevent film buildup, do the following.
- Before removing the contacts from the eyes, fill each chamber of the case with “fresh” contact lens disinfecting solution. Do not top off old solution.
- Remove contacts from the eyes, one lens at a time. Place the lens in the clean, dry palm of your hand, and apply a few drops of your contact lens disinfecting solution. With one finger, gently rub the lens back and forth on your palm to clean the lens surfaces.
- After rubbing each side of the lens, rinse them completely with more solution. Then place the lens into your clean contact lens case.
- Repeat the procedure for the next lens. Close the case lids and leave your lenses to soak overnight.
The Contact Case
 When not being used, store the lenses in the contact lens case provided with the product.
When not being used, store the lenses in the contact lens case provided with the product.- After removing the lenses from the case, empty the case and clean it as directed. It might be as simple as pouring out the solution, placing the case upside down, and then letting it air dry.
- Infection-causing biofilms can build up on lens cases. They should be replaced as recommended, usually every three months. When in doubt, replace it.
- Use only the approved solutions to clean the case.
Monitoring Concept 3 – Using Solutions Correctly
Contact lenses are made out of specialized materials that require specialized cleaning and care solutions. These solutions are designed to accomplish many tasks all at once and so are called contact care systems. The two most commonly used soft contact lens care systems are based on a multipurpose solution and a hydrogen peroxide solution.
Multi-purpose solution
Multi-purpose solutions are a combination of products that, clean, rinse, disinfect, and store contact lenses with one product. They are generally considered easier to use with fewer safety concerns than hydrogen peroxide systems. Their ease of use and low cost have made them the most commonly used product for lens care. Unfortunately, there are those who develop allergies or other sensitivities to one or more of the ingredients and require a hydrogen peroxide-based system.
Hydrogen peroxide solution
Hydrogen peroxide (HP) is a very reactive chemical that disrupts the bonding of other materials. It cleans off materials sticking to the surface of lenses and kills infectious organisms. Over time, the HP solution breaks down and changes into a normal saline solution. It is safe to store the lens in and will not harm the eye tissue. HP systems contain  materials that speed up the breakdown process, neutralizing the solution sooner. Even with these materials, it will take about four to six hours before the HP is completely neutralized. To avoid accidently putting HP solutions into the eye, each bottle comes with a red warning tip.
materials that speed up the breakdown process, neutralizing the solution sooner. Even with these materials, it will take about four to six hours before the HP is completely neutralized. To avoid accidently putting HP solutions into the eye, each bottle comes with a red warning tip.
If the resident still accidently puts HP into their eye or experiences stinging or burning when they insert the contact lens, remove the contact and flush the eye with a sterile saline solution. If an HP system is used, caregivers should store a bottle of sterile saline solution in their first-aid kit. If, after rinsing, the eye is still painful, call or get the resident to the doctor. Eye damage from HP is usually not permanent.
HP solutions degrade and lose potency over time. Multi-purpose solutions become less effective and saline solution becomes less sterile with time. Caregivers need to discard and replace these products as recommended by the manufacturer.
Other solutions that the caregiver may encounter are:
- Daily Cleaners – Daily cleaners are used only to loosen materials from the contact lenses. Other products, such as multi-purpose solutions, are needed to rinse and disinfect the lenses before they are stored in the contact lens case.
- Enzymatic Protein Removers – EPRs are an additional product used to remove the biofilm that collects on lenses. They are supplied in solution or tablet form and are used either on a daily or weekly basis.
General Instructions for Hard Contact Lenses:
 Hard contacts and rigid gas-permeable contacts are custom-made for the patient and require their own maintenance systems. Hard contact care systems usually require several different solutions for wetting, cleaning, and disinfecting. Though these steps may be similar to those for soft contacts, caregivers need to familiarize themselves with the specific requirements as supplied by the hard contact manufacturer. If the written material is lost, contact the eye doctor. Do not rely upon the memory of the resident. Except for sterile saline solutions, hard contact solutions cannot be used for soft contacts.
Hard contacts and rigid gas-permeable contacts are custom-made for the patient and require their own maintenance systems. Hard contact care systems usually require several different solutions for wetting, cleaning, and disinfecting. Though these steps may be similar to those for soft contacts, caregivers need to familiarize themselves with the specific requirements as supplied by the hard contact manufacturer. If the written material is lost, contact the eye doctor. Do not rely upon the memory of the resident. Except for sterile saline solutions, hard contact solutions cannot be used for soft contacts.
Notes for Caregivers
- Residents with contacts are required to see the eye doctor more often. Question the resident on when they last saw their eye doctor. Keep track of future appointments in their files.
 Continually monitor contact use. Watch for these common failings:
Continually monitor contact use. Watch for these common failings:
- inadequate handwashing
- non-prescribed overnight wear (accidental or intentional)
- excessive duration of extended wear
- excessive lens replacement interval
- inadequate case cleaning
- failure to use correct disinfecting solution (e.g., no disinfection or stored in tap water)
- failure to rub and rinse lenses
- topping off solution (e.g., not replacing with fresh solution for each storage occasion)
- Monitor resident’s eyes for:
- Dry eyes
- Irritated, red eyes
- Worsening pain in or around the eyes
- Light sensitivity
- Sudden blurry vision
- Unusually watery eyes
- Goopy or crusty eyes
- Brands matter in contact solution selection. Even generic versions may not be compatible with newer versions of contact lenses. Consult with the eye doctor if you are presented with a new brand of eye-care product.
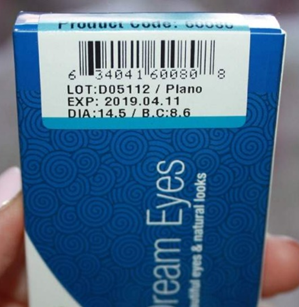
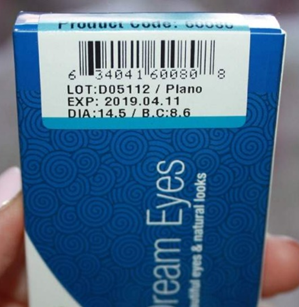
- Expiration dates matter in contact care products. Take note of the expiration date on the container and replace outdated products.
- Other eye-care products and eye medications may not be suitable with contacts. Get the advice and approval of the eye doctor before using any of these products. Do not rely on the pharmacist in these cases. Their knowledge may not be deep enough in these areas.
- Contacts can be stored in their cases only for a limited time before having to disinfect them again. If you are storing the contacts multiple times or for long periods, it might be wiser to switch to daily disposables. The following timeframes are based on tightly closed lids. Consult the instructional materials for product-specific times.
- Multipurpose solution – Up to 1 month.
- Gas permeable solutions – Up to 1 month
- Hydrogen peroxide – Up to 1 week, but as short as 24 hours
- If contacts are dropped and land on the ground, it is safer to sanitize the contacts before using them again. It might require the resident using their regular glasses while they wait.
 Never use tap water with anything contact-related. That includes swimming, pools, bathing, and showers. Infectious material in tap water that usually causes no problems can be become a significant health threat in contact use.
Never use tap water with anything contact-related. That includes swimming, pools, bathing, and showers. Infectious material in tap water that usually causes no problems can be become a significant health threat in contact use.
The Dangers of Improper Contact Use
The following patient cases, along with an accompanying video, can be found at the CDC website. https://www.cdc.gov/contactlenses/videos.html. The videos are not part of the course, but I do recommend watching them.
Ryan’s Story—Water and Contacts Don’t Mix
Alabama football player Ryan first noticed a painful problem with his left eye on his way to a championship game. He had a habit of rinsing his contact lenses in water if he didn’t have disinfecting solution. Ryan was diagnosed with Acanthamoeba keratitis, an infection caused by an organism that lives in water. He now has a scar in his eye that makes it difficult to see and will eventually need to have a major eye procedure to correct his vision.
Te’s Story—Don’t Sleep in Contacts
Te’ had been wearing contacts for about 14 years and would sometimes sleep in her lenses for up to two weeks at a time. On her wedding day, she woke up with a painful corneal infection and had severe vision loss within 24 hours. Te’ is still recovering and advises others to properly clean their contacts and not to sleep in them.
Whitney’s Story: Keep Water Away from Contacts
After wearing contact lenses for over 20 years, freelance writer, and mom of three teens Whitney was diagnosed with Acanthamoeba keratitis in 2015. She temporarily lost all vision in her left eye for several months. Looking back, her best guess is that the infection was caused by water that got on her lenses when she showered in her contacts. Whitney is back to wearing contacts and advises other contact lens wearers to practice healthy wear and care habits.
Patient Story: Jim
After improperly storing his contact lenses, Jim got an eye infection that led to severe vision loss in one eye. He waited for two years before he was able to get a corneal transplant to repair the damaged eye.
Conclusion
 For 150 million people, contact lenses are a preferred way of seeing the world more clearly. They are willing to take on the responsibilities that are involved in maintaining their contacts. If one of those patients moves into your care home, those responsibilities are now your responsibility to monitor. By constant communication with the eye doctor, reading the instructional material, and ensuring the resident follows the doctor’s orders and adheres to the product’s instructions, the caregiver can ensure the proper and safe use of contact lenses by their residents.
For 150 million people, contact lenses are a preferred way of seeing the world more clearly. They are willing to take on the responsibilities that are involved in maintaining their contacts. If one of those patients moves into your care home, those responsibilities are now your responsibility to monitor. By constant communication with the eye doctor, reading the instructional material, and ensuring the resident follows the doctor’s orders and adheres to the product’s instructions, the caregiver can ensure the proper and safe use of contact lenses by their residents.
As always, good luck in your caregiving efforts.
Mark Parkinson, BS Pharm
References:
Contact Lens Care. AOA.org. American Optometric Association. 2020
https://www.aoa.org/healthy-eyes/vision-and-vision-correction/contact-lens-care?sso=y
Kelsey Giara, PharmD. Contact Lenses: Choosing the Right Solutions. Power-Pak CE. UAN: 0430-0000-20-110-H01-P. Sep 30, 2020.
https://www.powerpak.com/course/preamble/120275
Healthy Contact Lens Wear and Care. Center for Disease Control and Prevention. 2020
https://www.cdc.gov/contactlenses/index.html
Contact lens. Wikipedia. 2020
https://en.wikipedia.org/wiki/Contact_lens
Types of Contact Lenses. AOA.org. American Optometric Association. 2020.
https://www.aoa.org/healthy-eyes/vision-and-vision-correction/types-of-contact-lenses?sso=y
Here’s Why Hydrogen Peroxide is an Excellent Contact Lens Solution. Berryessa Optometry. Nov 26, 2019
https://www.berryessaoptometry.com/2019/11/26/hydrogen-peroxide-contact-lens-solution-2019/
Types of Contact Lenses. US FDA Food and Drug Administration. Jan 16 2018
https://www.fda.gov/medical-devices/contact-lenses/types-contact-lenses#plano
Cleaning Your Contacts. Acuvue.com. 2020
https://www.acuvue.com/wear-and-care/contact-lens-cleaning-and-care
Caregiver Primer on Contact Lenses
Author: Mark Parkinson BsPharm: President AFC-CE
Credit Hours 2- Approximate time required: 120 min.
Educational Goal
Enable caregiver support of residents with contact lenses.
Educational Objective
- Help the care provider to decide whether or not to allow contact use in their homes
- List the reasons why people wear contacts
- Give a basic understanding of the types of contacts in use
- Tell what will be required to maintain the different types of contacts.
- Instruct how to prevent infections and eye damage caused by contact use
- Provide examples of the consequences of not following contact use instructions
Procedure:
Read the course materials. 2. Click on exam portal [Take Exam]. 3. If you have not done so yet fill in Register form (username must be the name you want on your CE certificate). 4. Log in 5. Take exam. 6. Click on [Show Results] when done and follow the instructions that appear. 7. A score of 70% or better is considered passing and a Certificate of Completion will be generated for your records.
Disclaimer
The information presented in this activity is not meant to serve as a guideline for patient management. All procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this article should not be used by care providers without evaluation of their patients’ Doctor. Some conditions and possible contraindications may be of concern. All applicable manufacturers’ product information should be reviewed before use. The author and publisher of this continuing education program have made all reasonable efforts to ensure that all information contained herein is accurate in accordance with the latest available scientific knowledge at the time of acceptance for publication. Nutritional products discussed are not intended for the diagnosis, treatment, cure, or prevention of any disease.
Caregiver Primer on Contact Lens
In-home caregivers are amazing health professionals. With little or no training, they step up to the plate and take care of any and every need their residents have. There is no shirking of responsibility, no passing the buck to another. They just shoulder the responsibility and sees that the job gets done.
One such duty is contact lens care. It does not happen often, but there are times when a resident who wears contact lenses moves into a care home. The care provider suddenly finds themselves having to manage an activity of daily living that most caregivers are ill-prepared for. This course will attempt to prepare the caregiver to move forward with managing this responsibility.
The Reasons for Contacts
Should a care home allow one of its residents to wear contacts? It is a care-home-policy decision that every care homeowner may have to face. Finding the answer comes from balancing the labor requirement of maintaining the new activity of daily living and the perceived need for contacts. Why does a person wear contacts? Are the reasons worth the extra effort that will be required by the resident and the caregiver?
Contact lenses, also known as just contacts, are thin lenses made of varying materials that are placed directly on the surface of the eyes. Medically known as ocular prosthetic devices, contacts are worn to correct vision, enhance appearance or for other cosmetic purposes, and to apply a specific medical therapy. Worldwide, over 150 million people wear contacts at least part of the time. The average age of a contact wearer is 31, and two-thirds of all people who wear contacts are women. Each year, $11.7 billion is spent on contacts or contact care products.
Individual reasons for wearing contacts vary from person to person. In addition to correcting vision problems, there are several additional advantages that contacts have over traditional glasses.
They are:
- Aesthetics – contact wearers think they look better without glasses.
- Contacts do not fog up.
- It is easier to wear sunglasses and goggles with contacts.
- Contact lenses move with your eye, allowing a natural field of view.
- Contacts have no frames to obstruct vision and greatly reduce distortions.
- Peripheral vision improves.
- You do not have to reach for or keep track of glasses.
- There are certain eye conditions that are better corrected with contacts.
Caregivers must find out all of the reasons why a resident wears their contacts. They then can better decide if they will allow their use in their home. Here is a gem of advice that comes from my own caregiver experience: Contacts can make a resident feel better about themselves and happy—and content residents are easier to take care of. Don’t underestimate the power of a positive self-image on the tranquility of your home.
The Types of Contacts
Not all contacts are the same. There is a surprising amount of variety in the type of contacts that a resident can wear. Before a decision to allow contacts is made, the caregiver must find out what type of contacts their residents have or will have. The type of contact will determine how much maintenance is involved. Caregivers must understand how and when the contacts are to be used, how they are maintained, and when to replace them.
The concept of contact lenses to correct vision is centuries old. Leonardo da Vinci first introduced the idea of altering vision by placing a person’s head in a clear glass bowl filled with water. Since then, advances in science, materials, and manufacturing technologies have given us the wide variety of products that are used today. Each type of product has its own purpose and instructions for use. It would be too confusing to discuss each product type. I will simplify matters by reducing the types to just Hard vs Soft contacts and extended ware versus disposable lens.
Hard vs. Soft
The first contacts were made of glass and were very uncomfortable to wear. They were replaced by the plastic polymethyl methacrylate (PMMA), also called Plexiglas. These hard contact lenses were more comfortable than glass to wear and gave excellent optics. Unfortunately, they also blocked oxygen from getting to the cornea, which put a limit on contact use. PMMA lenses were replaced by rigid gas-permeable lenses (RGP) made of materials that allowed oxygen to get to where it is needed. This greatly enhanced the wearability of the hard contact lens.
Compared to soft contacts, hard contact lenses are easier to handle, more durable, and less likely to tear. They tend to be less expensive over the life of the lens because they last longer than soft contacts. They are also less likely to have foreign material build up on their surfaces. Initially, hard contacts take longer to get used to wearing than soft contacts. It may take a few weeks to get comfortable wearing RGP lenses, compared to several days for soft contacts. When properly cared for, RGP contacts can last for months to years before they need replacing. Because of their rigid nature, RGP contacts may also be used for other therapeutic effects.
By far, the most common type of contacts that caregivers will encounter will be soft contacts. In the United States, about 76 percent of all contact lens prescriptions are for soft contacts. They are preferred because of their comfort and ease of use. Soft contacts are made out of soft flexible plastics, also called hydrogels. They are flexible enough to conform to the surface of the cornea, making them more comfortable to wear. Newer hydrogels incorporate silicone, which permits even more oxygen to reach the cells of the eye. This allows for extended periods of contact use.
Daily vs. Extended vs. Continuous
While we’re awake, the eye is exposed to enough oxygen to allow contact use without any problems. But at night, when the eyes are closed, the gas permeability factor of the contact becomes much more critical. Without enough oxygen reaching the eye, optic cells can die, causing ulcers on the surface of the eye to form.
There are three basic categories of contacts, based on their oxygen permeability:
- Daily wear —used while awake and must be removed during periods of sleep, including long naps, unless approved by the doctor.
- Extended wear — can be worn overnight, usually for seven days consecutively without removal.
- Continuous wear — can be worn for up to 30 consecutive nights, the maximum amount of time allowed by the FDA.
Replacement Schedule
No matter the type of contacts the resident has, they will eventually need to be replaced. For various reasons, contacts only last so long and need to be exchanged with a new pair. Hard contacts last the longest, while some disposable soft contacts are designed to be replaced on a daily basis. Each type has its advantages. As far as the caregiver is concerned, the longer the replacement schedule, the more important the lens care maintenance instructions become. Each set of contacts will come with instructions detailing when to best replace the old lenses with new. If the instructions are missing, contact the eye doctor for advice.
In general:
- Daily disposable lenses — discard after a single day of wear
- Disposable lenses — discard every two to four weeks
- Frequent replacement lenses — discard monthly or quarterly
- RGP lenses — discard every six months or longer
- PMMA — can last for five years or more
Caregiver note: Daily disposable contacts require no maintenance because they are thrown out after one use. Those contacts that must be removed nightly and stored away for the next day’s use are the most labor-intensive lenses. Which contacts are chosen is a balancing act between cost, ability of the resident to handle the contact, and your willingness to be responsible for supervising the extra maintenance steps.
How to Use Contacts
A resident who has contacts will have been taught how to use them by the doctor. Whether the resident follows those instructions is a different matter. Even the most cooperative patient can pick up bad habits. The Centers for Disease Control and Prevention (CDC) reports “Between 40%-90% of contact lens wearers do not properly follow the care instructions for their contact lenses. Approximately 99% of respondents reported at least one contact lens hygiene behavior previously associated with an increased risk of eye infection or inflammation.”
As a caregiver, you are not in a position to teach or advise the resident on proper contact use. But you can question the resident by asking if that was how the doctor initially taught them to use their prescription. You can also monitor and report any difficulties or abnormalities to the eye doctor. It is also your responsibility to ensure that the appropriate supplies are always handy. I recommend that you read the written material that came with the contacts and compare that with what you observe.
General instructions for use are:
Applying
- Wash hands (but don’t use soaps that have added oils or fragrances as they can stick to the surface of the lens)
- Gently shake the lens storage case to loosen the contact lens if it is sticking to the container. Carefully slide the lens into your hand. Use your fingertips (not your nails) to handle the lens.
- Fully rinse the lens with contact lens solution. Do not use tap water to rinse the lens.
- Place the contact lens on the tip of your pointer (index) or middle finger of your dominant hand (the hand you write with). Look closely at the lens to check for torn or damaged areas. Also, make sure the lens is right-side out. If the lens forms a bowl and the edges turn up, it is ready to be placed on the eye. If the lens looks like a lid (edges turn out), it needs to be reversed.
- Hold your upper eyelid open with your other (non-dominant) hand while looking in the mirror. Hold down your lower eyelid with your middle or ring finger of the dominant hand (whichever finger is not holding the contact lens). Or, you may also use your thumb and fingers of your non-dominant hand to open your upper and lower eyelids very wide instead.
- Place the lens on your eye. You can look in front of you or up toward the ceiling while putting the lens in.
- Close your eyes slowly and roll them in a full circle to help settle the lens properly in place. You may also gently massage your closed eyelid. Then open your eyes and gently blink a few times. Look in a mirror to see if the lens is centered on your eye.
Source: https://www.aao.org/eye-health/glasses-contacts/how-to-put-in-contact-lenses
Removing
First, wash and dry your hands before removing any lenses. To take out soft lenses, pull down your lower lid. Look up or to the side, and gently move your lens to the white of your eye. Using your thumb and index finger, gently pinch the lens and lift it off your eye. For gas-permeable lenses, open your eyes wide and pull the skin near the corner of your eye toward your ear. Bend over your open palm and blink. The lens should pop out into your palm.
Source: https://www.allaboutvision.com/contacts/contact-lens-tips.htm
Notes for the Caregiver
- The kind of soap you supply to the contact wearer matters. The soap and all of its ingredients must be able to rinse off completely. The rule of thumb is that if you can smell a scent or feel a lotion after rinsing, that substance will stick to the surface of the contact and cause problems.
- Fingernail hygiene matters to contact wearers. Help your resident keep their fingernails trimmed and clean.
- Towel hygiene also matters to contact wearers. Ensure that there is always a lint-free, clean towel handy to dry the hands.
- Encourage the contact wearer to inspect the contacts closely before putting them into the eye. If the contact feels uncomfortable after it is inserted, remove it and rinse the contact with the appropriate solution. If the contact continues to be uncomfortable, you inspect the contact for damage and the eye for inflammation. If the problem continues or if there are signs of infection or an allergic response, have the resident use their regular glasses. Then get the resident to the eye doctor.
Show and Tell
There are those who follow instructions better if they are shown what to do. You can ask for suggested video links from the doctor or view the following videos. I like these because it is an actual eye doctor putting in real contacts into his own eyes. Consider watching these videos as part of this course.
For those who are not computer savvy, click on the link to watch the video. If the video replaces this lesson screen, after you are done watching the video, click on the back arrow—usually it will be in the top left-hand corner. It will bring you to come back to this course. Or you can simply reload the course from afc-ce.com.
Inserting: https://www.youtube.com/watch?v=wlPyYkq3LnY
Removing: https://www.youtube.com/watch?v=kq2WRc99on4
The Care of Contacts
Our eyes are very delicate tissues. In order to survive in our germ-infested and dirt-clogged world, our eyes have a very impressive array of protective mechanisms. Improperly cared-for contact lenses can compromise those defenses and can lead to damaged eye tissues. Once the tissue has been damaged, germs, single-cell parasites, and other such nasties can invade and grow into a full-blown infection very quickly.
To prevent such damaging outcomes, the patient will have been given a set of instructions on how to take care of the lenses. But as contact lenses are a medical device, caregivers are responsible for ensuring that contact care instructions are followed. To help you more effectively monitor these activities, let us discuss some important concepts of lens care. Here is another video to get us started on explaining how to take care of contacts.
https://www.youtube.com/watch?v=CaeSkPAykkU
Monitoring Concept 2 – Cleaning and Disinfecting
General Instructions for Reusable Soft Contact Lenses:
The Contacts
Protein in the resident’s tears or foreign material from the environment can adhere to the lens and build up over time. This film can compromise the eye’s defenses and cause irritation. To prevent film buildup, do the following.
- Before removing the contacts from the eyes, fill each chamber of the case with “fresh” contact lens disinfecting solution. Do not top off old solution.
- Remove contacts from the eyes, one lens at a time. Place the lens in the clean, dry palm of your hand, and apply a few drops of your contact lens disinfecting solution. With one finger, gently rub the lens back and forth on your palm to clean the lens surfaces.
- After rubbing each side of the lens, rinse them completely with more solution. Then place the lens into your clean contact lens case.
- Repeat the procedure for the next lens. Close the case lids and leave your lenses to soak overnight.
The Contact Case
- When not being used, store the lenses in the contact lens case provided with the product.
- After removing the lenses from the case, empty the case and clean it as directed. It might be as simple as pouring out the solution, placing the case upside down, and then letting it air dry.
- Infection-causing biofilms can build up on lens cases. They should be replaced as recommended, usually every three months. When in doubt, replace it.
- Use only the approved solutions to clean the case.
Monitoring Concept 3 – Using Solutions Correctly
Contact lenses are made out of specialized materials that require specialized cleaning and care solutions. These solutions are designed to accomplish many tasks all at once and so are called contact care systems. The two most commonly used soft contact lens care systems are based on a multipurpose solution and a hydrogen peroxide solution.
Multi-purpose solution
Multi-purpose solutions are a combination of products that, clean, rinse, disinfect, and store contact lenses with one product. They are generally considered easier to use with fewer safety concerns than hydrogen peroxide systems. Their ease of use and low cost have made them the most commonly used product for lens care. Unfortunately, there are those who develop allergies or other sensitivities to one or more of the ingredients and require a hydrogen peroxide-based system.
Hydrogen peroxide solution
Hydrogen peroxide (HP) is a very reactive chemical that disrupts the bonding of other materials. It cleans off materials sticking to the surface of lenses and kills infectious organisms. Over time, the HP solution breaks down and changes into a normal saline solution. It is safe to store the lens in and will not harm the eye tissue. HP systems contain materials that speed up the breakdown process, neutralizing the solution sooner. Even with these materials, it will take about four to six hours before the HP is completely neutralized. To avoid accidently putting HP solutions into the eye, each bottle comes with a red warning tip.
If the resident still accidently puts HP into their eye or experiences stinging or burning when they insert the contact lens, remove the contact and flush the eye with a sterile saline solution. If an HP system is used, caregivers should store a bottle of sterile saline solution in their first-aid kit. If, after rinsing, the eye is still painful, call or get the resident to the doctor. Eye damage from HP is usually not permanent.
HP solutions degrade and lose potency over time. Multi-purpose solutions become less effective and saline solution becomes less sterile with time. Caregivers need to discard and replace these products as recommended by the manufacturer.
Other solutions that the caregiver may encounter are:
- Daily Cleaners – Daily cleaners are used only to loosen materials from the contact lenses. Other products, such as multi-purpose solutions, are needed to rinse and disinfect the lenses before they are stored in the contact lens case.
- Enzymatic Protein Removers – EPRs are an additional product used to remove the biofilm that collects on lenses. They are supplied in solution or tablet form and are used either on a daily or weekly basis.
General Instructions for Hard Contact Lenses:
Hard contacts and rigid gas-permeable contacts are custom-made for the patient and require their own maintenance systems. Hard contact care systems usually require several different solutions for wetting, cleaning, and disinfecting. Though these steps may be similar to those for soft contacts, caregivers need to familiarize themselves with the specific requirements as supplied by the hard contact manufacturer. If the written material is lost, contact the eye doctor. Do not rely upon the memory of the resident. Except for sterile saline solutions, hard contact solutions cannot be used for soft contacts.
Notes for Caregivers
- Residents with contacts are required to see the eye doctor more often. Question the resident on when they last saw their eye doctor. Keep track of future appointments in their files.
- Continually monitor contact use. Watch for these common failings:
- inadequate handwashing
- non-prescribed overnight wear (accidental or intentional)
- excessive duration of extended wear
- excessive lens replacement interval
- inadequate case cleaning
- failure to use correct disinfecting solution (e.g., no disinfection or stored in tap water)
- failure to rub and rinse lenses
- topping off solution (e.g., not replacing with fresh solution for each storage occasion)
- Monitor resident’s eyes for:
- Dry eyes
- Irritated, red eyes
- Worsening pain in or around the eyes
- Light sensitivity
- Sudden blurry vision
- Unusually watery eyes
- Goopy or crusty eyes
- Brands matter in contact solution selection. Even generic versions may not be compatible with newer versions of contact lenses. Consult with the eye doctor if you are presented with a new brand of eye-care product.
- Expiration dates matter in contact care products. Take note of the expiration date on the container and replace outdated products.
- Other eye-care products and eye medications may not be suitable with contacts. Get the advice and approval of the eye doctor before using any of these products. Do not rely on the pharmacist in these cases. Their knowledge may not be deep enough in these areas.
- Contacts can be stored in their cases only for a limited time before having to disinfect them again. If you are storing the contacts multiple times or for long periods, it might be wiser to switch to daily disposables. The following timeframes are based on tightly closed lids. Consult the instructional materials for product-specific times.
- Multipurpose solution – Up to 1 month.
- Gas permeable solutions – Up to 1 month
- Hydrogen peroxide – Up to 1 week, but as short as 24 hours
- If contacts are dropped and land on the ground, it is safer to sanitize the contacts before using them again. It might require the resident using their regular glasses while they wait.
- Never use tap water with anything contact-related. That includes swimming, pools, bathing, and showers. Infectious material in tap water that usually causes no problems can be become a significant health threat in contact use.
The Dangers of Improper Contact Use
The following patient cases, along with an accompanying video, can be found at the CDC website. https://www.cdc.gov/contactlenses/videos.html. The videos are not part of the course, but I do recommend watching them.
Ryan’s Story—Water and Contacts Don’t Mix
Alabama football player Ryan first noticed a painful problem with his left eye on his way to a championship game. He had a habit of rinsing his contact lenses in water if he didn’t have disinfecting solution. Ryan was diagnosed with Acanthamoeba keratitis, an infection caused by an organism that lives in water. He now has a scar in his eye that makes it difficult to see and will eventually need to have a major eye procedure to correct his vision.
Te’s Story—Don’t Sleep in Contacts
Te’ had been wearing contacts for about 14 years and would sometimes sleep in her lenses for up to two weeks at a time. On her wedding day, she woke up with a painful corneal infection and had severe vision loss within 24 hours. Te’ is still recovering and advises others to properly clean their contacts and not to sleep in them.
Whitney’s Story: Keep Water Away from Contacts
After wearing contact lenses for over 20 years, freelance writer, and mom of three teens Whitney was diagnosed with Acanthamoeba keratitis in 2015. She temporarily lost all vision in her left eye for several months. Looking back, her best guess is that the infection was caused by water that got on her lenses when she showered in her contacts. Whitney is back to wearing contacts and advises other contact lens wearers to practice healthy wear and care habits.
Patient Story: Jim
After improperly storing his contact lenses, Jim got an eye infection that led to severe vision loss in one eye. He waited for two years before he was able to get a corneal transplant to repair the damaged eye.
Conclusion
For 150 million people, contact lenses are a preferred way of seeing the world more clearly. They are willing to take on the responsibilities that are involved in maintaining their contacts. If one of those patients moves into your care home, those responsibilities are now your responsibility to monitor. By constant communication with the eye doctor, reading the instructional material, and ensuring the resident follows the doctor’s orders and adheres to the product’s instructions, the caregiver can ensure the proper and safe use of contact lenses by their residents.
As always, good luck in your caregiving efforts.
Mark Parkinson, BS Pharm
References:
Contact Lens Care. AOA.org. American Optometric Association. 2020 https://www.aoa.org/healthy-eyes/vision-and-vision-correction/contact-lens-care?sso=y
Kelsey Giara, PharmD. Contact Lenses: Choosing the Right Solutions. Power-Pak CE. UAN: 0430-0000-20-110-H01-P. Sep 30, 2020.
https://www.powerpak.com/course/preamble/120275
Healthy Contact Lens Wear and Care. Center for Disease Control and Prevention. 2020 https://www.cdc.gov/contactlenses/index.html
Contact lens. Wikipedia. 2020 https://en.wikipedia.org/wiki/Contact_lens
Types of Contact Lenses. AOA.org. American Optometric Association. 2020. https://www.aoa.org/healthy-eyes/vision-and-vision-correction/types-of-contact-lenses?sso=y
Here’s Why Hydrogen Peroxide is an Excellent Contact Lens Solution. Berryessa Optometry. Nov 26, 2019
https://www.berryessaoptometry.com/2019/11/26/hydrogen-peroxide-contact-lens-solution-2019/
Types of Contact Lenses. US FDA Food and Drug Administration. Jan 16 2018 https://www.fda.gov/medical-devices/contact-lenses/types-contact-lenses#plano
Cleaning Your Contacts. Acuvue.com. 2020 https://www.acuvue.com/wear-and-care/contact-lens-cleaning-and-care
Exam Portal
click on [Take Exam]
Purchase membership here to unlock Exam Portal.
*Important*
Registration and login is required to place your name on your CE Certificates and access your certificate history.
Username MUST be how you want your name on your CE Certificate.
 What vitamins really are is a group of powerful chemical compounds— synthetically produced or derived from the foods we consume—that have the following properties:
What vitamins really are is a group of powerful chemical compounds— synthetically produced or derived from the foods we consume—that have the following properties: own before 1910. The ability to identify minute chemical compounds in the body just did not exist. Then, in Japan, and later, in England, a group of chemicals was discovered that seemed to be vital for maintaining good health. Kazimierz Funk, a Polish biochemist working in London, described them as vital-amines (amines are compounds containing nitrogen). Publications later shortened the name to vitamines. The term was soon used to describe other chemical compounds that were essential for good health. Instead of giving the chemical name, writers found it was easier to call them vitamine A, B, C, and so forth. The name vitamine was used even when there was no amine group in the compound. For clarity, the name was shortened to simply vitamin. As our biochemistry knowledge grew, further adjustments to the naming systems had to occur. For example, folic acid was originally called vitamin M. Then it was reclassified to vitamin B9. Vitamin G (riboflavin) become Vitamin B2, and so forth. The word vitamin soon made its way into advertising and popular culture. What was once a shortcut name for medical writers became the word that everyone used.
own before 1910. The ability to identify minute chemical compounds in the body just did not exist. Then, in Japan, and later, in England, a group of chemicals was discovered that seemed to be vital for maintaining good health. Kazimierz Funk, a Polish biochemist working in London, described them as vital-amines (amines are compounds containing nitrogen). Publications later shortened the name to vitamines. The term was soon used to describe other chemical compounds that were essential for good health. Instead of giving the chemical name, writers found it was easier to call them vitamine A, B, C, and so forth. The name vitamine was used even when there was no amine group in the compound. For clarity, the name was shortened to simply vitamin. As our biochemistry knowledge grew, further adjustments to the naming systems had to occur. For example, folic acid was originally called vitamin M. Then it was reclassified to vitamin B9. Vitamin G (riboflavin) become Vitamin B2, and so forth. The word vitamin soon made its way into advertising and popular culture. What was once a shortcut name for medical writers became the word that everyone used. Vitamins are biochemical compounds that are involved in multiple chemical processes throughout the body. They provide vital components that enable chemical processes to occur. They do not provide energy; they enable us to more efficiently get energy from the foods we eat. They don’t make strong bones; they enable our body to make strong bones. They do not provide immunity; they enable the body to protect itself.
Vitamins are biochemical compounds that are involved in multiple chemical processes throughout the body. They provide vital components that enable chemical processes to occur. They do not provide energy; they enable us to more efficiently get energy from the foods we eat. They don’t make strong bones; they enable our body to make strong bones. They do not provide immunity; they enable the body to protect itself. Chemical reactions occur when compounds come into contact with each other. The greater the concentrations of compounds, the more reactions occur. It is an automatic occurrence, and they happen even if we don’t want them to. For example, vitamin C is an antioxidant used in our immune system, but it can also create kidney stones. Taking too much vitamin C, for some people, will cause very painful problems.
Chemical reactions occur when compounds come into contact with each other. The greater the concentrations of compounds, the more reactions occur. It is an automatic occurrence, and they happen even if we don’t want them to. For example, vitamin C is an antioxidant used in our immune system, but it can also create kidney stones. Taking too much vitamin C, for some people, will cause very painful problems. Economically speaking, naturally produced vitamins usually cost more. This is partly due to advertising hype. People are fooled into thinking that “natural” means better so they will pay more for the product. The main reason for the extra cost comes from the fact that it takes a lot more effort to produce naturally sourced vitamins. You have to harvest the food source, isolate the parts that have the vitamin compound, remove the vitamin, concentrate its supply, and then package it in a consumable form. It’s ironic that naturally sourced vitamins require so many unnatural processes.
Economically speaking, naturally produced vitamins usually cost more. This is partly due to advertising hype. People are fooled into thinking that “natural” means better so they will pay more for the product. The main reason for the extra cost comes from the fact that it takes a lot more effort to produce naturally sourced vitamins. You have to harvest the food source, isolate the parts that have the vitamin compound, remove the vitamin, concentrate its supply, and then package it in a consumable form. It’s ironic that naturally sourced vitamins require so many unnatural processes.